With over 1 million incidence cases and more than 780,000 deaths in 2018, gastric cancer (GC) was ranked as the 5th most common cancer and the 3rd leading cause of cancer deaths worldwide. Though several biomarkers, including carcinoembryonic antigen (CEA), cancer antigen 19-9 (CA19-9), and cancer antigen 72-4 (CA72-4), have been identified, their diagnostic accuracies were modest. Circulating tumor cells (CTCs), cells derived from tumors and present in body fluids, have recently emerged as promising biomarkers, diagnostically and prognostically, of cancers, including GC. In this review, we present the landscape of CTCs from migration, to the presence in circulation, biologic properties, and morphologic heterogeneities. We evaluated clinical implications of CTCs in GC patients, including diagnosis, prognosis, and therapeutic management, as well as their application in immunotherapy.
- circulating tumor cells
- gastric cancer
- diagnostic
- prognostic
- treatment
Note: The following contents are extract from your paper. The entry will be online only after author check and submit it.
1. Introduction
2. Landscape of CTCs
2.1. CTC Migration
2.2. CTCs in Circulation
2.3. Morphologic Heterogeneity of CTCs
3. Clinical Implication of CTCs in GC
| Author, Country, Year | Cases | Isolation and Identification Tool | Markers | OS and PFS of CTC(+) vs. CTC(-) | Positive Cutoff | Clinical Implications | Reference |
|---|---|---|---|---|---|---|---|
| Lee (South Korea), 2015 |
100 metastatic GC patients | anti-EpCAM antibody coated magnetic particles CTC-Profiler (Veridex) | EpCAM, CK8/18/19, CD45 | OS: 120 days vs. 220 days; p = 0.03) PFS: 59 days vs. 141 days; p = 0.004 |
≥ 5CTCs/7.5 mL | CTCs are associated with poor response to chemotherapy in metastatic gastric cancer patients. CTC positivity was an independent adverse factor for PFS and OS. |
[55] |
| Okabe (Japan), 2016 |
136 advanced GC patients | semi-automated immunomagnetic separation system CellSearch | EpCAM, CK8/18/19CD45, DAPI | OS: HR 2.20 [95%CI: 1.120–4.03]; p = 0.009 PFS: HR 2.03 [95%CI: 1.13–3.66]; p = 0.016 | ≥ 1 CTCs/7.5 mL | Detection of CTCs was an independent predictor of a shorter PFS in advanced gastric cancer. Patients who require intensive treatment: CTCs could be a valuable biomarker. The combined status of CTC and CY would be useful in selecting patients for radical surgery. |
[56] |
| Zhou 2016 |
1110 GC patients in meta-analysis | - | - | OS: HR = 2.23, 95% CI: 1.86–2.66 PFS: HR = 2.02, 95% CI: 1.36–2.99 |
- | High CTCs count was associated with depth of infiltration regional lymph nodes metastasis and distant metastasis. For un-resectable GC patients, high CTCs count before and during chemotherapy was significantly correlated with poor OS, PFS, and DC rate. |
[57] |
| Mishima(Japan), 2017 | 101 GC patients 15 advanced GC patients whose primary tumors were HER2-, but CTCs were HER2+ |
both 3 D-IF-FISH method & CellSearch System3D-IF-FISH only | EpCAM, CK8/18/19, CD45 HER2 |
OS and PFS of 15 advanced GC patients with CTC- HER2+: 6.1 months (95% CI: 2.1–10.0) and 14.4 months (11.0–17.8), respectively | ≥ 1 CTCs/7.5 mL | New, non-invasive strategy to select patients who are likely to benefit from trastuzumab-based therapies, despite their primary biopsy being HER2-negative. | [58] |
| Liu (China), 2017 | 59 GC patients of stage II-IV | CELLection™ Epithelial Enrich kit | EpCAM, CK8/18/19, DAPI | OS: HR = 3.59, 95% CI:1.655-7.817, p = 0.001 PFS: = 2.81, 95% CI:1.313-5.999, p = 0.008 |
≥ 2 CTCs/5 mL | The baseline CTC count of >2 cells/5 mL and an increase of the CTC count after the first cycle of chemotherapy was an independent prognostic marker of poor PFS and OS→ patients with a low baseline CTC count or decrease of the CTC count after the first cycle of chemotherapy may benefit significantly from palliative chemotherapy | [59] |
| Zheng (China), 2017 |
81 GC patients | ISET-immunofluorescence | CK8/18/19, vimentin | CTM positivity was an independent factor for determining the PFS (p = 0.016) and OS (p = 0.003) of stage IV patients CTM correlated with shorter PFS and OS than single CTCs (p < 0.05) |
≥ 1 CTCs/5 mL For CTM: ≥ 3 CTCs |
In stage IV patients, CTM positivity was correlated with serum CA125 level. CTM were an independent predictor of shorter PFS and OS in stage IV patients. → CTM detection may be a useful tool to predict prognosis in stage IV patients. | [60] |
| Kang (South Korea), 2017 |
116 patients with gastric cancer patients & 31 healthy volunteers | “FAST disc” centrifugal microfluidic system | EpCAM, CK8/18/19, CD45 DAPI |
- | ≥ 2 CTCs/7.5 mL Sensitivity: 85.3 Specificity: 90.3 |
Although the clinical feasibility of CTCs for gastric cancer staging was not proved, these results suggest a potential role of CTCs as an early diagnostic biomarker of gastric cancer. | [61] |
| Yue (China), 2018 | 35 patients with different advanced gastrointestinal tumors | Pep MNPs isolated system |
CK19, CD45 DAPI, PD-L1 | PFS based on baseline PD-L1high CTC count: 4.27 vs. 2.07 months HR = 3.342; 95%CI 1.488–7.505; p= 0.002 PFS based on post-therapeutic PD-L1high CTC count: 3.4 vs. 2.1 months; HR= 0.412; 95%CI 0.177–0.962;, p= 0.031) |
≥ 2 PD-L1high CTCs/4 mL | The abundance of PD-L1high CTCs at baseline might serve as a predictor to screen patients for PD-1/PD-L1 blockade therapies. Measuring the dynamic changes of CTC could indicate the therapeutic response at early time. |
[62] |
| Yang (China), 2018 |
40 GC patients | wedge-shaped microfluidic chip (CTC-ΔChip) & three-color immunocytochemistry method | (CK, CD45, Nucleus marker | - | - | CTC-ΔChip exhibited the feasibility of detecting CTCs from different types of solid tumor, and it identified 7.30 ± 7.29 CTCs from 2 mL peripheral blood with a positive rate of 75% (30/40) in GC patients. Novel CTC-ΔChip shows high performance for detecting CTCs from less volume of blood samples of cancer patients and important clinical significance in GC. |
[63] |
| Li (China), 2018 | 115 advanced GC patients, including 56 tumor HER2+ subjects who received first-line HER2-targeted therapy plus chemotherapy and 59 tumor HER2− subjects who received chemotherapy alone | IF-FISH Cytelligen system | DAPI, HER2, CEP8, and CD45 | - | - | CTC HER2+ was found in 91.0% of tumor HER2+ and 76.2% tumor HER2− patients and was correlated with development of resistance to trastuzumab for the tumor HER2+ patients and chemotherapy alone for the tumor HER2− patients. Determining of CTC HER2 showed advantages in real-time monitoring of therapeutic resistance. |
[64] |
| Cheng (China), 2019 | 32 advanced GC patients | CanPatrol CTC enrichment technique Multiplex RNA in situ hybridization assay |
EpCAM, CK8/18/19, CD45 DAPI, PD-L1, Vimentin and Twist |
- | ≥ 2 PD-L1+ CTCs/5 mL | CTCs count was well correlated with clinicopathology parameters. Enumeration of epithelial CTC subset and its relative abundance in the total CTC pool are highly correlated with clinical efficacy. Monitoring CTC subtypes exhibits higher sensitivity of evaluating the disease status, compared to the traditional methods. |
[65] |
| Lu (China), 2019 |
42 GC patients of stage III-IV | ISET-ICC method followed by IHC | EpCAM, CK8/18/19, CD45, Vimentin and Twist, E-cadherin |
- | - | The threshold number of CTCs is significantly associated with different clinical stages and was positively correlated with the value in U/mL of CA724. CTCs technology based on ISET method has a high detection rate. CTCs are promising predictor for the evaluation and prediction of treatment responses in stage III–IV gastric cancer. |
[66] |
| Abdallah (Brazil), 2019 |
At diagnosis (55 samples before neoadjuvant treatment) After surgery and before adjuvant therapy (33 samples) |
ISET and immunocytochemistry & microscopy | HER2 and plakoglobin, CD45 | -PFS between CTM-positive patients vs. CTM-negative patients (18.7 months vs. 21.6 months; p = 0.258 -PFS between plakoglobin-positive CTM patients vs. plakoglobin-positive CTM patients: 15.9 months vs. 21.3 months; p= 0.114 |
≥ 1 CTM (2 CTCs)/4 mL | The analysis of CTM plakoglobin expression is a promising tool in the understanding the biology and prognosis of GC. | [67] |
| Gao, 2019 | 3814 GC patients in meta-analysis | - | - | HR = 1.84, 95%CI 1.50–2.26, p < 0.001 | - | CTC positivity was associated with poorer OS. | [68] |
3.1. Diagnostic Potential of CTC in GC
3.2. CTC Assay for Prognosis and Treatment Management of GC
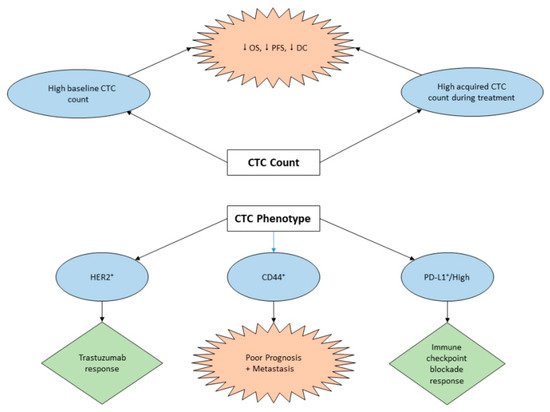
3.3. The Role of CTCs in GC Immunotherapy
This entry is adapted from the peer-reviewed paper 10.3390/cancers12030695
