Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Medical Informatics
Feedback is an effective pedagogy aimed to create cognitive dissonance and reinforce learning as a key component of clinical training programs. Pharmacy learners receive constant feedback. However, there is limited understanding of how feedback is utilized in pharmacy education.
- feedback
- pharmacy education
1. Introduction
Feedback has been identified as a critical component of clinical training programs [1]. It has been described as “the heart of medical education” [2] and “the cornerstone of effective clinical training” [3]. The Accreditation Council for Pharmacy Education highlights the importance of the provision of feedback in both didactic and experiential curricula, requiring formative performance feedback to students in both settings [4]. Additionally, the American Society of Health-System Pharmacists describes feedback as “essential for residents’ skill development” and requires verbal formative feedback by Standard 3.4 in their guidance document for postgraduate year-one pharmacy residency program accreditation standards [5].
Feedback has been proposed to play a critical role at the center of adult learning theory and is among the most influential moderator of learning [6][7]. The main roles of feedback are to identify and minimize student dissonance and reinforce correct learning for consolidation into existing knowledge and skill development. Feedback can have many effects in addition to confirming the accuracy of a student including increasing student effort and motivation to engage in learning, exposing different methods of understanding to the student, and conveying progress toward a student’s goal. While feedback has been shown to be one of the most powerful tools in the teaching arsenal, a meta-analysis reported that one-third of feedback had a negative impact on achievement, possibly due to person-focused feedback as opposed to process or task-oriented feedback [8]. This highlights the critical, yet variable impact feedback can have on learning [6].
Pharmacy learners are constantly being provided feedback from various sources including faculty, standardized patients, preceptors, and peers throughout their education. This feedback is also delivered to students in many forms including written, verbal, and automatic response devices. Most of the discussion involving feedback within the health professions education literature, however, is described in other disciplines, primarily medicine [9]. Although pharmacy learners were incorporated in a prior scoping review of feedback in medical education, the number of publications regarding feedback to pharmacy learners has increased and it has not been evaluated broadly within the pharmacy education literature [9]. The purpose of this scoping review was to identify the breadth and depth of evidence regarding the use of feedback for learning in pharmacy education and training and identify potential gaps which could lead to future research.
2. Study Selections
Figure 1 shows the PRISMA flow chart for article inclusion. Overall, 64 citations were included for analysis in this review from around the world encompassing Bachelor (BPharm), Master (MPharm), and Doctor of Pharmacy (PharmD) programs spanning four curricular settings: didactic, objective structured clinical examination (OSCE), experiential, and co-curriculum (Table 2) (see Supplementary Tables S2–S5 for full data extraction). Feedback was provided for a variety of topics including communication, patient work up, and career/interview preparation through written, verbal, or multimodal (written and verbal) means (Table 3).
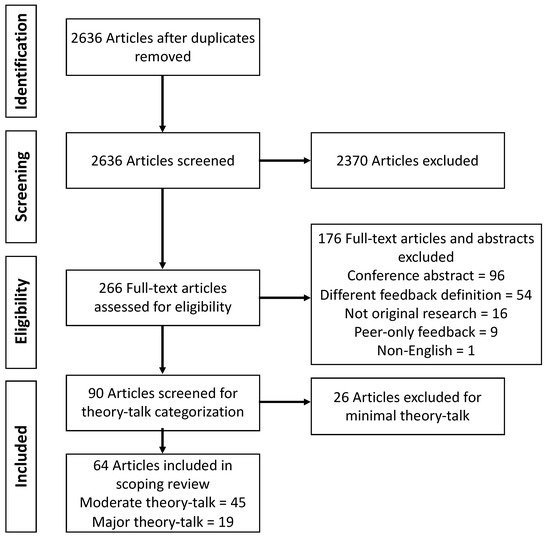
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for scoping review search strategy.
3. Didactic Studies
Over half of the included studies focused on feedback given in didactic settings. These 36 studies include 24 moderate theory talk while 12 were categorized as major theory talk. They span the didactic curricular setting, including students from the first to final years of Bachelor (BPharm), Master (MPharm), and Doctor of Pharmacy (PharmD) programs, and range in study size from 18 to 621 participants. Most of the studies in this setting provided written feedback, while smaller percentages provided verbal or multimodal feedback (Table 3).
The moderate theory talk articles examined new didactic courses and course interventions, and included feedback on student performance within their design, but did not assess the given feedback for quality or impact. Overall, as a group, these papers did not focus on feedback as a key study objective or outcome; only four studies included feedback in their study objectives, but no aspect of the feedback provided was included for analysis [10][11][12][13]. These four papers tested the use of feedback in three different areas: improving CPR skills development [10]; subjective, objective, assessment, and plan (SOAP) note writing [11]; and student performance on verbal competency and patient counseling and interviewing assessments [12][13]. The other studies’ feedback focus areas were patient communication including counseling and other simulated patient interactions [14][15][16][17][18]; patient work up including SOAP notes [14][19][20][21][22][23][24] or oral case presentations and care plans [22][25][26][27]; and other topics such as evidence appraisal and research skills [28][29]; self-assessments [30]; disease information [31]; pharmacy calculations [32]; and pharmacology experiments [33].
Eleven of the 12 major theory talk articles assessed the impact of feedback on student learning. Seven articles evaluated the impact of a singular method of delivering feedback [audio-verbal [34][35], objective rubric [36], online (n = 90 s and third-year PharmD (P2-P3) and 410 first-year PharmD (P1) students over 5 years) [37][38], or written (n = 133 fifth-year BPharm students and 150 MPharm) [39][40] on learning whereas four articles compared multiple methods of delivery including online vs. handwritten (n = 169 first-year MPharm and 201 P3) [41][42], verbal vs. written (350 P2-P3) [43], and audio-verbal vs. written (n = 75 P1) [44]. Only one major theory talk article evaluated the quality of feedback provided, comparing peer to faculty feedback (n = 182 fourth-year BPharm) [45].
Audio-verbal feedback and the use of an objective rubric resulted in positive outcomes with respect to compression depth in 120 “novice” learners, and all compression and ventilation outcomes for 104 “novice” learners during CPR training [34][35] and SOAP note grading and standardized patient checklist over successive cases for 126 P3 students [36], respectively. Studies evaluating online feedback yielded varying results on feedback’s impact on learning; one study found it promoted improvements on future SOAP notes [37], while another found mixed results as significant grade improvements occurred between two cohorts, but four cohorts had no difference [38]. One study found students engaging with written feedback as part of problem-based learning significantly increased laboratory practical grades [39]. Similarly, another study saw an increase in student pre- and post-course patient work-up scores [40]. Some evidence suggests that written online feedback was more timely than written paper feedback [42] while audio-verbal feedback took 1.5 times longer than written [44]. However, in terms of amount of feedback, praise and error identification, and personability, more feedback was provided through audio-verbal and online than paper [41][44]. Alternatively, the role of multimodal feedback in improving student problem-solving skills compared to a singular delivery method or no feedback at all was demonstrated [43]. Finally, peer assessment resulted in higher grades than experts. However, there was no difference in the quality of feedback provided [45].
4. Objective Structured Clinical Examination/Simulation Studies
There were seven articles (five moderate theory talk and two major theory talk) related to OSCE or simulation activities and all but one included learners in the later years of the pharmacy curriculum. One moderate theory talk article described the development and design of a formative and summative OSCE program across the entire curriculum [46]. All five moderate theory talk studies in a simulation or OSCE training environment incorporated immediate verbal [47][48][49] written [46], or multimodal [50] feedback into their methodology.
One major theory talk article sought to compare immediate versus delayed feedback after a patient counseling simulation for 153 P3 students. While the trainees preferred the immediate feedback, overall grades did not differ between immediate and delayed feedback [51]. Learner satisfaction and feedback preferences of 20 final year MPharm students was compared with three scenario simulation modalities [45]. The paper-based simulation had feedback provided immediately in the form of model answers to written questions and a small group discussion. The computer-based simulation incorporated feedback immediately after completing the game as a detailed scorecard. For the simulated patient, a video recording of the role-play was provided to the students along with their score and feedback using a guide the day after the experience [52].
5. Experiential Studies
Twelve of the included studies focused on feedback given in experiential settings including seven moderate theory talk [53][54][55][56][57][58][59] and five major theory talk [60][61][62][63][64]. All articles included learners in the final year of their pharmacy program ranging from 13 to 162 participants. Two articles compared early learners or post-graduate trainees to learners in the final year of the program [54][56]. Most of the studies provided multimodal feedback while the remainder provided written feedback only (Table 3).
The moderate theory talk articles primarily examined feedback on learner communication through patient medication history and counseling [54][58] or motivational interviewing [53], patient work up via simulated patient case scenarios [56][57], or student knowledge of pharmaceutical calculations [55]. One article focused feedback to residents on their provision of feedback to students [59]. The primary format for feedback in these studies was multimodal [53][54][55][56] while other studies provided only written [57] or verbal feedback [58][59]; however, none of the studies examined the direct impact of feedback on learning.
In contrast, the four major theory talk articles directly assessed learner feedback using multimodal [62] or written only approaches [60][61][63]. These studies examined feedback as it relates to students’ patient counselling skills, problem solving, clinical care (assessment/plan), evidenced-based medicine application, professionalism, communication, effective student self-reflections, and SOAP note writing. In all major theory talk studies, student performance (knowledge or abilities) was improved as a result of the feedback [60][61][62][63]. Feedback increased student scores across three SOAP notes after written feedback was provided to 54 fourth-year PharmD (P4) students. In addition, there was positive correlation between SOAP note performance and advanced pharmacy practice experience (APPE) grade [60]. The impact of feedback on student achievement of curricular outcomes (patient-centered assessment and plan, evidence-based medicine application, professionalism, and communication) was evaluated in another study of 149 students by utilizing faculty feedback to students. Ninety-seven percent of students in their APPE year demonstrated achievement of these ability-based outcomes [61]. Another study showed communication and counseling skills of 45 fourth-year BPharm students were significantly improved over three sessions as a result of both verbal and video recorded feedback compared to no feedback [62]. Another evaluation demonstrated that, among 34 students, providing feedback on reflective responses during an ambulatory care APPE led to more “reflective” responses (intervention) as compared to less “reflective” responses when no feedback was given (control) [63]. A final study assessed SOAP note performance finding that 128 P4 students performed better on a second SOAP note after written feedback in all sections. However, semester of APPE had no effect on performance [64].
6. Co-Curriculum Studies
Finally, nine studies included feedback within the co-curricular space, all of which were moderate theory talk [65][66][67][68][69][70][71][72][73]. Five studies provided only written feedback [65][69][71][72][73] while three studies provided multimodal feedback [66][67][70], and one study provided only verbal feedback [68]. The focus of most publications was related to preparing final year students in obtaining a residency or employment through mock interview practice, curriculum vitae development, and related activities [65][67][68][69][70][74] while two focused on student reflections [71][72], and one incorporated feedback into a student portfolio activities [73]. No study evaluated the quality or impact of feedback provided, only reporting student perceptions on the feedback they received. Although three studies included more than 100 participants [70][71][73], samples sizes in individual studies were generally small ranging from 9–39 participants [65][66][67][68][69][72].
7. Identified Gaps
Several gaps have been revealed from this scoping review. First, documentation and evaluation of the quality of feedback is largely absent in the pharmacy education literature as only 1 of 64 included studies assessed the quality of feedback provided. However, this study evaluated feedback quality to compare faculty comments to peer comments, finding no difference in quality of feedback between faculty and peer [45]. Second, as mentioned above, the impact and effectiveness of the various feedback interventions on student learning and performance is largely unknown as authors tend to focus on student perception data. In addition, few studies have assessed the use of feedback in the post-graduate setting. No studies included trainees in fellowship programs and only four of 64 (6.25%) included learners in clinical training programs. There are also areas to explore feedback within interprofessional education as only one major theory talk article included multidisciplinary learners and two moderate theory talk articles evaluated pharmacy and either neuroscience or advanced practice nursing students. No articles assessed pharmacy and other health profession learners. Finally, given that only professional development and student reflection skills were studied in the co-curricular setting, and the impact of feedback was not included, there are numerous opportunities for in depth research as well as a broader scope of research in this area. The use and role of feedback in both patient care and non-patient care activities including public health outreach and education events, interprofessional education, leadership development, and cultural competency is still largely unknown.
8. Discussion
This scoping review summarizes what has been published about feedback as it relates to information written or verbally communicated to a learner from a teacher/preceptor that is intended to modify the learner’s thinking or behavior for the purpose of improving learning in pharmacy education. Importantly, from the initial search it is clear that “feedback” is a very broadly used term as only 10% of identified articles met criteria for full-text review. Furthermore, of those that underwent full-text review, 20.3% used “feedback” to describe an intervention or program different than how this review defined “feedback,” warranting exclusion from analysis.
The breadth of feedback utilized throughout pharmacy education and training around the world is wide reaching. The 64 included articles span the entirety of pharmacy education from first programmatic year of Bachelor, Masters, and Doctor of Pharmacy programs to postgraduate year two residency programs. The majority of these studies came from the United States and focused on students in the didactic years/courses of their curriculum while 12 articles studied feedback in the experiential curriculum including three articles that included postgraduate training. There are also several ways that feedback was provided to learners including written and verbal, or a combination of both. The areas in which feedback was focused also encompasses many key elements of pharmacy training. Articles from didactic, OSCE, and experiential curricular settings focused on similar topics including communication and patient work up. The co-curricular setting, however, focused exclusively on professional development in the form of career/interview preparation or reflection, primarily for final year students seeking residency training. Didactic articles primarily included written feedback whereas multimodal feedback was more common in OSCE, experiential, and co-curricular settings. This is likely due to the fact that didactic courses typically have larger student to feedback provider ratio compared to the other settings making verbal feedback less feasible compared to OSCE or experiential settings. It is worth noting, however, the relatively few articles of feedback during OSCEs given its effectiveness in this environment [75].
The included articles in this review demonstrate the relative paucity of utilization and impact of feedback within the pharmacy education literature. Much of what is known about feedback and how to provide feedback in pharmacy, dental, and medical education is based on little to no high-quality evidence, thus evidence-based recommendations are lacking [9][76]. A recent systematic review of feedback within nursing education, however, found quality feedback as described by students to be timely, incorporate positive and constructive comments, be directly related to the content, linguistically clear, and feed forward or justify a grade [77]. Importantly, studies which included an assessment of student performance all found positive impact from their educational interventions although evidence suggests that up to one-third of feedback can have a negative effect [8]. This may be due to feedback rarely being the sole intervention or publication bias. Although this review did not intend to assess the quality of included articles, the small number of articles which not only described how feedback was incorporated in the educational intervention, but also assessed its impact on student learning is astonishing. Only 19 of the 90 (21.1%) articles screened for theory talk analysis met major theory talk criteria where feedback was not only included in the educational design, but its use was also analyzed as part of the study. Therefore, feedback appears to more commonly be an aspect of an educational intervention but has rarely been assessed for impact, effect size, or quality. In addition to the lack of feedback assessment, most of the analyzed articles in the experiential and co-curricular settings had relatively small sample sizes, especially compared to feedback in the didactic or OSCE settings. This may be due to the fact that not every learner will take the same experiential rotation and many of the co-curricular studies were primarily voluntary and consisted of students seeking residency training, possibly limiting generalizability pharmacy learners at large. Finally, while articles seeking only to evaluate student perception of feedback were excluded, contrary to their main objective, results often focused on student perception data as opposed to the impact, effectiveness, or quality of the feedback intervention in concordance with their stated objectives, further limiting the depth of feedback literature.
There are some notable limitations to this review. First, the used definition of “feedback” may have resulted in an overly narrow group of included articles which was further limited through applying theory talk analysis due to potential author bias. Given the common use, range of definitions of feedback, and large number of articles initially identified in the initial database search, however, this review was specifically designed to describe feedback from an educator to a learner. In addition, all articles underwent independent review by two authors with a third author resolving any conflicts to maintain objectivity. However, data extraction was not confirmed by a second author, so varying results are possible if different or additional investigators were involved in thematic analysis. This subgroup of articles was also limited to only articles written in English. Only one article was excluded for this reason, however, which increases confidence in the search strategy for a complete evaluation of the breadth and depth of feedback related literature.
This entry is adapted from the peer-reviewed paper 10.3390/pharmacy9020091
References
- Grover, B.; Hayes, B.D.; Watson, K. Feedback in Clinical Pharmacy Education. Am. J. Health-Syst. Pharm. 2014, 71, 1592–1596.
- Branch, W.T.; Paranjape, A. Feedback and Reflection: Teaching Methods for Clinical Settings. Acad. Med. 2002, 77, 1185–1188.
- Cantillon, P.; Sargeant, J. Giving Feedback in Clinical Settings. BMJ 2008, 337, 1292–1294.
- Accreditation Council for Pharmacy Education. Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Available online: (accessed on 2 March 2021).
- ASHP Commission on Credentialing. Guidance Document for the ASHP Accreditation Standard for Postgraduate Year One (PGY1) Pharmacy Residency Programs. Available online: (accessed on 5 January 2021).
- Hattie, J.; Clarke, S. Visible Learning: Feedback; Routledge: New York, NY, USA, 2019.
- Taylor, D.C.; Hamdy, H. Adult Learning Theory: Implications for Learning and Teaching in Medical Education: AMEE Guide No. 83. Med. Teach. 2013, 35, e1561–e1572.
- Kluger, A.N.; DeNisi, A. The Effects of Feedback Interventions on Performance: A Historical Review, a Meta-Analysis, and a Preliminary Feedback Intervention Theory. Psychol. Bull. 1996, 119, 254–284.
- Bing-You, R.; Hayes, V.; Varaklis, K.; Trowbridge, R.; Kemp, H.; McKelvy, D. Feedback for Learners in Medical Education. Acad. Med. 2017, 92, 1346–1354.
- Mpotos, N.; De Wever, B.; Cleymans, N.; Raemaekers, J.; Valcke, M.; Monsieurs, K.G. Efficiency of Short Individualised CPR Self-Learning Sessions with Automated Assessment and Feedback. Resuscitation 2013, 84, 1267–1273.
- Persky, A.M.; Greene, J.M.; Anksorus, H.; Fuller, K.A.; McLaughlin, J.E. Developing a Comprehensive First-Year Capstone to Assess and Inform Student Learning and Curriculum Effectiveness. Am. J. Pharm. Educ. 2019, 83, 6730.
- Valdez, C.; Shea, L.; Knutsen, R.; Hoody, D. Facilitating Skill Development Using Student-Directed Activities and Personalized Formative Feedback. Curr. Pharm. Teach. Learn. 2014, 6, 826–833.
- Beal, J.L.; Weber, Z.A.; Isaacs, A.N.; Illingworth Plake, K.S.; Zillich, A.; Woodyard, J.L. Pharmacy Student Perceptions and Preferences of In-Person versus Video-Recorded Evaluations in Skills-Based Courses. Am. J. Pharm. Educ. 2020, 84, 1499–1508.
- Planas, L.G.; Er, N.L. A Systems Approach to Scaffold Communication Skills Development. Am. J. Pharm. Educ. 2008, 72, 12.
- Buring, S.M.; Brown, B.; Kim, K.; Heaton, P.C. Implementation and Evaluation of Motivational Interviewing in a Doctor of Pharmacy Curriculum. Curr. Pharm. Teach. Learn. 2011, 3, 78–84.
- Hanya, M.; Yonei, H.; Kurono, S.; Kamei, H. Development of Reflective Thinking in Pharmacy Students to Improve Their Communication with Patients through a Process of Role-Playing, Video Reviews, and Transcript Creation. Curr. Pharm. Teach. Learn. 2014, 6, 122–129.
- Melody, K.; Harris, E.M.; Grover, A.B. Development and Evaluation of an Elective Course That Incorporates a Standard Medication Therapy Management Certificate Program. Curr. Pharm. Teach. Learn. 2018, 10, 1104–1112.
- Powers, M.F.; Bright, D.R. Communication Training and Assessment Using Webcams. J. Pharm. Technol. 2010, 26, 187–192.
- Brown, M.C.; Kotlyar, M.; Conway, J.M.; Seifert, R.; Peter, J.V.S. Integration of an Internet-Based Medical Chart into a Pharmacotherapy Lecture Series. Am. J. Pharm. Educ. 2007, 71, 53.
- Skelley, J.W.; Wulz, J.L.; Thibodeaux, A.M. Implementation of an Electronic Medical Record Simulation Activity Aligned with the Pharmacist Patient Care Process in an Ambulatory Care Elective Course. Pharm. Educ. 2018, 18, 91–98.
- Gogineni, H.; Aranda, J.P.; Garavalia, L.S. Designing Professional Program Instruction to Align with Students’ Cognitive Processing. Curr. Pharm. Teach. Learn. 2019, 11, 160–165.
- Burnworth, M. Development of an Elective Course in Rare and Interesting Diseases. Curr. Pharm. Teach. Learn. 2013, 5, 564–573.
- Pittenger, A.L.; Dimitropoulos, E.; Foag, J.; Bishop, D.; Panizza, S.; Bishop, J.R. Closing the Classroom Theory to Practice Gap by Simulating a Psychiatric Pharmacy Practice Experience. Am. J. Pharm. Educ. 2019, 83.
- Villa, K.R.; Sprunger, T.L.; Walton, A.M.; Costello, T.J.; Isaacs, A.N. Inter-Rater Reliability of a Clinical Documentation Rubric within Pharmacotherapy Problem-Based Learning Courses. Am. J. Pharm. Educ. 2020, 84, 886–891.
- Strohfeldt, K.; Grant, D.T. A Model for Self-Directed Problem-Based Learning for Renal Therapeutics. Am. J. Pharm. Educ. 2010, 74, 7.
- Bond, R.; Donohoe, K.L.; Jakeman, B.; Davis, H.T.; Morgan, L. Combining Rhetoric and Role-Play to Introduce and Develop Patient Presentation Skills in Third Year Pharmacy Students. Curr. Pharm. Teach. Learn. 2017, 9, 1164–1169.
- Kawaguchi-Suzuki, M.; Fuentes, D.G.; Gibbard, R.S.; Backus, D.; Marcus, K. Integration of Mentored Self-Directed Learning (MSDL) through Both Group and Individual Presentations in an Accelerated Modified Block Program. Curr. Pharm. Teach. Learn. 2018, 10, 946–954.
- Sibbald, D. Elective Self-Care Course Emphasizing Critical Reasoning Principles. Am. J. Pharm. Educ. 2011, 75, 182.
- Kelsch, M.P.; Werremeyer, A.B. Poster Project to Emphasize Public Health in the Pharmacy Curriculum. Am. J. Pharm. Educ. 2011, 75, 2.
- Kalata, L.R.; Abate, M.A. A Mentor-Based Portfolio Program to Evaluate Pharmacy Students’ Self-Assessment Skills. Am. J. Pharm. Educ. 2013, 77, 81.
- Hernick, M. Test-Enhanced Learning in an Immunology and Infectious Disease Medicinal Chemistry/Pharmacology Course. Am. J. Pharm. Educ. 2015, 79, 97.
- Maher, S.; Hayden, J.C.; Strawbridge, J.D.; Gallagher, P.J.; Flood, M. Both Useful in Their Own Way’: Video Podcasts and Typed Solutions as Feedback on Undergraduate Pharmaceutical Calculations Skills Assessment. Curr. Pharm. Teach. Learn. 2020, 12, 367–377.
- Lewis, D.J.A.; Sewell, R.D.E. Providing Formative Feedback from a Summative Computer-Aided Assessment. Am. J. Pharm. Educ. 2007, 71, 33.
- Mpotos, N.; Lemoyne, S.; Calle, P.A.; Deschepper, E.; Valcke, M.; Monsieurs, K.G. Combining Video Instruction Followed by Voice Feedback in a Self-Learning Station for Acquisition of Basic Life Support Skills: A Randomised Non-Inferiority Trial. Resuscitation 2011, 82, 896–901.
- Mpotos, N.; De Wever, B.; Calle, P.A.; Valcke, M.A.; Peersman, W.; Monsieurs, K.G. Acquiring Basic Life Support Skills in a Self-Learning Station: Video Alone Is Not Enough. Eur. J. Emerg. Med. 2013, 20, 315–321.
- Sherman, J.J.; Johnson, C.D. Assessment of Pharmacy Students’ Patient Care Skills Using Case Scenarios with a SOAP Note Grading Rubric and Standardized Patient Feedback. Curr. Pharm. Teach. Learn. 2019, 11, 513–521.
- Barnett, S.G.; Gallimore, C.; Kopacek, K.J.; Porter, A.L. Evaluation of Electronic SOAP Note Grading and Feedback. Curr. Pharm. Teach. Learn. 2014, 6, 516–526.
- Nutan, M.T.H.; Demps, E.L. Online Assessments in Pharmaceutical Calculations for Enhancing Feedback and Practice Opportunities. Curr. Pharm. Teach. Learn. 2014, 6, 807–814.
- Strohfeldt, K.; Khutoryanskaya, O. Using Problem-Based Learning in a Chemistry Practical Class for Pharmacy Students and Engaging Them with Feedback. Am. J. Pharm. Educ. 2015, 79, 141.
- Basheti, I.A.; Qunaibi, E.A.; AbuRuz, S.; Samara, S.; Bulatova, N.R. Home Medication Reviews in a Patient Care Experience for Undergraduate Pharmacy Students. Am. J. Pharm. Educ. 2013, 77, 173.
- Denton, P.; Madden, J.; Roberts, M.; Rowe, P. Students’ Response to Traditional and Computer-Assisted Formative Feedback: A Comparative Case Study. Br. J. Educ. Technol. 2008, 39, 486–500.
- Haack, S.; Fornoff, A.; Caligiuri, F.; Dy-Boarman, E.; Bottenberg, M.; Mobley-Bukstein, W.; Bryant, G.; Bryant, A. Comparison of Electronic versus Paper Rubrics to Assess Patient Counseling Experiences in a Skills-Based Lab Course. Curr. Pharm. Teach. Learn. 2017, 9, 1117–1122.
- Medina, M.S.; Conway, S.E.; Davis-Maxwell, T.S.; Webb, R. The Impact of Problem-Solving Feedback on Team-Based Learning Case Responses. Am. J. Pharm. Educ. 2013, 77, 189.
- Nemec, E.C.; Dintzner, M. Comparison of Audio versus Written Feedback on Writing Assignments. Curr. Pharm. Teach. Learn. 2016, 8, 155–159.
- Basheti, I.A.; Ryan, G.; Woulfe, J.; Bartimote-Aufflick, K. Anonymous Peer Assessment of Medication Management Reviews. Am. J. Pharm. Educ. 2010, 74, 77.
- Evans, B.W.; Alinier, G.; Kostrzewski, A.J.; Lefteri, K.A.; Dhillon, S. Development and Design of Objective Structured Clinical Examinations (OSCE) in Undergraduate Pharmacy Education in a New School of Pharmacy in England. Curr. Pharm. Teach. Learn. 2011, 3, 216–223.
- Gums, T.H.; Kleppinger, E.L.; Urick, B.Y. Outcomes of Individualized Formative Assessments in a Pharmacy Skills Laboratory. Am. J. Pharm. Educ. 2014, 78, 166.
- Kubota, R.; Shibuya, K.; Tanaka, Y.; Aoki, M.; Shiomi, M.; Ando, W.; Otori, K.; Komiyama, T. Clinical Pharmacy Education in Japan: Using Simulated Patients in Laboratory-Based Communication-Skills Training before Clinical Practice. Pharmacy 2018, 6, 49.
- O’Reilly, C.L.; Moles, R.J.; Boukouvalas, E.; El-Den, S. Assessing Students’ Mental Health Crisis Skills via Consumers with Lived Experience: A Qualitative Evaluation. J. Ment. Health Train. Educ. Prac. 2019, 14, 361–371.
- Bajis, D.; Chaar, B.; Basheti, I.A.; Moles, R. Pharmacy Students’ Medication History Taking Competency: Simulation and Feedback Learning Intervention. Curr. Pharm. Teach. Learn. 2019, 11, 1002–1015.
- DeLucenay, A.J.; Conn, K.M.; Corigliano, A. An Evaluation of the Impact of Immediate Compared to Delayed Feedback on the Development of Counselling Skills in Pharmacy Students. Pharm. Educ. 2017, 17, 322–328.
- Tait, L.; Lee, K.; Rasiah, R.; Cooper, J.M.; Ling, T.; Geelan, B.; Bindoff, I. Simulation and Feedback in Health Education: A Mixed Methods Study Comparing Three Simulation Modalities. Pharmacy 2018, 6, 41.
- Bailey, L.; Curington, R.; Espel, M.; Brown, B.; Hegener, M. Motivational Interviewing Education: Creation and Assessment of a Learning Module Implemented among Advanced Pharmacy Practice Experience Students. J. Am. Pharm. Assoc. 2016, 56, e25–e26.
- Bates, J.S.; Buie, L.W.; Lyons, K.; Rao, K.; Pinelli, N.R.; McLaughlin, J.E.; Roth, M.T. A Study of Layered Learning in Oncology. Am. J. Pharm. Educ. 2016, 80, 68.
- Flood, M.; Hayden, J.C.; Bourke, B.; Gallagher, P.J.; Maher, S. Design and Evaluation of Video Podcasts for Providing Online Feedback on Formative Pharmaceutical Calculations Assessments. Am. J. Pharm. Educ. 2017, 81, 6400.
- Wigmore, B.C.; Collins, J.C.; Schneider, C.R.; Arias, D.; Moles, R.J. Ability of Pharmacy Students, Pharmacists and Pharmacy Support Staff to Manage Childhood Fever via Simulation. Am. J. Pharm. Educ. 2018, 82, 6445.
- Korayem, G.B.; Alboghdadly, A.M. Integrating Simulation into Advanced Pharmacy Practice Experience Curriculum: An Innovative Approach to Training. Saudi Pharm. J. 2020, 28, 837–843.
- Muzyk, A.; Mullan, P.; Andolsek, K.; Derouin, A.; Smothers, Z.; Sanders, C.; Holmer, S. A Pilot Interprofessional Course on Substance Use Disorders to Improve Students’ Empathy and Counseling Skills. Am. J. Pharm. Educ. 2020, 84, 438–444.
- Nisly, S.A.; Nifong, E.; Coble, E.B.; Mihm, A.E. Longitudinal Pharmacy Student Presentations Mentored by Pharmacy Residents: A Pilot Study. Curr. Pharm. Teach. Learn. 2021, 13, 63–67.
- Andrus, M.R.; McDonough, S.L.K.; Kelley, K.W.; Stamm, P.L.; McCoy, E.K.; Lisenby, K.M.; Whitley, H.P.; Slater, N.; Carroll, D.G.; Hester, E.K.; et al. Development and Validation of a Rubric to Evaluate Diabetes SOAP Note Writing in APPE. Am. J. Pharm. Educ. 2018, 82, 6725.
- Blackmer, A.B.; Thompson, M.; Brunner, J.M.; Patel, T.; Saseen, J.J. Implementation and Assessment of a Novel APPE Intersession Course to Assess Near-Terminal Student Competence. Am. J. Pharm. Educ. 2018, 82, 6460.
- Chiau, T.P.; Ali, A.M.; Bakry, M.M.; Azmi, N.; Paraidathatu, T. Video Recording Feedback in Communication and Counselling among Pharmacy Students. Is It Better than Verbal Feedback? Indian J. Pharm. Educ. Res. 2016, 50, 246–250.
- Teply, R.; Spangler, M.; Klug, L.; Tilleman, J.; Coover, K. Impact of Instruction and Feedback on Reflective Responses during an Ambulatory Care Advanced Pharmacy Practice Experience. Am. J. Pharm. Educ. 2016, 80, 81.
- Nguyen, T.; Wong, E.; Wang, Z.; Goldberg, T. SOAP Notes During APPEs: Assessment of Student Performance. J. Pharm. Pract. 2019, 2–5.
- Bushell, M.J.A.; Austin, J.; Moore, L.; Hendry, E.; Adams, A. Mock Interviews for Internships: Improving Pharmacy Student Preparedness Using Formative Assessment. Pharm. Educ. 2015, 15, 159–161.
- Caballero, J.; Benavides, S.; Steinberg, J.G.; Clauson, K.A.; Gauthier, T.; Borja-Hart, N.L.; Marino, J. Development of a Residency Interviewing Preparatory Seminar. Am. J. Health Syst. Pharm. 2012, 69, 400–404.
- Knutsen, S.; Hanselin, M.R.; Lalama, J.; Moote, R. Preparation Bootcamp for Pharmacy Residency Application and Interviews. Pharm. Educ. 2018, 18, 1–4.
- Koenigsfeld, C.F.; Wall, G.C.; Miesner, A.R.; Schmidt, G.; Haack, S.L.; Eastman, D.K.; Grady, S.; Fornoff, A. A Faculty-Led Mock Residency Interview Exercise for Fourth-Year Doctor of Pharmacy Students. J. Pharm. Pract. 2012, 25, 101–107.
- Wolfgang, K.W. A Novel and Comprehensive Design of Mock Residency Interviews for Fourth-Professional Year Doctor of Pharmacy Students. Curr. Pharm. Teach. Learn. 2019, 11, 956–960.
- Medina, M.S.; Schwier, N.C.; Miller, J.L.; Miller, M.M.; Skrepnek, G.H. Career Skills Assessment in a Doctor of Pharmacy Curriculum. Am. J. Pharm. Educ. 2018, 82, 6300.
- Buckley, K.; Bowman, B.; Raney, E.; Afolabi, T.; Fettkether, R.M.; Larson, S.; Tennant, S.; Goodlet, K.J. Enhancing the Emotional Intelligence of Student Leaders within an Accelerated Pharmacy Program. Am. J. Pharm. Educ. 2020, 84, 1476–1481.
- Lucas, C.; Gibson, A.; Shum, S.B. Pharmacy Students’ Utilization of an Online Tool for Immediate Formative Feedback on Reflective Writing Tasks. Am. J. Pharm. Educ. 2019, 83, 1260–1267.
- Ray, M.E.; DuBrava, L.; Jacks, M. Leveraging a Required E-Portfolio Course to Meet Multiple Needs: Student Assessment, Curriculum Improvement, and Accreditation. Curr. Pharm. Teach. Learn. 2020, 12, 1437–1446.
- Caballero, J.; Benavides, S.; Clauson, K.A.; Steinberg, J.G.; Gauthier, T.P.; Elrod, S.; Marino, J. Impact of a Residency Interviewing Preparatory Seminar (RIPS) Elective in Securing Post-Doctoral Training. Pharmacotherapy 2012, 32, e195–e196.
- Hodder, R.V.; Rivington, R.N.; Calcutt, L.E.; Hart, I.R. The Effectiveness of Immediate Feedback during the Objective Structured Clinical Examination. Med. Educ. 1989, 23, 184–188.
- Rung, A.; George, R. A Systematic Literature Review of Assessment Feedback in Preclinical Dental Education. Eur. J. Dent. Educ. 2020, 25, 135–150.
- Paterson, C.; Paterson, N.; Jackson, W.; Work, F. What Are Students’ Needs and Preferences for Academic Feedback in Higher Education? A Systematic Review. Nurse Educ. Today 2020, 85.
This entry is offline, you can click here to edit this entry!
