Crohn’s Disease (CD) is a chronic idiopathic inflammatory affection involving the gastrointestinal (GI) tract. CD is a lifelong, currently incurable condition, whose natural history is characterized by alternating quiescent periods and active flares of inflammation, progressing to bowel damage and subsequent considerable morbidity [
1,
2]. To date, approximately 10% of CD cases are diagnosed before the patient’s 17th birthday, with a progressive acceleration in incidence in the last few decades [
3,
4]. When arising during childhood or adolescence, CD typically presents with a more extensive/panenteric phenotype [
5,
6]. In addition, as the disease occurs in a period of important developmental milestones, such as growth and puberty, children and adolescents are in a particularly vulnerable situation and management strategies need to deal with these peculiarities [
7,
8]. The exact pathophysiology of CD remains undetermined. It has been widely endorsed that multifactorial etiology, including an interaction between genetic and environmental factors, can contribute to CD pathogenesis [
9]. Advances in DNA sequencing have led to the identification of more than 200 risk loci [
10], which are estimated to explain only 25% of the inheritability of inflammatory bowel disease (IBD) [
11,
12]. The recent progress in basic and clinical science has changed our appraisal of the role of non-genetic factors in IBD susceptibility [
13]. The dramatic rise in the incidence of IBD in newly industrialized countries shifting to Western dietary habits [
14] represents one of the foremost clues to the relevant influence of environmental factors, including diet, on IBD pathogenesis. Dietary components have proven to be able to shape gut microbiota composition [
15,
16] and intestinal wall permeability [
17], altering the interaction between host and intestinal microbiota, the latter being addressed as a master regulator of metabolism and immune response [
13,
18,
19]. More specifically, high animal or dairy fat, animal protein, wheat, emulsifiers and thickeners appear to be strongly associated with intestinal inflammation in animal models [
13]. Historically, growth failure at disease presentation represents one of the hallmarks of pediatric IBD, especially in CD, where it has also been associated with underweight and malnutrition [
20]. Growth failure and malnutrition in IBD develop from a combination among low caloric input owing to decreased food intake (because of abdominal pain or restricted diets), malabsorption, increased basal metabolism and chronic inflammatory condition [
21]. Undernutrition and nutritional deficiencies are associated with poorer clinical outcomes, such as higher infection rates or in-hospital length of stay, and with higher postoperative complications [
22]. Despite being acknowledged as a multifactorial disease, where genetics, the immune system and the environment interplay, leading to disease onset and maintenance, treatment of CD remains focused on immune suppression (such as corticosteroids, methotrexates, thiopurines and biologic agents such anti-tumor necrosis factor alpha (TNFα)) [
23]. Furthermore, notwithstanding the expansion of medical treatments, CD is still associated with non-negligible morbidity, mainly owing to its progression to complicated disease [
24]. Moreover, the use of immunosuppressant agents and biologic drugs bears with it an increased risk of serious infections and malignancies [
25,
26]. In turn, corticosteroid use in pediatric patients affected by CD is associated with growth impairment and bone maturation delay [
27,
28]. Lastly, the achievement of consistent rates of deep outcomes (such as mucosal healing), along with sustained maintenance of remission, are still unfulfilled objectives [
29,
30]. Multiple studies in children with CD have demonstrated the efficacy in the induction of remission, the excellent safety profile and the nutritional benefits of exclusive enteral nutrition (EEN) [
31,
32]. However, EEN has tolerability issues, limiting compliance and widespread clinical application [
33]. From this perspective, multiple research lines have investigated the efficacy of novel dietary therapeutic strategies designed to allow access to food excluding potential harmful substances for intestinal wall integrity and microbiome [
34,
35]. Such dietary strategies may enable the simultaneous targeting of the induction and maintenance of remission, allowing medication sparing, with the modulation of the gut microenvironment and the correction of possible macro- or micronutrient deficiencies and optimization of nutritional status.
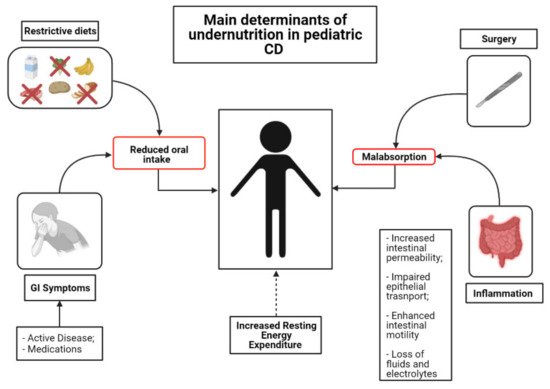
2. Mechanisms and Clinical Implications of Undernutrition in Children with CD
The inflammatory involvement in CD may extend throughout the length of the small bowel, thus impairing the absorption and processing of nutrients [
36]. However, several other factors contribute to development of inadequate nutritional states in IBD [
37]. One of the foremost determinants of malnutrition in IBD is reduced oral intake of food. Active disease often leads to reduced appetite due to abdominal symptom onset (abdominal pain, diarrhea, vomiting and nausea) [
38]. Moreover, inflammation itself (i.e., via TNF-α and IL-6) can cause a reduction in appetite via catabolic effects and hypothalamic weight regulation [
39]. In addition, some of the most commonly prescribed medications can induce nausea, vomiting and/or anorexia [
40]. Lastly, some patients and/or their parents believe that certain foods may worsen, or even elicit, their symptoms. Therefore, they are inclined to modify their diet, excluding putative noxious triggers, in order to control their disease. According to a recent European survey, the most commonly charged foods are grains (29%), milk (28%), vegetables (18%) and fruits (11%) [
41]. This behavior may have detrimental effects on nutritional status [
42]. The intestinal epithelium can be easily disrupted during gut inflammation [
43]. Impaired epithelial transport and loss of mucosal integrity are tightly associated with malabsorption. Indeed, deterioration of epithelial function leads to alterations of ionic transport, which consequently cause loss of fluids and electrolytes [
38]. Furthermore, inflammation of the intestinal mucosa results in chronic leakage of blood and proteins [
38]. Surgery is also associated with impairment of macro- and micronutrient absorption [
38]. Bowel resections can cause accelerated intestinal transit and diarrhea, thus reducing the contact time of the luminal contents with the mucosal surface. Lastly, conflicting evidence exists regarding Resting Energy Expenditure (REE). REE represents the energy needs for an individual in resting condition [
44]. Increased REE is thought to contribute to augmented caloric requirements in patients with active IBD. However, the latter issue remains controversial, as some studies have documented a positive correlation between REE and disease activity [
45], whereas some others have not [
46] ().
Figure 1. Mechanisms of undernutrition in children with CD.
Linear growth impairment may be the first presenting symptom in up to 46% of children and adolescents affected by CD [
47,
48]. The prevalence of undernutrition and growth impairment has substantially decreased throughout the last few decades among patients with IBD [
47,
49,
50]. However, irrespective of treatment modality, impaired linear growth and underweight still affect a significant proportion of pediatric patients with CD [
51]. Underweight at diagnosis is associated with poorer disease outcomes [
21,
52]. In a retrospective longitudinal study, Yerushalmy-Feler reported that BMI in the lower quartile at diagnosis was associated with disease flares (HR: 3.212,
p = 0.016) and with the need for anti-TNF- α (HR: 4.489,
p = 0.021) in a cohort of children with IBD [
52]. In a subsequent study from the same group, BMI in the lower quartile at 6, 12 and 18 months from diagnosis was associated with disease exacerbations (HR: 1.90, 1.98 and 2.43, respectively,
p < 0.021) [
21]. Children affected by CD have an altered body composition compared to healthy controls [
53,
54]. Thangarajah et al. [
53] performed a systematic review aiming to define the alterations in non-bone tissue compartments in children with IBD. The results of the review showed that children affected by CD have a lower lean mass compared to healthy subjects [
53]. In a recent prospective study, Ward et al. [
55] enrolled 73 children with newly diagnosed CD to assess the impact of IBD on musculoskeletal health. The authors reported that total body lean mass (
z-score −2.5, SD 1.1,
p < 0.01) was low for age and gender. Furthermore, jumping mechanography demonstrated low muscle power [
55]. Interestingly, children and adolescents with IBD show chronic deficits in lean body mass in spite of weight restoration and quiescent disease [
56,
57]. Persistence of lean mass deficiency negatively affects metabolic homeostasis, physical activity and bone mass accrual along with bone architecture and it is known to increase the risk of infections [
58,
59]. Moreover, lean mass deficit is known to affect negatively also some of the specific disease-related outcomes in IBD. In a retrospective study including 68 patients affected by IBD, Holt et al. [
60] reported that lower values of skeletal muscle areas at TNF-α initiation were associated with a shorter time to loss of response. Despite advances in medical therapies, non-negligible numbers of patients during their disease course require a surgical intervention [
61]. Unfortunately, undernutrition is a frequent clinical feature of children and adolescents who are referred to surgery. A long disease course, along with persistently active mucosal inflammation and the side effects of the multiple lines of medications, contribute to malnourishment in such patients. Undernutrition can have detrimental effects on post-surgical course. In a retrospective study on 161 CD patients who underwent elective ileocecal resection, poor nutritional status was independently associated with increased risk of postoperative septic complications [
62]. Recently, the clinical implications of diminished lean body mass have been investigated by Ryan et al. [
63]. Despite the vast heterogeneity in the assessment of sarcopenia, in a systematic review, the authors demonstrated that lean body mass deficit can predict the need for surgical intervention in patients with IBD and it is further associated with higher rates of major postoperative complications [
63].
3. Nutritional Therapies
Nutritional status represents one of the foremost determinants of both clinical and surgical outcomes for patients affected by CD [
118]. From this perspective, the identification, prevention and correction of nutritional deficiencies can be considered a therapeutic intervention as crucial as the choice of adequate pharmacological strategies. Indeed, malnutrition and impaired linear growth can be suggestive of active disease and their restoration should be considered as a treatment goal [
44].
3.1. EEN
EEN is a nutritional treatment strategy that provides the total amount of calories and nutrient requirements of patients through a proprietary liquid formula administered orally via an enteral tube. There are three main types of EEN currently available, namely elemental (amino-acid-based), semi-elemental (oligopeptide-based) and polymeric (whole-protein-based) formulas [
119]. Elemental formulas are entirely antigen-free, and they are best-suited in cases of severe malabsorption, where there may be impairment of the gastrointestinal tract. Oligopeptide formulas are peptide-based feeds where the source of nitrogen is represented by peptides of four or five amino acids in length obtained from hydrolysis of whole proteins. Lastly, polymeric feeds contain whole proteins from milk, egg, soy or even meat [
119]. Efficacy of EEN does not vary according to the type of feed, as it also has been recently confirmed by a Cochrane review of EEN for the induction of remission in CD that evaluated the different formulas composition and found no difference in efficacy or in side effects [
120]. However, polymeric feeds are more palatable when consumed orally and they are more commonly used to improve adherence to treatment, helping to overcome one of the major limitations of EEN treatment [
121]. EEN has no major medical side effects. The more commonly reported adverse effects by patients on EEN include diarrhea, nausea and vomiting. Moreover, in pediatric CD, in extremely selected cases with prolonged nutritional restriction, abrupt re-introduction of calories may be associated with refeeding syndrome [
122,
123].
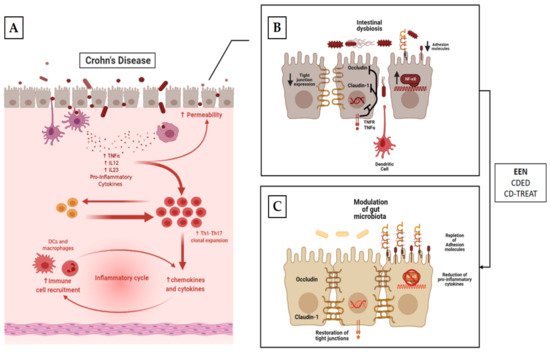
3.1.1. Mechanism of Action
Impaired epithelial barrier function, alterations of normal gut microbiota composition and translocation of bacteria through the intestinal epithelium have all been described in IBD and thus in CD [
13,
124,
125,
126]. Despite the wide availability of data regarding EEN utilization for the induction of remission in CD, there is a considerable knowledge gap in our understanding of its exact mechanism of action. EEN has the ability to mitigate the aberrant immune response that characterizes CD and thus to relieve inflammation. This has been highlighted by several in vivo and in vitro studies [
127,
128,
129]. EEN is thought to exert its anti-inflammatory properties through deactivation of the major intracellular signaling pathways NF-κB [
129,
130]. Two amino acids contained in the polymeric formula, arginine and lysine, have been addressed as responsible for this effect via interference with its kinase activity [
131]. In an in vitro study, the polymeric formula has also been demonstrated to reduce the production of pro-inflammatory cytokines as IL-6, IL-8, IL-1b and IFN-γ by peripheral blood mononuclear cells isolated from children with active CD [
132]. Besides the reduction of pro-inflammatory cytokines, EEN has also been shown to be able to enhance TGF-β1 [
133], an immune-suppressive cytokine whose signaling pathway has been detected in patients with active CD’s intestine [
134]. Consequently, some authors have postulated that enrichment of EEN formulations with TGF-β might boost their anti-inflammatory properties [
135]. Further, EEN has been demonstrated to increase the expression of some of the adhesion molecules involved in the innate intestinal immune response. Repletion of such transmembrane proteins may prevent bacterial interaction with intestinal epithelial cells and thus their activation of dendritic cells, macrophages and the mucosal inflammation cascade [
136,
137]. EEN has also been shown to improve mucus integrity and gut permeability in children affected by CD. This effect is thought to be exerted by: (i) avoidance of dietary products that impair intestinal barrier [
13]; (ii) reduction of pro-inflammatory cytokines that have been implicated in the reduction of permeability [
138]; (iii) restoration of cell-to-cell adhesion molecules (such as occludin and claudin-1) [
138] ().
Figure 2. Mechanism of action of EEN, CDED and CD-TREAT. The panels (A,B) depict the potential pathogenic effects of diet on the development of CD. (i) Reduction in the expression of apical membrane adhesion molecules, which cause increased interactions between bacteria and epithelial membrane. (ii) Reduction in the synthesis and expression of lateral tight junction proteins, causing defects in gut barrier. As a consequence, there is an amplification of the interaction between gut bacteria and immune cells, causing stimulation of pro-inflammatory cytokine secretion and attracting and stimulating the proliferation of pro-inflammatory T-cells with the establishment of a pro-inflammatory milieu along with a self-empowered mechanism. Panel (C) describes the potential effects of nutritional interventions. (i) Modulation of gut microbiota. (ii) Enhancement of expression of apical adhesion molecules. (iii) Increased expression of tight junction with restoration of intestine permeability. (iv) Reduction in pro-inflammatory cytokines and, as a consequence, polarization of immune response towards a regulatory phenotype of T cells.
Pediatric patients with newly diagnosed CD display reduced microbial diversity when compared to healthy controls [
139], with a relatively lower representation of Firmicutes as well as an expansion of Proteobacteria [
140]. Moreover, the intestinal metabolic signature of patients with CD, including short-chain fatty acid (SCFA) reduction [
141,
142], amino acid abundance [
142] and bile acid composition dysregulation [
143], pronouncedly differs from those of healthy controls. Modulation of gut microbiota along with intestinal metabolic changes are among the likely mechanisms through which EEN exerts its functions [
144,
145]. Interestingly, some studies have demonstrated that EEN administration is associated with a reduction in the alpha-diversity of gut microflora, a parameter usually associated with microbiota “fitness” [
146]. Additionally, a reduction in SCFAs such as butyrate, a presumed beneficial metabolite for the host, has been observed during successful EEN induction treatment [
146]. However, it is worth noting that these findings are not so surprising when looking at the composition of EEN. More specifically, shortage of complex fermentable carbohydrates reduces SCFA substrates, whereas the limited number of EEN components, compared to a regular diet, may account for the reduction in microflora diversity [
144]. Indeed, although fiber has been considered to exert a potential clinical benefit for patients with CD, the vast majority of EEN formulations do not contain any fiber [
147]. Moreover, among the few EEN formulations containing fiber, the main ones were slightly different from the range of fibers included in standard diets. The latter observation, however, does not suggest that fiber is harmful, but rather that its removal from the diet does not worsen symptoms in patients with CD [
147].
Some authors have hypothesized that that EEN may exert its effect by depleting harmful bacteria and thus allowing for subsequent re-colonization [
148]. Lastly, a recent prospective multicenter cohort study including 43 newly diagnosed children with CD receiving EEN as induction therapy reported decreased microbiota diversity, a reduction in fecal amino acid concentration and a partial regularization of the microbial metabolism of bile acids [
144]. Moreover, differences in microbiota and metabolome patterns were observed between responders and non-responders to EEN, postulating the possibility for future prediction of EEN response.
3.1.2. EEN for Induction of Remission in CD
In the early 1970s, Voitk et al. [
149] reported for the first time in an uncontrolled study the use of Enteral Nutrition (EN) as a management option for active IBD. Thirteen patients awaiting surgery were treated with an elemental diet for an average time of 22 days. The authors observed improved nutritional states and, unexpectedly, a clinical improvement, with some even avoiding the intended surgery. Subsequently, the first experiences with elemental diet have been reported also in pediatric populations [
150,
151], showing effectiveness of a 6-week course of elemental diet in restoring growth [
150] and inducing remission [
151]. Following the above-cited pathfinder studies, several other research lines, including several meta-analyses [
120,
152], demonstrated the efficacy of EEN for the induction of remission in patients, especially children with CD. According to this recent body of literature, EEN may induce remission in up to 86% of children with CD, along with a significant decrease in inflammatory biomarkers, such as C reactive protein (CRP), erythrocyte sedimentation rate (ESR) and FC [
27,
153,
154]. Furthermore, in a multicenter prospective inception cohort of newly diagnosed mild-to-moderate CD, Cohen-Dolev et al. [
27] showed that, in a propensity-matched score analysis, EEN was superior to corticosteroids for induction of remission (
p = 0.05) and preservation of linear growth (
p = 0.055). Efficacy of EEN in the induction of clinical remission in children with CD was further confirmed by Lee et al. [
154] also in comparison to biological therapy. Ninety consecutive children with active CD were consequently enrolled in a prospective study, receiving EEN, Infliximab (IFX) or partial enteral nutrition (PEN) for the induction of remission. No differences in clinical response rates between EEN and biologic therapy were observed (88% vs. 84%). Even though symptom control is a relevant endpoint for patients with IBD, more recently, treatment strategies have evolved, moving towards targeting the resolution of mucosal inflammation [
155]. Several studies demonstrated that EEN is also effective in inducing mucosal healing (MH) within 8–10 weeks of its initiation [
156]. In a prospective, open-label study including 26 children with newly diagnosed CD who completed a 6-week EEN course, 15 (58%) had early endoscopic response, with 11 (42%) of them showing complete MH (Simplified Endoscopic Score for CD (SES−CD) = 0). The authors reported also complete transmural remission in 3 out of 14 (21%) patients with ileal CD [
156]. Additionally, EEN has also outperformed corticosteroid treatment in MH achievement when the two strategies have been directly compared. In an open-label, randomized controlled trial enrolling 37 children with recently diagnosed active CD, the proportion of patients showing MH was significantly higher in the EEN group than in the corticosteroid group (74% vs. 33%,
p < 0.05) [
157]. Furthermore, achievement of complete MH after administration of EEN has been shown to predict also long-term sustained clinical remission [
158]. In a prospective single-center study, Grover at al. [
158] demonstrated that, among 54 children with mild-to-moderate CD completing a 6-week EEN induction course, achievement of complete MH (SES-CD = 0) was associated with higher sustained remission at 3 years compared with active endoscopic disease (8/16, (50%) vs. 1/19, (6%),
p = 0.005). Conflicting data regarding the association between EEN efficacy and CD localization are available [
31,
159,
160,
161]. Previous studies suggested a lower efficacy of EEN in patients with isolated colonic disease compared to those with ileal involvement [
160]. Subsequent experiences, however, found no differences between isolated colonic disease and ileal or ileocecal involvement [
31,
161]. In the absence of high-quality evidence, EEN is recommended as the first-line treatment irrespective of CD location [
23,
44]. Moreover, in cases of the second course of EEN, studies have shown good efficacy, with clinical remission rates ranging from 58% to 80%. Moreover, two small prospective studies demonstrated that intermittent administration of EEN over one year resulted in a reduction in corticosteroid need and with increased growth velocity [
162,
163]. These data confirm that if the compliance of the patients is maintained, EEN may be successfully reused during the subsequent course of the disease for future relapses [
44] ().
Table 1. Summary of the studies using EEN as nutritional therapy in children with CD.
| First Author |
Study Design |
Population |
Intervention
(Duration) |
Control Group |
Key Findings |
| Morin [139] |
R |
4 CD with growth failure |
Elemental formula
(6 weeks) |
N/A |
- -
-
Clinical efficacy;
- -
-
Weight and height restoration.
|
| Sanderson [140] |
P/RCT |
8 pts with active CD |
Elemental formula
(6 weeks) |
8 CD patients treated with CS |
- -
-
Significant clinical and biochemical improvement compared to steroids;
- -
-
Improved body weight and linear growth.
|
| Cohen-Dolev [24] |
P/O |
60 patients with newly diagnosed CD |
Any formula
(6–8 weeks) |
87 matched patients treated with CS |
- -
-
EEN was superior to CS for inducing remission;
- -
-
EEN trended to superiority for height z-score compared to CS.
|
| Levine [142] |
P/O |
43 patients with newly diagnosed CD |
Any formula
(6–8 weeks) |
114 patients treated with CS
29 with 5-ASA |
- -
-
EEN and CS effective in normalizing CRP at week 12;
- -
-
In mild-to-moderate CD, EEN was superior to CS in normalizing CRP.
|
| Lee [143] |
P/O |
22 patients with active CD |
Any formula
(6–8 weeks) |
52 patients treated with anti-TNF-α
16 pts with PEN + unrestricted diet |
- -
-
Clinical remission rates of EEN and anti-TNF-α were 88% and 84%, respectively, superior to those of PEN (64%);
- -
-
EEN and anti-TNF-α but not PEN were effective in normalizing FC.
|
| Grover [145] |
P/O |
26 patients with active CD |
Any formula
(6 weeks) |
N/A |
- -
-
58% of patients achieved at least partial MH;
- -
-
21% of pts had complete transmural remission of ileal CD.
|
| Borrelli [146] |
P/RCT |
19 patients with active CD |
Polymeric formula
(10 weeks) |
18 patients treated with CS |
- -
-
No differences were observed in clinical remission rates;
- -
-
EEN was superior to CS in achieving MH.
|
| Grover [147] |
P/O |
54 patients with active disease |
Any formula
(6 weeks) |
N/A |
- -
-
Achievement of complete MH (SES-CD) after EEN course was associated with a long-term sustained response.
|
| Rubio [148] |
R |
45 patients with CD who received oral EEN |
Polymeric formula
(8 weeks) |
61 patients treated with continuous EEN |
- -
-
Similar remission rates;
- -
-
Similar changes in PCDAI and inflammatory markers;
- -
-
Higher weight gain in the continuous EEN group.
|
| Buchanan [149] |
R |
110 patients with CD |
Polymeric/
Elemental formula
(8 weeks) |
N/A |
- -
-
Patients with terminal ileum disease (n = 4) had lower remission rates but no other difference was observed among various disease locations.
|
| Afzal [150] |
R |
65 patients with active CD |
Polymeric formula
(8 weeks) |
N/A |
- -
-
Patients with colonic disease phenotype had significantly lower remission rates compared to ileal and ileocolonic localizations.
|
| Belli [152] |
P |
8 patients with active CD and growth failure |
Polymeric formula
(intermittent administration over 1 year) |
4 matched CD patients not treated with EEN |
- -
-
Intermittent EEN administration showed significant decrease in CDAI and in CS use;
- -
-
Intermittent EEN showed significant height and weight improvement
|
3.1.3. EEN for Preoperative Nutritional Optimization in Children with CD
As previously mentioned, surgery in children with CD is often performed when therapeutic inventory has been depleted, a setting where the onset of postoperative complications is likely to be substantial due to the burden of immunosuppression, hospitalization and malnutrition. Nutritional status is a key element for favorable surgical outcomes [
164]. From this perspective, perioperative nutritional therapy has been addressed as a pivotal element when caring for patients with CD who require surgical interventions [
118]. A recent systematic literature review performed by a consensus expert panel acknowledged the use of nutritional therapies prior to surgery as a perioperative optimization strategy, despite the paucity of available pediatric data [
118]. Indeed, although EEN was first conceived as a preoperative nutritional support, there is a dearth of high-quality studies reporting its systematic use in a preoperative setting [
165,
166]. A recent systematic review explored preoperative nutritional conditioning of patients with CD [
167]. Fourteen original studies were identified. Five out of the studies that included a control group [
165,
168,
169,
170,
171], four of which utilized EEN and one parenteral nutrition (PN), reported improved post-surgical outcomes in patients receiving preoperative nutritional support. To date, the only experience reported in pediatric populations is represented by a small case series reported by Harris et al. [
172], who assessed the use of EEN as a treatment prior to resection surgery for pediatric CD patients. The authors gathered data on 17 CD pediatric patients who underwent right hemicolectomy. Eight of them received a preoperative course of EEN for a median time of 4 weeks (IQR: 3.7–4.0 weeks). The median length of hospital stay after surgery was lower in the EEN cohort compared to the non-EEN one (4.5 days versus 6 days,
p = 0.03). Moreover, the use of EEN was associated with a decreased rate of moderate or severe disease on resection pathology (5/8 (62.5%) versus 9/9 (100%);
p = 0.04). No differences in serologic markers were observed, in contrast to previously published adult literature, arguably due to the small sample size. Replication of the results of this study, along with well-designed prospective studies, hopefully RCTs, are deemed to substantiate EEN’s role in the preoperative setting of pediatric CD.
3.1.4. EEN’s Effects on Body Mass Composition in Children with CD
The benefits of EEN extend beyond its ability to induce remission and its capacity to improve anthropometric indices in patients with CD. Gerasimidis et al. [
32] performed a prospective study enrolling 17 children with active CD who received EEN, aiming to assess its effects on changes on body composition [
32,
173,
174]. The authors reported an improvement in lean body mass after EEN course (lean body mass
z-score: −2.1 vs. −0.8 before and after treatment, respectively;
p < 0.0001) without a significant increase in fat mass [
32]. In the same study, also a significant improvement in circulating micronutrients was observed after EEN treatment [
32]. A more recent prospective study performed by Strisciuglio et al. [
174] reported that EEN was associated with an improvement in both fat free mass (assessed via bioimpedentiometric examination) and bone mineral density (assessed via dual-energy X-ray) in children with newly diagnosed CD. Moreover, the authors observed a significant increase in bone mineral density also at the 1-year follow-up visit, supporting the hypothesis that the reduction in inflammation combined with improvement in nutritional status might be persistent after one year, resulting in ameliorated bone composition and muscle mass. Lastly, a recent sub-study of a randomized clinical trial enrolling children with new-onset mild-to-moderate CD explored the effect of nutritional therapies on bone health. The authors evaluated bone formation and resorption at baseline, at week 12 and at week 24 via serum C-Propeptide of Type I Procollagen (CICP) and type I Collagen N-Telopeptide (NTX), respectively [
175]. Bone mineral density was assessed by dual-energy X-ray. The authors reported a significant improvement in CICP, a sensitive marker of bone formation but not of bone mineral density, suggesting that bone improvement is a challenging and a slow process [
175].
3.2. Partial Enteral Nutrition (PEN) in CD
PEN refers to the replacement of 35% to 50% of habitual food intake with EN feeds while continuing to eat an unrestricted or exclusion diet.
3.2.1. PEN for the Induction of Remission in CD
The first RCT specifically designed to investigate the efficacy of PEN (provided as 50% of elemental formula associated with unrestricted diet) in the induction of remission in children and adolescents with active CD showed unsatisfactory clinical remission rates. Among the 50 children who were randomly assigned to receive either 50% (PEN) or 100% (EEN) of their energy requirement as elemental formula for six weeks, clinical remission rates were significantly lower in the PEN group compared to the EEN one (15% vs. 42%) [
176]. These results suggest that PEN with access to a free diet is ineffective at relieving inflammation when compared with EEN or IFX, restating the principle of exclusivity. Following the results of this robustly designed, groundbreaking study, research interest in PEN as an alternative induction treatment for CD diminished. More recently, Gupta et al. [
177] reported the efficacy of a nutritional treatment protocol involving the administration of 80% to 90% of caloric needs through an EN formula overnight and the remaining 10% to 20% of the daily energy intake from an unrestricted diet. Among 43 CD pediatric patients included in this retrospective study, induction of remission was achieved in 65% of them, within a mean treatment duration of 2 months. However, this nutritional protocol led to frequently reported adverse events (up to 65% of patients) mainly related the use of nocturnal EEN (abdominal distension, sleep disturbances, morning nausea and vomiting, etc.). Nevertheless, these results have not been replicated in more robustly designed studies. Therefore, PEN associated with an unrestricted diet is not currently recommended for the induction of remission of children and adolescents with CD [
23].
3.2.2. Maintenance of Enteral Nutrition (MEN) in CD
Long-term exclusive enteral nutrition and avoidance of a normal diet is an unfeasible therapeutic option for the maintenance of remission, mainly owing to compliance issues. Maintenance of enteral nutrition (MEN) refers to the use of EN formula, accounting for a percentage of the total caloric requirements, for the maintenance of remission in CD. In a retrospective historical cohort, Wilschanski et al. [
178] first reported the effectiveness of supplementary administration of an elemental formula in a cohort of children and adolescents affected by CD. Among 47 pediatric CD patients who achieved remission after EEN induction, 28 of them continued nocturnal supplementary feeding via a nasogastric tube after resumption of an otherwise unrestricted daytime diet. This subset of patients showed a higher cumulative probability of maintaining clinical remission compared to the group of 19 patients who did not receive PEN (
p = 0.005). A subsequent retrospective study showed that up to 50% of patients who received MEN as the only maintenance therapy after a successful course of EEN remained in remission at 1-year follow-up [
179]. This response rate did not differ from those obtained with azathioprine (65%) or with the combination of MEN and azathioprine (67%) but was significantly higher than those achieved without maintenance therapy (15%). Conversely, subsequent studies were not able to confirm the association between MEN and prolonged time to relapse [
180,
181,
182]. A retrospective study performed by Gavin et al. [
181] did not observe a difference in remission length between patients who received MEN and those who remained on a habitual diet (77% vs. 78% 1-year relapse rates). Moreover, in a recent study, Logan et al [
182] demonstrated that patients who used MEN during the early period of food reintroduction following a successful course of EEN had lower FC levels compared to those who did not consume MEN. Nonetheless, this effect appeared to be only short-lived as the use of MEN was not associated with prolongation of remission length. Beyond the sole clinical efficacy, the use of MEN has been associated with additional benefits, such as increased height [
178] and weight [
180] z-scores in children and adolescents. The main evidence to support the benefits of MEN to prolong remission following a successful course of EEN is supported by two RCTs performed in adult cohorts in Japan [
183,
184]. Furthermore, a recent meta-analysis investigated the effects of EN in combination with anti-TNF-alpha antibody treatment in adult patients affected by CD [
185]. The authors demonstrated, via a systematic review of nine studies, that maintenance of remission was higher in the combination group (70.5%) than in the non-EN group (53.8%) [
185]. A lack of pediatric evidence in this field exists. Notably, a “dose-dependent” response association appears to exist between the use of MEN and disease relapse [
186]. A recent review performed by Gkikas et al. showed that consumption of >35% MEN was associated with significantly lower relapse rates compared to the control group, in 8 out of 10 (80%) studies (performed both in children and in adults). Conversely, in all four studies using ≤35% MEN, there was no additional benefit of MEN use in reducing clinical relapse [
186]. Arguably, one of the main barriers to MEN consumption is low compliance, mainly due to formula palatability and patient’s exhaustion. Interestingly, compliance was not assessed in many of the studies in which MEN was not effective [
180,
181]. Therefore, treatment failure could have been biased by low acceptability of the dietary regimen rather than inadequate efficacy of MEN. The heterogeneity among different studies and the lack of RCTs studies in children remain some of the major limitations in this field of knowledge.
3.3. Food-Based Therapies in CD
EEN has shown high efficacy in the short term in inducing clinical remission. However, one of its main barriers is represented by monotony of food and taste fatigue experienced by patients. This is one of the major limitations to the wider access and availability of this type of therapy. Several food reintroduction protocols have been attempted after induction of remission using nutritional therapies [
187,
188,
189]. Among the latter, single-food reintroduction with exclusion of symptom-aggravating foods was the most commonly used protocol [
187], which was associated with lower clinical relapse rates, assessed by disease activity indices, compared to patients following an unrestricted diet. Subsequently, Woolner et al. [
188] demonstrated that a low-fat, low-fiber diet (LOFFLEX) was associated with similar remission rates when compared to a symptom-alleviating, exclusion diet, arguing a higher acceptability for the patient. The results of these studies, conducted in an era in which markers of mucosal inflammation (endoscopies or FC) were not commonly used, need to be cautiously interpreted, as it remains questionable whether gut inflammation parallels symptoms. Recently, Logan et al. [
182] demonstrated a rapid re-exacerbation of inflammation, demonstrated by a rise in FC, during the first 2–3 weeks after the reintroduction of whole food. Hence, re-establishment of a normal diet is associated with reactivation of intestinal inflammation, with MEN showing only a modest effect for the earliest weeks [
182].
From this perspective, an understanding of how remission can be maintained through manipulation of diet represents a compelling unmet need. Therefore, it is no surprise that, in the past few years, multiple research groups have attempted to mimic EEN results with nutritional therapeutic strategies allowing access to whole food (.)
Table 2. Summary of the studies using food-based therapies in children with CD.
| First Author |
Study Design |
Population |
Intervention
(Duration) |
Control Group |
Key Findings |
| Sigall-Boneh [183] |
R |
47 children and young adult pts with active CD |
CDED + PEN (12 weeks, n = 40)
CDED
weeks, n = 7) |
N/A |
Clinical remission achieved in 24/34 children and 9/13 adults at wk 6 and maintained in 27/33 patients at week 12;
Significant fall in clinical disease activity and inflammatory markers. |
| Sigall-Boneh [187] |
R |
21 children and young adult pts with treatment-refractory CD |
CDED + PEN
(12 weeks, n = 12)
CDED
(12 weeks, n = 4)
Mod. EEN + CDED
(2 + 12 weeks, n = 5) |
N/A |
13/21 pts refractory to biologic treatment achieved clinical remission;
9/17 of patients failing double biologic therapy achieved clinical remission;
Significant decrease in serum markers of inflammation. |
| Levine [32] |
P/RCT |
40 pts with mild-to-moderate CD |
CDED + PEN
(12 weeks) |
34 pts with mild-to-moderate CD treated with EEN |
CDED+PEN was equally as effective as EEN in inducing remission at week 6;
CDED+PEN was superior to EEN in maintaining remission at week 12;
CDED+PEN was able to induce rapid remission (3 weeks); |
| Svolos [33] |
OL |
5 pts with active CD
(PCDAI ≥ 12.5) |
CD-TREAT
(8 weeks) |
N/A |
CD-TREAT was able to induce clinical response in 80% and remission in 60% of patients;
80% of pts showed decrease in fecal calprotectin |
3.3.1. Crohn’s Disease Exclusion Diet (CDED)
Among the various food-based therapies, Crohn’s Disease Exclusion Diet (CDED) currently represents the most clinically documented for the treatment of active CD. The pathophysiologic paradigm behind CDED is represented by the “bacterial penetration cycle hypothesis”, according to which the exposure of intestinal mucosa to adherent or penetrating bacterial species may act as a trigger for the immune system, thus generating inflammation, further barrier breakdown and a subsequent increase in the migration of harmful bacteria through a vicious cycle [
190]. CDED was developed to exclude potential harmful foods that have been associated with alterations in host mucous layer [
191], dysbiosis [
192] and with the development of virulence factors [
193] that may allow bacteria to attach to mucosa or to translocate the epithelial barrier. However, CDED is not all about exclusion, as this treatment aims to provide a consistent amount of high-quality protein and to deliver sugars mainly through foods rich in complex carbohydrates. Following these two principles of exclusion and inclusion, natural foods are combined with a variable volume of polymeric formula to meet the nutritional needs and to provide additional amounts of protein, calcium and vitamin D. The CDED nutritional regimen consists of different phases with incremental varieties of food allowed. Phase 1 lasts 6 weeks, aims to induce clinical remission and is the most restrictive one. Besides the elimination of dietary components that trigger inflammation, also fruit and vegetable consumption is restrained during the first phase in order to reduce fiber exposure. PEN is added to provide 50% of the nutritional needs. During phase 2, which lasts a further 6 weeks, access to food is broadened. To increase the flexibility of the diet and to improve adherence, fiber intake is increased so that almost all fruit and vegetables are allowed during this phase. Moreover, also potentially noxious foods (i.e., gluten, red meat, etc.), whose consumption is not permitted during phase 1, are gradually reintroduced in a controlled way. PEN consumption is reduced from 50% to 25% of the nutritional requirements [
194]. Efficacy of CDED was first assessed in a cohort of 47 patients (34 children and 13 adults, mean age: 16 ± 5.6 years) [
195]. Sigall-Boneh et al. [
195] reported that such a dietary intervention, based on CDED combined with PEN at 50%, was able to induce clinical responses in nearly 80% and clinical remission in up to 70% of patients with mild-to-moderate CD. They also demonstrated the capacity of such a dietary regimen to normalize CRP in 70% of patients who achieved clinical remission. The abovementioned results were subsequently confirmed in a 12-week prospective RCT [
34]. Seventy-eight children with mild-to-moderate newly diagnosed CD were randomly assigned to a group (
n = 40) that received CDED plus PEN at 50% for 6 weeks followed by CDED with PEN at 25% from week 7 to 12 or a group (
n = 38) that received EEN for the first 6 weeks and then PEN at 25% with a free diet [
34]. The authors observed no differences in corticosteroid-free remission rates at week 6 (75% in CDED group vs. 59% in EEN group,
p = 0.38). At week 12, the combination of CDED plus PEN was associated with higher remission rates than EEN (75.6% vs. 45.1%,
p = 0.01). Additionally, the authors reported that CDED plus PEN was better tolerated than EEN (tolerance rates: 97.5% vs. 73.6%,
p = 0.002). Furthermore, in a subsequent analysis of the abovementioned RCT, it was demonstrated that CDED + PEN was able to induce a rapid clinical response (at week 3), thus possibly identifying predictors of being in clinical remission at week 6 [
196].
The efficacy of CDED was also demonstrated in another, unfortunately common, clinical scenario: the loss of response to biologic agents [
197,
198]. Sigall-Boneh et al. [
199] reported the outcomes of 21 patients (11 children and 10 adults) with CD who had experienced loss of response (LoR) to a biologic agent despite dose escalation or combination therapy and received a course of 12 weeks of CDED plus PEN at 50%. At week 6, clinical remission was obtained in 13/21 patients (61.9%). Mean CRP levels decreased from 2.8 ± 3.4 mg/dL to 0.7 ± 0.5 mg/dL (
p = 0.005) and mean albumin increased from 3.5 ± 0.6 g/dL to 3.8 ± 0.5 g/dL (
p = 0.06). After the first two phases lasting 12 weeks, the maintenance phase begins. Occasional and controlled access to some type of foods not allowed during the earliest phases is now permitted. The duration of this phase is not strictly determined as it is intended to become a stable modification through a healthier lifestyle [
194].
3.3.2. CD Treatment-with-Eating (CD-TREAT)
CD-TREAT is an individualized, food-based therapy, which aims to recreate as closely as possible the composition of EEN using ordinary (solid) food through the exclusion of certain dietary components (i.e., gluten, lactose) and the combination of others (macronutrients, vitamins, minerals and fiber) [
35]. The objective of such a dietary strategy is to mimic EEN’s capacity to modulate the gut microbiota composition [
35]. Such properties were first assessed by Svolos et al. [
35] in a prospective RCT enrolling 25 healthy subjects, who were randomly allocated to receive either EEN or CD-TREAT for 7 days, each with a 2-week washout in between. The authors reported that the fecal microbiota along with fecal metabolome significantly changed in the same direction for the two dietary strategies, with several parallel changes in metabolites and species [
35]. The effects observed in healthy subjects were subsequently replicated in gut inflammation animal models [
35]. Lastly, CD-TREAT has been administered in a course of 8 weeks to five children with active CD in a pilot study, showing efficacy in inducing clinical remission and in reducing FC [
35]. Although promising, these proof-of-concept data need to be confirmed in an ongoing, adequately powered RCT [
200].