Initial calibration is a great challenge for cuff-less blood pressure (BP) measurement. The traditional one point-to-point (oPTP) calibration procedure had a strong sensitivity in the selection of initial value because of only using one sample/point to obtain unknown parameters of specific model in a calm state. In this study, a mean point-to-point (mPTP) paring calibration method through averaging and balancing calm or peaceful state was proposed for the first time. Thus, based on mPTP, a factor point-to-point (fPTP) paring calibration method through introducing the penalty factor was further proposed to improve and optimize the performance of BP estimation.
- Point-to-point pairing method
- Initial sensitivity
- Penalty factor
- Correcting errors
- Cuff-less blood pressure
1. Cuff-less BP monitoring technology
Uncontrolled hypertension or high blood pressure (BP) was a major risk factor that links to potential development of serious diseases such as stroke, hypertensive heart disease, and coronary artery disease [1]. BP was influenced by many factors such as food, exercise, mental situations, stress, among others; thus, it varied considerably from time to time [2]. Instantaneous information about BP status could be obtained from conventional standard cuff-based BP measurement, such as oscillometry [3] and auscultation. However, these methods were not applicable to ambulatory BP monitoring (ABPM) or home BP monitoring (HBPM) due to the cumbersome and discontinue nature of cuff wrapping around the arm or leg to detect the oscillations during cuff-deflation [4] and the limited frequency of measurement [5]. Moreover, the clinical BP which may not reflect the normal level due to the effect of white coat effect had been questioned [6]. Therefore, the development of cuff-less BP monitoring technology was extremely urgent.
1.1. Cuff-less BP estimation method
For decades, many directions, such as bio-sensor [7]-[8], signal processing [9], calibrating or modeling [10] and performance verification [11] were extensive reported and investigated for cuff-less BP measurement. Various BP monitoring models were proposed based on pulse wave velocity (PWV), pulse transit time (PTT), and pulse wave analysis (PWA), in which pulse signals could be non-invasively obtained through electrocardiogram (ECG), non-invasive photoplethysmography (PPG) [3],[8],[9],[11] and ballistocardiography (BCG) originated from cardiovascular system. Here, PPG, a noninvasive optical measurement technique by means of photoelectric measurement, obtained physiological signals and characteristics of the human body by detecting changes in blood volume in micro-vessels. And the PTT was the time delay for the pressure wave to travel between two arterial sites and could be estimated by a R peak time interval between ECG and PPG signal in same cardiac cycle[7]-[9],[12]. The PTT-based cuff-less BP estimation measurement had shown great potential and attracted extensive attentions [13]-[15], especially while estimating systolic blood pressure (SBP) [12]-[13],[16]. For example, early research by Chen et al. [16] had developed a PTT-BP model based on Moens-Korteweg (M-K) equation [3],[9]-[10],[12]-[14], and showed that PTT could track BP with quite desired accuracy. Similarly, based on M-K equation and Bramwell-Hill (B-H) equation [3],[12], a novel PTT-BP model by Zheng et al. [17] was developed. During a 24-hour smooth changes in BP monitoring experiment, this PTT-BP model was validated a good performance of BP estimation. However, it was meaningful and necessary to investigate the estimating BP performance in the condition of wild BP fluctuations such as intense exercise and excessive tension or fatigue, instead of the condition of smooth changes in BP.
Recently, heuristic modeling were investigated through regression technique, such as linear estimation [21], non-linear estimation [3],[17],[22]-[23], to estimate BP from the indirect indicators, where the indicators included PTT or heart rate (HR) [18], PIR [15], TDB [18], and others. Furthermore, some reports on predictive modeling with data-driven methods such as machine learning, were paid more attention to obtain model for better describing the relationship between BP-indicators and BP through analyzing pulse wave morphology based on more comprehensive and available indicators from ECG or PPG signals [19]-[20]. Although these BP monitoring solutions described above were helpful, their accuracy of estimating BP still need to improve to meet the AAMI standard [24] with a better accuracy.
1.2. Personalized calibration procedure
Referring to the difference of calibration methods during BP estimation models, it could be divided into two categories: least square method (LS) [5],[13],[14],[25] and point-to-point (PTP) pairing method[3] [11],[15]. The LS method could not meet the needs of a small initial sample size in the initial calibration process due to the requirement of all data sets. Hence, the PTP method had caused extensive research in wearable system and cuff-less measurement [3] [11],[15]. However, the PTP calibration method which only needed a single sample was bound to have a huge defect on initial value sensitivity; to some extent, it reduced and weakened the accuracy of BP estimation. Physiological parameters such as PTT and BP were not always constant in a calm state for subjects and could fluctuated in a range of small variations to be observed. For the common one-point PTP (oPTP) calibration method using only one BP paired with one PTT, however, there was no evidence of improvement so far to explain enough the entire calm and rest state. Hence, the calibration method needed to be further improved and explained with more details, especially in the selection of initial samples.
2.Two novel point-to-point calibration methods (mPTP and fPTP)
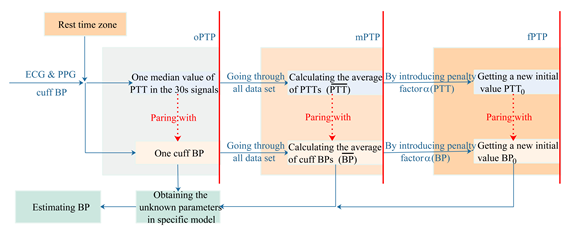
The PTT-based BP measurements are required an individualized calibration to obtain the unknown coefficients or parameters in BP estimation model for each subject before monitoring BP. Here, the mapping relationship between BP and PTT is established through paring one cuff BP with one , which is called one point-to-point (oPTP) paring calibration method. However, it was sensitive that using one pair of cuff BP and to complete the calibration procedure in the oPTP method. Here, we selected one median of PTT from the ECG & PPG signals to pair with one cuff BP for each 30 seconds for completing one calibration behavior according to the specific BP estimation model.
In present study, with all cuff BPs and samples during the clam or peace state about five minutes [3],[9],[12], we researched two new calibration methods to pair PTT with the base value of BP on the basis of oPTP method. Firstly, a mean point-to-point pairing (mPTP) calibration method was proposed to measure the entire state of calm or rest. Thus, a penalty factor point-to-point (fPTP) pairing calibration method was investigated to adjust and real-timely correct estimated difference. The both of mPTP and fPTP calibration methods overcame the limitation of the initial value sensitivity of oPTP method in which BP is taken as a constant in calm or still state. Their calibration procedures in detail are shown in Figure 1.
Figure 1. The calculation procedure for BP monitoring system.
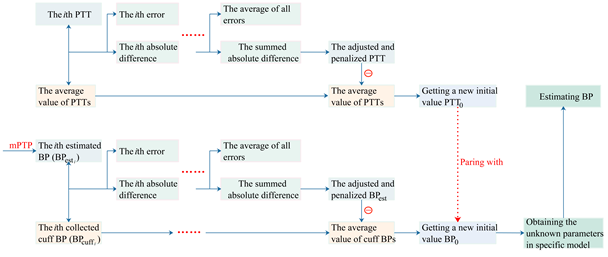
To establish fPTP method, there are two steps: the real-time adjustment of the PTT and the calculation of the base value of cuff BP.
Step 1: the real-time adjustment of the PTT. It comprises of a base value of calibration and a negative feedback function that adjusted and corrected PTT difference to adapt the change of cuff BP.
Step 2: the calculation of the base value of cuff BP. It comprises of a base value of calibration and a negative feedback function responsible for adjusting and correcting the BP estimation errors.
In summary, the penalty factor 



Figure 2. Detailed flowchart on fPTP calibration method
The calibration was done only once for each subject. After deriving parameters in the BP estimation model, the BP could be estimated continuously.
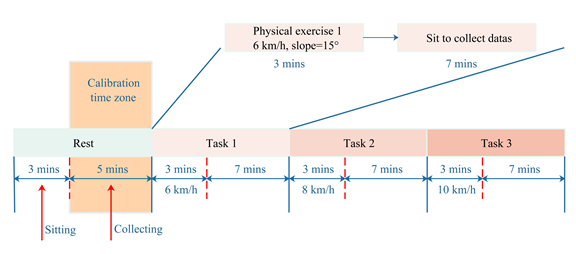
3. Experimental protocol
This experimental protocol was performed in a study room with temperature 23.9 ± 1.6 ◦C and Relative Humidity 60 – 70%. Powerlab/16sp system (Castle Hill, ADInstruments, Australia, 2002) was employed to synchronously record and amplify the ECG and PPG signals. The ECG signal was filtered by a 1 Hz high pass filter and a 40 Hz low-pass filter. Meanwhile, the PPG signal was filtered by a 0.5 Hz high pass filter and a 20 Hz low-pass filter, and the sampling frequency was 1 kHz [12]. The cuff-type BP monitor (HEM-7211-IT, Omron, Japan) was mounted on the right arms of subject to provide reference BP values. Considering that the data sample populations and the replicability of the experimental results, the subjects were required to conduct a resting experiment and exercise a recovery experiment, which took about 35 minutes in total. The exercise recovery experiment was subdivided into three tasks (i.e., task 1, task 2 and task 3), in which the subjects were told to run on a treadmill (Powereach PET-90, China) with a slope of 15 angles at 6 km/h, 8 km/h and 10 km/h for three minutes respectively. Then, signals were collected for seven minutes immediately after each end of the running exercise. The details of the experiment are shown in Figure 3.
Figure 3. Experimental protocol under different tasks
References
- Lewington S.; Clarke R.; Qizilbash N.; et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies, 2002, 361(9366):1389-1390.
- Kachuee M; Kiani M; Mohammadzade H.; et al. Cuff-Less blood pressure estimation algorithms for continuous health-care monitoring, IEEE Trans. Biomed. Eng. 2017, 64(4):859-869.
- Tang ; Tamura T.; Sekine M.; et al. A chair-based unobtrusive cuffless blood pressure monitoring system based on pulse arrival time, IEEE J. Biomed. Health Inf. 2016, 21(5):1194-1205.
- Liu J.; Hahn J. O.; Mukkamala R.; Error mechanisms of the oscillometric fixed-ratio blood pressure measurement method, Biomed.Eng. 2013, 41(3): 587-597.
- Solà ; Chételat O.; Sartori C.; et al. Chest pulse-wave velocity: a novel approach to assess arterial stiffness, IEEE Trans. Biomed. Eng. 2011, 58(1):215-223.
- O'Brien E.; Asmar R.; Beilin L.; et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement, Hypertens. 2003, 21(5):821-48.
- Luo N.; Dai W.; Li C.; et al. Flexible Piezoresistive Sensor Patch Enabling Ultralow Power Cuffless Blood Pressure Measurement, Adv Funct Mater. 2016, 26(8).
- Martin L. O.; Carek A. M.; Kim C. S.; et al. Weighing Scale-Based Pulse Transit Time is a Superior Marker of Blood Pressure than Conventional Pulse Arrival Time, Rep. 2016, 6(1):39273.
- Choi Y.; Zhang Q.; Ko S.; Noninvasive cuffless blood pressure estimation using pulse transit time and Hilbert–Huang transform, Electr. Eng. 2013,39(1):103-111.
- Ding X.; Zhao N.; Yang G.; et al. Continuous blood pressure measurement from invasive to unobtrusive: celebration of 200th birth anniversary of Carl Ludwig, IEEE J. Biomed. Health. 2016, 20(6):1455-1465.
- Mccarthy B. M.; Vaughan C. J.; et al. An examination of calibration intervals required for accurately tracking blood pressure using pulse transit time algorithms, Hum. Hypertens. 2013, 27(12):744-750.
- Mukkamala R.; Hahn J. O.; Inan O. T.; et al. Toward ubiquitous blood pressure monitoring via pulse transit time: theory and practice, IEEE Trans. Biomed. Eng. 2015, 62(8):1879-1901.
- Ding X.; Yan B. P.; Zhang Y. T.; et al. Pulse transit time based continuous cuffless blood pressure estimation: a new extension and a comprehensive evaluation, Rep. 2017, 7(1):11554.
- Lin H.; Xu W.; Guan N.; et al. Noninvasive and continuous blood pressure monitoring using wearable body sensor networks, IEEE Intell. Syst. 2015, 30(6):38-48.
- Bilo G.; Zorzi C.; Munera J. E. O.; et al. Validation of the somnotouch-NIBP noninvasive continuous blood pressure monitor according to the European society of hypertension international protocol revision 2010, Blood Press. Monit. 2015, 20(5):291-294.
- Wong Y. M.; Poon C. Y.; Zhang Y. T.; An evaluation of the cuffless blood pressure estimation based on pulse transit time technique: a half year study on normotensive subjects, Eng. 2009, 9(1):32-38.
- Zheng Y.; Poon C. C.; Yan B. P.; et al. Pulse arrival time based on cuff-less and 24-H wearable blood pressure monitoring and its diagnostic value in hypertension, Med. Syst. 2016, 40(9):1-11.
- Kim S. H.; Song J. G.; Park J. H.; et al. Beat-to-beat tracking of systolic blood pressure using noninvasive pulse transit time during anesthesia induction in hypertensive patients, Analg. 2013, 116(1):94-100.
- Monte-Moreno E. Non-invasive estimate of blood glucose and blood pressure from a photoplethysmograph by means of machine learning techniques, Intell. Med. 2011, 53(2):127-138.
- Pandian P. S.; Mohanavelu K.; Safeer K. P.; et al. Smart Vest: wearable multi-parameter remote physiological monitoring system, Eng. Phys. 2008, 30(4):466-477.
- Chen W.; Kobayashi T.; Ichikawa S.; et al. Continuous estimation of systolic blood pressure using the pulse arrival time and intermittent calibration, Biol. Eng. Comput. 2000, 38(5):569-574.
- Nabeel P.; Joseph J.; Sivaprakasam M. Single-source PPG based local pulse wave velocity measurement: A potential cuffless blood pressure estimation technique, Mea. 2017, 38(12):2122-2140.
- Zhang Q.; Chen X.; Fang Z.; et al. Cuff-less blood pressure measurement using pulse arrival time and a Kalman filter, Microeng. 2017, 27(2):024002.
- “American National Standard for Electronic or automated sphygmomanometers,” AAMI, 2002, ANSI/AAMI SP 10 2002.
- Liu Q.; Yan B. P.; Yu C. M.; et al. Attenuation of systolic blood pressure and pulse transit time hysteresis during exercise and recovery in cardiovascular patients, IEEE Trans. Biomed. Eng. 2014, 61(2):346.
This entry is adapted from the peer-reviewed paper 10.3390/s20082205