The nasolabial angle (NLA) is one of the key factors to be studied in an orthodontic diagnosis for the aesthetics of the nose and facial profile.
- nasolabial angle
- soft-tissue profile
- facial profile
- orthodontic profile
- rapid palatal expansion
- orthognathic surgery
- headgear treatment
- hyaluronic acid
- hyaluronic acid filler
1. Introduction
The evaluation of the facial profile is an important factor in any current orthodontic diagnosis, considering that an extreme advancement or retreat in the position of the upper lip or chin can determine the worsening of the patient’s profile and aesthetic results. There are many factors to consider to preserve the aesthetics of the facial profile: the nasolabial angle (NLA), the nasal prominence, the position of the upper and lower lip and the depth of the chin-labial sulcus. The NLA is one of the key factors to be considered in an orthodontic diagnosis as guidance for the aesthetics of the nose and facial profile. It is defined as the angle formed by the two lines passing through the lower edge of the nose (the columella) and the edge of the upper lip (as shown in Figure 1). As described in literature, the ideal nasolabial angle ranges from 90° and 95° for males and 95–115° for females, although these values may vary among the various phenotypical groups (races).
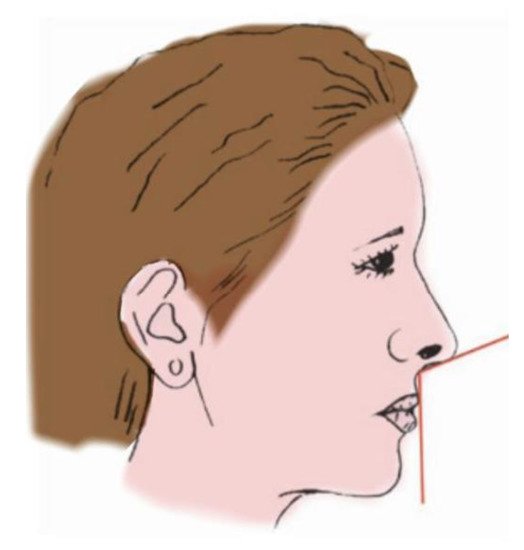
Figure 1. The nasolabial angle (NLA).
In general, the NLA values are increased in Asian populations, showing a flatter profile and a more obtuse angle in comparison with Caucasian populations or with African populations [1]. Dental extractions in orthodontics are often recommended in order to gain space in the case of severe or moderate crowding or for the camouflage of consolidated skeletal malocclusions. However, the orthodontic diagnosis and decision of whether or not to treat a patient with extractions remains controversial. As for the NLA modification, many theories exist. Some orthodontists believe that extractions worsen the patient’s soft tissue profile by making it too flat. Therefore, they prefer to follow a conservative approach, creating minimally invasive treatments that allow the recovery of space within the arch, such as: dental stripping, expansion of the dental arches and distalization [2]. On the other hand, there are orthodontists who believe that extraction represents the right therapeutic strategy. According to this approach, extraction does not worsen the profile, indeed in some cases it may improve it, by increasing the NLA values [3]. Furthermore, extractions often have a strong positive impact on factors such as: vertical dimension, treatment stability, width of the arches, facial convexity and perioral tissues [4]. The drawback of extractions is that they may result in a bi-retruded or flat profile, narrow dental arches, or an increase in the width of buccal corridors, which, in non-extractive cases, may result in an instability of the occlusal contacts with the risk of relapse. Additionally, in borderline cases, this may lead to a biprotruded profile [5]. Therefore, the customary extraction of four premolars is contraindicated in cases of a deep bite and horizontal growth pattern, as it will lead to the loss of the vertical dimension, further retrusion of the lower third of the face and an increase in NLA values [6]. Among non-extractive protocols that may influence the NLA, there are the distalization of the upper molars and the use of mandibular advancement devices (MAD), for the treatment of class II malocclusions [7][8]. Treatments such as the Delaire face mask for maxillary advancement, orthodontic camouflage and orthognathic surgery represent valid non-extractive therapeutic options for the treatment of patients with skeletal class III [9][10][11]. Rapid palatal expansion (RPE) is an effective treatment option for the correction of transverse maxillary discrepancies, which produces changes in the soft tissues related to an increase in the size of the nasal soft tissues and bone bases. In this systematic review of the relevant literature, we will analyze how these various therapeutic procedures can affect the NLA values, including non-surgical rhinoplasty with a hyaluronic acid filler as a non-orthodontic treatment option to improve the patients’ soft tissue profile, mostly in patients who do not want to undergo orthodontic or surgical treatment or in those cases in which the orthodontic treatment does not obtain the desired results in terms of aesthetics of the facial profile.
2. Discussion
2.1. NLA in Extraction vs. Non-Extraction Cases
There were 10 articles addressing the variations of the NLA by comparing the extractive cases to the non-extractive cases, with a total of 2845 patients divided into the various study groups, including 428 females and 696 males, with an average age of 14.62 years. Among these, four authors found a statistically significant increase in post-treatment NLA values ranging from 2.4° to 9.410° in class I patients treated with extractions of the first four or second premolars, and in patients with maxillary bi-protrusion treated with extractions of all four first premolars. Almurtadha et al. recorded a retraction in the position of the upper and lower lips and the consequent increase in the NLA with an average difference of 4.92° after the orthodontic treatment of these patients who had extractions. The authors explained that the retraction of the lips, and therefore an increase of the NLA, is due to the retraction of the upper and lower anterior teeth as they move backwards to occupy the extractive spaces. On the other hand, there is no change in the NLA in those cases with extractive orthodontics where the procedure indicated aimed at the resolution of dentoalveolar crowding or a camouflage of mild skeletal malocclusions. The authors stated that a 2 mm change in lip retraction is enough to make the profile look worse or better [3]. Similar results to the previous study were reported by Alqahtani et al., who registered a statistically significant increase both in the NLA and in the length of the upper lip, as related to a retraction of the upper and lower incisors—plus a retro-inclination—in biprotruded patients treated with extractions of the first upper and lower premolars. They also report a decrease of 1.1 mm post treatment in the exposure of the upper incisors [12]. Additionally, Konstantonios et al. reported a significant increase in the NLA in cases involving the extraction of the four upper and lower first premolars compared to non-extractive cases. However, there was no significant increase in the NLA’s values obtained in cases where only two premolars were extracted. The retraction of the lips and the increase in the NLA’s values were associated with a retraction of the upper or lower incisors. This means that extractions can have a low impact on the facial profile if the retraction of the anterior sector is minimal, as it occurs in cases where the extractive spaces are closed by mesialization of the posterior sectors.
There was also a significant association between the NLA values and the patients’ age, as a greater increase in the NLA was achieved in older patients than in those youngsters who were still growing. The cause of this association is reported to be related to the growth of the nasal spine or of the lips during the patient’s growth [4]. A significant increase in NLA of 9.410°—with subsequent labial retraction in class I borderline patients—was recorded in the study of Yashwant, Ravi and Arumugam, which supports the results reported by the previous authors [5].
Four studies reported no statistically significant values for the NLA by comparing the results obtained among a group of patients undergoing extractions of the four premolars and a non-extractive group, among these: Freitas et al. in their study on 20 class I patients, Iared et al. in their study conducted on 195 patients, and Kirschneck et al. in their study on 50 patients [6][13][14]. Omar et al., as well, registered no statistically significant NLA values, but in their article they compared the NLA values obtained in two extraction groups, one with the extraction of the four first premolars and one with the extraction of four s premolars [15].
Two more studies reported a statistically significant increase of NLA values in the treatment of extractive cases. One of these studied the results obtained with skeletal anchorage using orthodontic mini screws. Liu et al. obtained a 3.52° increase in NLA values on biprotruded patients [16]. Conversely, Jo et al. in their scientific article studied variations in the NLA between a group undergoing extractions and a group undergoing molar distalization and they reported a significant increase in the values of the NLA in both study groups. Furthermore, they recommended the extraction of the four premolars in patients with class II malocclusion who required further retraction of the anterior sectors and improvement of the soft tissues profile [2].
2.2. NLA in Treatment of Class II Malocclusion
Regarding the variations in the NLA as recorded in studies concerning class II malocclusions, there were no statistically significant differences when patients were treated with functional orthodontic, orthopedic devices or with brackets. Xuan et al. reported a correlation between changes in the NLA and the posterior occlusal plane in patients with class II malocclusion [17]. Hourfar et al. recorded a greater increase in the NLA in patients treated with Herbst (118.64°) compared to patients treated with removable appliances for mandibular advancement (114.78°) [7]. Vilanova et al. did not find significant variations in NLA values in their study comparing the effects of two different devices (Distal Jet and Jones Jig, respectively) used for the treatment of class II malocclusion, with a control group of untreated patients [8].
The results for two articles evaluating the variations of the NLA obtained after treatment with extraoral tractions were contradictory. Papageorgiou et al. did not record statistically significant changes in NLA values after the “short-term” (as defined by the authors) treatment of 930 patients with extraoral tractions. The effects achieved on the NLA were associated with the degree of protrusion of the maxilla before receiving orthodontic treatment and there was no relationship with the modification of the longitudinal growth recorded in these patients. Moreover, there was no statistically significant difference between the three types of extraoral tractions studied, which were, respectively, high traction, cervical traction, and combined traction [18]. However, Park et al. did record differences that were statistically significant in their study of 44 subjects comparing patients with class II malocclusions treated with extraoral cervical traction to patients treated with C-palatal plane on orthodontic mini screws [19]. Although the results obtained by these two studies were contradictory, it should be noted that 930 patients were included in the study by Papageorgiou et al., a much larger sample of orthodontic patients with class II malocclusion than the 44 patients treated by Park et al. Furthermore, it should be considered that the first study was about growing patients, while the second one dealt with adult patients.
2.3. NLA in Treatment of Class III Malocclusion
In this systematic literature review, only two articles evaluated the effects produced on the NLA by orthodontic treatment protocols for class III malocclusion. Xu et al. reported a statistically significant decrease in the NLA values of 5.629° in patients treated with protocols that included a protraction of the maxilla. They also reported changes in the position of the upper and lower lip [10]. Conversely, Celikoglu et al. reported no statistically significant difference between two groups of patients treated with a “mini maxillary protractor” and with rapid palatal expansion plus face mask. The slight increase in NLA values recorded in patients treated with “mini maxillary protractor” was certainly due to the dental and skeletal effects on the upper jaw, resulting in a better support to the upper lip, which was more advanced [9].
2.4. NLA after Rapid Palatal Expansion
Torun is the only author who dealt with the effects of rapid palatal expansion, reporting a slight and not statistically significant decrease in NLA values [20].
2.5. NLA after Orthognatic Surgery
No statistically significant changes in NLA values were reported in the four studies on orthognathic surgery, all performed by Lefort I. Shmuly et al., which found a decrease of 3.78° in the NLA in their study of variation in the NLA, in the upper lip and in the nasal base in patients who underwent upper jaw advancement surgery. However, the authors were unable to find a correlation between a decrease in the NLA and the amount of maxillary advancement [21]. Allar et al. also found a decrease in the NLA and an advancement of the upper lip in patients undergoing maxillary advancement surgery of ≥6 mm, but not enough to be statistically significant [22]. The results obtained from the study by Ghassemi et al. on mandibular advancement were in line with the other authors [23]. Furthermore, the same authors (Ghassemi et al.), in their study on orthognathic surgery, compared the effects obtained on soft tissues after surgical treatment with mandibular repositioning and advancement of the maxilla, recording an increase in the NLA in both groups. In the case of mandibular advancement, it was due to the change in tension of the upper lip, while in the cases of mandibular advancement, it was due to the decrease in nasal prominence. Despite the data reported, the values recorded did not have a statistical significance [11].
2.6. NLA and Hyaluronic Acid Fillers
As for the variation in the NLA, after non-surgical rhinoplasty treatment with a hyaluronic acid filler, four articles were included in this systematic review of the literature, and they all showed statistically significant results in increasing the NLA. These medical aesthetic operations are requested by patients who show a depressed section in the middle third of the face, due to the downward rotation of the nasal tip that reduces the NLA [24] For this reason, filler injections to modify the NLA are applied in the area of the columella and of the nasal spine on the nasolabial joint, so as to modify the nasal tip [25]. In all the studies included here, a statistically significant increase in the NLA values was obtained. Santorelli et al. reported that post-treatment, the NLA average values were 88.5° with an average increase of 3.2° ± 2.6° [26]. Xiong et al. reported post-treatment NLA average values of 107.93° [24]. Youn et al. compared patients who underwent a total increase of nose proportions to patients who underwent filler injections only in the bridge of the nose. As a result, they reported that post-treatment, the NLA average value was 96.8° with an average increase of 9.4° ± 4.5° [25]. Rho et al. reported average post-treatment NLA values of 95° with an average increase of 3.79° ± 8.71° [1]. The statistically significant results obtained by all the authors who treated the increase of the NLA with filler allow us to recognize the validity of the technique that can be used as a post orthodontic treatment to increase the NLA by altering the nasal tip.
This entry is adapted from the peer-reviewed paper 10.3390/app11062531
References
- Rho, N.K.; Park, J.Y.; Youn, C.S.; Lee, S.-K.; Kim, H.S. Early Changes in Facial Profile Following Structured Filler Rhinoplasty: An Anthropometric Analysis Using a 3-Dimensional Imaging System. Dermatol. Surg. 2017, 43, 255–263.
- Jo, S.Y.; Bayome, M.; Park, J.; Lim, H.J.; Kook, Y.-A.; Han, S.H. Comparison of treatment effects between four premolar extraction and total arch distalization using the modified C-palatal plate. Korean J. Orthod. 2018, 48, 224–235.
- AlMurtadha, R.H.; Alhammadi, M.S.; Fayed, M.M.; Abou-El-Ezz, A.; Halboub, E. Changes in Soft Tissue Profile After Orthodontic Treatment With and Without Extraction: A Systematic Review and Meta-analysis. J. Évid. Based Dent. Pract. 2018, 18, 193–202.
- Konstantonis, D.; Vasileiou, D.; Papageorgiou, S.N.; Eliades, T. Soft tissue changes following extraction vs. nonextraction orthodontic fixed appliance treatment: A systematic review and meta-analysis. Eur. J. Oral Sci. 2018, 126, 167–179.
- Yashwant, V.A.; Arumugam, E. Comparative evaluation of soft tissue changes in Class I borderline patients treated with extraction and nonextraction modalities. Dent. Press J. Orthod. 2016, 21, 50–59.
- Kirschneck, C.; Proff, P.; Reicheneder, C.; Lippold, C. Short-term effects of systematic premolar extraction on lip profile, vertical dimension and cephalometric parameters in borderline patients for extraction therapy—a retrospective cohort study. Clin. Oral Investig. 2016, 20, 865–874.
- Hourfar, J.; Lisson, J.A.; Gross, U.; Frye, L.; Kinzinger, G.S.M. Soft tissue profile changes after Functional Mandibular Advancer or Herbst appliance treatment in class II patients. Clin. Oral Investig. 2017, 22, 971–980.
- Vilanova, L.; Janson, G.; Patel, M.P.; Reis, R.S.; Castillo, A.A.-D.; Henriques, J.F.C. Class II malocclusion treatment effects with Jones Jig and Distal Jet followed by fixed appliances. Angle Orthod. 2017, 88, 10–19.
- Celikoglu, M.; Yavuz, I.; Ünal, T.; Oktay, H.; Erdem, A. Comparison of the soft and hard tissue effects of two different protraction mechanisms in class III patients: A randomized clinical trial. Clin. Oral Investig. 2015, 19, 2115–2122.
- Xu, F.-Y.; Kwon, T.-G.; Rong, H.; Kyung, H.-M.; Bing, L.; Wu, X.-P. Morphological Changes of Skeletal Class III Malocclusion in Mixed Dentition with Protraction Combined Activities. Int. J. Morphol. 2018, 36, 430–434.
- Ghassemi, M.; Hilgers, R.-D.; Fritz, U.; Modabber, A.; Ghassemi, A. Maxillary advancement versus mandibular setback in class III dentofacial deformity: Are there any differences in aesthetic outcomes? Int. J. Oral Maxillofac. Surg. 2017, 46, 483–489.
- Alqahtani, N.D.; Alshammari, R.; Almoammar, K.; Almosa, N.; Almahdy, A.; AlBarakati, S.F. Post-orthodontic cephalometric variations in bimaxillary protrusion cases managed by premolar extraction—A retrospective study. Niger. J. Clin. Pract. 2019, 22, 1530–1538.
- Freitas, B.V.; Rodrigues, V.P.; Rodrigues, M.F.; De Melo, H.V.; Dos Santos, P.C. Soft tissue facial profile changes after orthodontic treatment with or without tooth extractions in Class I malocclusion patients: A comparative study. J. Oral Biol. Craniofacial Res. 2019, 9, 172–176.
- Iared, W.; Da Silva, E.M.K.; Iared, W.; Macedo, C.R. Esthetic perception of changes in facial profile resulting from orthodontic treatment with extraction of premolars. J. Am. Dent. Assoc. 2017, 148, 9–16.
- Omar, Z.; Short, L.; Banting, D.W.; Saltaji, H. Profile changes following extraction orthodontic treatment: A comparison of first versus second premolar extraction. Int. Orthod. 2018, 16, 91–104.
- Liu, Y.; Yang, Z.-J.; Zhou, J.; Xiong, P.; Wang, Q.; Yang, Y.; Hu, Y.; Hu, J.-T. Soft Tissue Changes in Patients With Dentoalveolar Protrusion Treated With Maximum Anchorage: A Systematic Review and Meta-analysis. J. Évid. Based Dent. Pract. 2019, 19, 101310.
- Xuan, J.; Bing, L.; Li, S.-F.; Ma, Y.-N.; Kwon, T.-G.; Wu, X.-P. Morphological Characteristics of Soft Tissue Profile of Angle’s Class II Division I Malocclusion before and after Orthodontic Treatment. Int. J. Morphol. 2018, 36, 26–30.
- Papageorgiou, S.N.; Kutschera, E.; Memmert, S.; Gölz, L.; Jäger, A.; Bourauel, C.; Eliades, T. Effectiveness of early orthopaedic treatment with headgear: A systematic review and meta-analysis. Eur. J. Orthod. 2016, 39, 176–187.
- Park, C.O.; Sa’Aed, N.L.; Bayome, M.; Park, J.H.; Kook, Y.-A.; Park, Y.-S.; Han, S.H. Comparison of treatment effects between the modified C-palatal plate and cervical pull headgear for total arch distalization in adults. Korean J. Orthod. 2017, 47, 375–383.
- Torun, G.S. Soft Tissue Changes in the Orofacial Region after Rapid Maxillary Expansion: A Cone Beam Computed Tomography Study. J. Orofac. Orthop. Fortschr. Kieferorthopädie 2017, 78, 193–200.
- Shmuly, T.; Chaushu, G.; Allon, D.M. Does Maxillary Advancement Influence the Nasolabial Angle? J. Craniofacial Surg. 2019, 30, e408–e411.
- Allar, M.L.; Movahed, R.; Wolford, L.M.; Oliver, D.R.; Harrison, S.D.; Thiesen, G.; Kim, K.B. Nasolabial Changes Following Double Jaw Surgery. J. Craniofacial Surg. 2019, 30, 2560–2564.
- Ghassemi, M.; Hilgers, R.-D.; Jamilian, A.; Shokatbakhsh, A.; Hölzle, F.; Fritz, U.; Ghassemi, A. Effect of maxillary advancement on the change in the soft tissues after treatment of patients with class III malocclusion. Br. J. Oral Maxillofac. Surg. 2015, 53, 754–759.
- Xiong, Z.; Jiang, Z.; Liu, K. Midline Volume Filler Injection for Facial Rejuvenation and Contouring in Asians. Aesthetic Plast. Surg. 2019, 43, 1624–1634.
- Youn, S.H.; Seo, K.K. Filler Rhinoplasty Evaluated by Anthropometric Analysis. Dermatol. Surg. 2016, 42, 1071–1081.
- Santorelli, A.; Marlino, S. Non-surgical Rhinoplasty with Hyaluronic acid Fillers: Predictable Results Using Software for the Evaluation of Nasal Angles. Aesthetic Plast. Surg. 2020, 44, 919–926.
