Due to their mechanical properties, ranging from flexible to hard materials, polyurethanes (PUs) have been widely used in many industrial and biomedical applications. PU characteristics, along with their biocompatibility, make them successful biomaterials in short and medium time applications. The most important biomedical applications of PUs include antibacterial surfaces and catheters, blood oxygenators, dialysis devices, stents, cardiac valves, vascular prostheses, bioadhesives/surgical dressings/pressure sensitive adhesives, drug delivery systems, tissue engineering scaffolds and electrospinning, nerve generation, pacemaker lead insulation and coatings for breast implants. The diversity of polyurethane properties due to the ease of bulk and surface modification plays a vital role in their applications.
- polyurethanes
- biomedicine
- resin-based dental composites
- prosthetic resins
- electrospinning
- bioadhesives
- carriers
- cardiac valves
- scaffolds
- coatings
PUs are primarily obtained from the petrochemical refining of coals and crude oil as raw materials [1][2], using by-products of plant material derived either from crops or their residues or from forestry biomass [3][4].
These materials, known under the general term of lignocellulosic biomass, are used to extract the proper raw material for PUs [3]. Lignin, one of the most sustainable raw materials used to produce polymers, widely used in paper and pulp industries, is the most frequently used natural polymer after cellulose [5], due to the fact that it is readily available in bulk quantities and inexpensive [3]. PU foams, known for their versatile mechanical properties, thermal insulation and low volumetric weight [3][6], are also produced through the re-polymer approach, based on lignin functionalization with diisocyanate, resulting in an electrophilic precursor polymer [7][8].
The initial stage in the manufacturing process of PUs implies either the use of a polymer, or a low-molecular-weight pre-polymer liquid, a monomer. The results of the main reactions in PU synthesis are represented by the formation of the carbamate (urethane) linkage. In 1849, Wurtz and Hoffman were the first to discover this linkage after evaluating the reaction between an isocyanate and a hydroxylated compound [9].
Following the accidental discovery of polyaddition for the synthesis of polyurethane out of poly-isocyanates by Otto Bayer in 1937, PUs were widely applied in the industrial field [9][10].
Formed as a result of a polycondensation reaction between an isocyanate (with at least two hydroxyl groups) anda hydroxylated compound (with at least two hydroxyl groups) in the presence of a catalyst, PUs have a wide variety of industrial uses, as footwear, furniture, construction materials, automotive parts, clothing, packaging and others [1][3][9][11] (Figure 1).
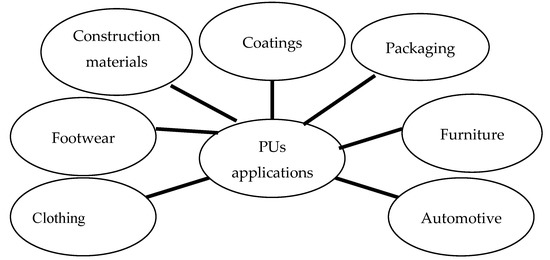
Figure 1. PUs’ applications.
Due totheir mechanical flexibility, combined with their increased tear strength, biocompatibility, biodegradability and tailorable forms, PUs have attracted the attention of biomedical device developers since 1950, when a polyester-urethane foam was first usedas a breast prosthesis coating [12].
In 1959, a newly developed PU foam wasapplied as a bone gap filler and immobilizing agent, followed by a polyester-urethane-based material used in the preparation of heart valves and aortic grafts [9]. Although PUs have excellent mechanical properties and chemical stability, and are easy to process, they are usually hydrophobic. Thus, they must be surface modified in order to adapt for biomedical applications.
The applications of polymers in biomedicine include orthopedics, ophthalmology, surgery, cardiology, dentistry, dialysis, and controlled delivery systems [13].
Polymers used in biomedicine need to meet certain requirements, such as biocompatibility, bioacceptability and biodegradability, and have to be modified either chemically or physically in order to achieve the desired properties [9]. When considering the medical field, besides their increased biocompatibility and antithrombogenic effects, PUs are also known to improve cell migration, sustain drug delivery and ensure proper organ reconstruction.
Current biomedical application areas of PUs include antibacterial surfaces and catheters, blood oxygenators, dialysis devices, stents, cardiac valves, vascular prostheses, bioadhesives/surgical dressings/pressure-sensitive adhesives, drug delivery systems, tissue engineering scaffolds and electrospinning, nerve generation, pacemaker lead insulation and coatings for breast implants (Figure 2) [14][15][16].
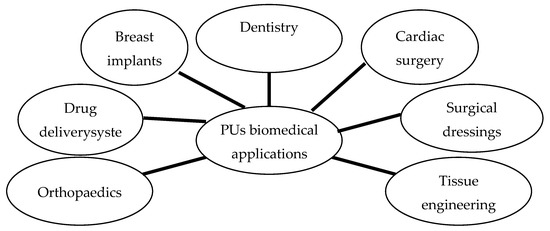
Figure 2. Biomedical applications of PUs.
Due to the multiple and extensive development of the PUs, our approach is not to be considered an exhaustive one. In this regard, the aim of this narrative review is to present the key structural properties of polyurethanes and their applications in biomedicine. In this regard, the current paper is bringing new insights to systematized knowledge in this area.
Due to their mechanical features, ranging from rigid to flexible, PUs are present in a variety of domains, including the biomedical field [17].
The morphology of polyurethane, based on two structural phases—hard and soft segments—ensures high mechanical resistance, determined by the hard segment, and elastomeric behaviour, ensured by the soft segment. Therefore, the singular molecular structure provides different properties, such as elasticity, resistance to abrasion, durability, chemical stability and facile processability [9][18].
A particular category of polymers are reactive polymers (PUs included), widely used in the chemical industry. These types of polymers are able to determine different chemical reactions at the chain levels, resulting in polymer changes [19][20]. Their preparation implies two major procedures, either performing reactions on polymer chains, or adding a monomer containing a reactive group [19].
Despite their great benefits in chemical industry and technology, polymers sometimes represent risk factors for the environment. From this point of view, microplastics are a source of marine and atmospheric pollutants as well as media for the attachment of hydrophobic organic pollutants [21][22][23][24]. It appears that PU and polyamide display the most increased ability for bisphenol A sorption. Compared to other polymers such as polyethylenes, polypropylenes, or poly(vinyl chloride), in case of both PU and polyamide, sorption is almost irreversible. Microplastics thus represent environmental risk factors, due to their role as transportation vectors for bisphenol A [21]16. However, the chemical industry currently benefits from the fabrication of different polymeric structures and materials that are regarded as environment-friendly.
Due to their extensive structure and diverse properties, PUs are considered among the most bio- and blood-compatible materials. Properties such as durability, elasticity, elastomer-like character, fatigue resistance, compliance, acceptance and tolerance in the body during healing are often also associated with PUs [18]. These materials play a major role in the development of many medical devices, ranging from catheters to total artificial hearts.Their applications include artificial organs, tissue replacement and augmentation, performance-enhancing coatings, drug delivery systems and many others [25]. Due to their usage in a wide range of domains, polymeric structures represent a major challenge considering biodegradability and biocompatibility.
To increase biostability, novel PUs with a siloxane segment, polycarbonate polyurethanes, and nanocomposite polyurethanes were developed [26]. PUs with a siloxane segment are prone to calcification during continuous in-vivo exploitation [27]. Nanocomposite polyurethanes are free of these disadvantages and have been included into clinical trials [28][29]. On the other hand, some authors reported a low rate of patency on in-vivo testing of nanocomposite polyurethane small-caliber vascular grafts implanted into the ovine carotid artery [30].
Literature data clearly indicate the potential of PUs to complement or substitute degradable polymers, such as polyester, in the replacement of damaged tissues or organs, as well as in nanomedicine, as they show superior drug encapsulation efficiency and enhanced capability to target specific tissue compartments [31][32].
Blending allows the tailoring and modulation of the properties of selected polymers. Blends are oftenfabricated by electrospinning. Electrospinning is the most promising and simple technique for manufacturing vascular grafts of polymeric materials.
The new generation of vascular PU grafts produced by electrospinning closely meets the requirements of an ideal prosthesis [13][33][34][35].
This method allows the diameter, composition, and porosity of nanofiber scaffolds to be controlled and multilayered vascular grafts, similar to the native vessels in their physical and biological properties, to be designed [36][37].
All these also contribute to graft biostability and biocompatibility, making them closer to ‘‘ideal’’ variants [38][39].
Studies show that electrospun nanocomposites treated with basil oil and titanium dioxide particles exhibit a lower cellular toxicity compared to pristine polymers [40]. Electrospun composites based on PU with added peppermint and copper sulphate used to fabricate scaffolds showed low toxicity levels and improvement of blood clotting time and seem to be more effective compared to pristine PU due to the increased cell viability [31][32].
Hospital infections represent a great challenge for current medicine, as they are responsible for increased morbidity and mortality worldwide. Antibacterial effects and super-hydrophobic properties are shown to be induced on the surface of thermoplastic PU sheets [41]. When using a pure PVC film, bacterial adhesion showed a significant decrease in case of S. aureus and E. coli bacteria [41]. PU and silicone with incorporated copper nanoparticles have shown antimicrobial activity against infectious agents such as Staphylococcus aureus and Escherichia coli. Incorporated polymers have proved their efficacy in reducing bacterial contamination in the case of bed rails, push plates and overbed tables [42].
The applications of PUs in biomedicine are continuously extending, with new research being published and demonstrating that the potentials of PUs are far from fully exploited.
This entry is adapted from the peer-reviewed paper 10.3390/polym12051197
References
- Colombo, A.; De Bortoli, M.; Pecchio, E.; Schauenburg, H.; Schlitt, H.; Vissers, H. Chamber testing of organic emission from building and furnishing materials. Sci. Total Environ. 1990, 91, 237–249.
- Gama, N.V.; Ferreira, A.; Barros-Timmons, A. Polyurethane foams: Past, present, and future. Materials 2018, 11, 1841.
- Zieglowski, M.; Trosien, S.; Rohrer, J.; Mehlhase, S.; Weber, S.; Bartels, K.; Siegert, G.; Trellenkamp, T.; Albe, K.; Biesalski, M. Reactivity of isocyanate-functionalized lignins: A key factor for the preparation of lignin-based polyurethanes. Front. Chem. 2019, 7, 562.
- Furtwengler, P.; Avérous, L. Renewable polyols for advanced polyurethane foams from diverse biomass resources. Polym. Chem. 2018, 9, 4258–4287.
- Boerjan, W.; Ralph, J.; Baucher, M. Lignin bionthesis. Annu. Rev. Plant Biol. 2003, 54, 519–546.
- A. K. Agrawal; B. Singh; Y. S. Kashyap; M. Shukla; B. S. Manjunath; S. C. Gadkari; Gamma-irradiation-induced micro-structural variations in flame-retardant polyurethane foam using synchrotron X-ray micro-tomography. Journal of Synchrotron Radiation 2019, 26, 1797-1807, 10.1107/s1600577519009792.
- Chauhan, M.; Gupta, M.; Singh, B.; Singh, A.; Gupta, V. Effect of functionalized lignin on the properties of lignin–isocyanate prepolymer blends and composites. Eur. Polym. J. 2014, 52, 32–43.
- Gómez-Fernández, S.; Ugarte, L.; Calvo-Correas, T.; Peña-Rodríguez, C.; Corcuera, M.A.; Eceiza, A. Properties of flexible polyurethane foams containing isocyanate functionalized kraft lignin. Ind. Crop Prod. 2017, 100, 51–64.
- Alves, P.; Ferreira, P.; Gil, M. Biomedical polyurethanes-based materials. In Polyurethane: Properties, Structure and Applications; Cavaco, L.I., Melo, J.A., Eds.; Nova Publishers: New York, NY, USA, 2012; pp. 1–27.
- Bellis, M.; The History of Polyurethane-Otto Bayer. ThoughtCo. 2020. Available online: Thoughtco.com/history-of-polyurethane-otto-bayer-4072797 (accessed on 8 May 2020).
- Mellette, M.P.; Bello, D.; Xue, Y.; Yost, M.; Bello, A.; Woskie, S.; Testing of disposable protective garments against isocyanate permeation from spray polyurethane foam insulation. Ann. Work Expo. Health 2018, 62, 754–764, .
- Takacs, E.S.; Vlachopoulos, J.; Biobased, biodegradable polymers for biomedical applications: Properties and processability. Plast. Eng. 2008, 64, 28–33, .
- Alessandra Bianco; Manuela Calderone; Ilaria Cacciotti; Electrospun PHBV/PEO co-solution blends: Microstructure, thermal and mechanical properties. Materials Science and Engineering: C 2013, 33, 1067-1077, 10.1016/j.msec.2012.11.030.
- Venkateshaiah, A.; Padil, V.V.; Nagalakshmaiah, M.; Waclawek, S.; Černík, M.; Varma, R.S. Microscopic techniques for the analysis of micro and nanostructures of biopolymers and their derivatives. Polymers 2020, 12, 512.
- Nguyen, T.P.; Nguyen, Q.; Nguyen, V.-H.; Le, T.-H.; Huynh, V.; Vo, D.-V.N.; Trinh, Q.T.; Kim, S.Y.; Van Le, Q. Silk fibroin-based biomaterials for biomedical applications: A review. Polymers 2019, 11, 12.
- Moura, D.; Souza, M.; Liverani, L.; Rella, G.; Luz, G.; Mano, J.F.; Boccaccini, A. Development of a bioactive glass-polymer composite for wound healing applications. Mater. Sci. Eng. C 2017, 76, 224–232.
- Guangyu Zhang; Yumin Wu; Weisheng Chen; Dezhi Han; Xiaoqi Lin; Gongchen Xu; Qinqin Zhang; Open-Cell Rigid Polyurethane Foams from Peanut Shell-Derived Polyols Prepared under Different Post-Processing Conditions.. Polymers 2019, 11, 1392, 10.3390/polym11091392.
- Cooper, S.L.; Jianjun, G. Advances in Polyurethane Biomaterials, 1st ed.; Woodhead Publishing: Sawston, UK, 2016; pp. 3–16.
- Chen, Y.-C.; Huang, C.-H.; Liu, Y.-L. Polymerization of meldrum’s acid and diisocyanate: An effective approach for preparation of reactive polyamides and polyurethanes. ACS Omega 2019, 4, 7884–7890.
- Lu, D.; Zhou, J.; Hou, S.; Xiong, Q.; Chen, Y.; Pu, K.; Ren, J.; Duan, H. Functional macromolecule-enabled colloidal synthesis: From nanoparticle engineering to multifunctionality. Adv. Mater. 2019, 31, e1902733.
- Liu, X.; Shi, H.; Xie, B.; Dionysiou, D.D.; Zhao, Y. Microplastics as both a sink and a source of bisphenol a in the marine environment. Environ. Sci. Technol. 2019, 53, 10188–10196.
- Zocchi, M.; Sommaruga, R. Microplastics modify the toxicity of glyphosate on Daphnia magna. Sci. Total Environ. 2019, 697, 134194.
- Peez, N.; Becker, J.; Ehlers, S.M.; Fritz, M.; Fischer, C.B.; Koop, J.H.E.; Winkelmann, C.; Imhof, W. Quantitative analysis of PET microplastics in environmental model samples using quantitative 1H-NMR spectroscopy: Validation of an optimized and consistent sample clean-up method. Anal. Bioanal. Chem. 2019, 411, 7409–7418.
- Liu, K.; Wang, X.; Wei, N.; Song, Z.; Li, D. Accurate quantification and transport estimation of suspended atmospheric microplastics in megacities: Implications for human health. Environ. Int. 2019, 132, 105127.
- Richard J. Zdrahala; Ivanka J. Zdrahala; Biomedical applications of polyurethanes: a review of past promises, present realities, and a vibrant future.. Journal of Biomaterials Applications 1999, 14, 67-90, 10.1177/088532829901400104.
- A. A. Gostev; Andrei A. Karpenko; Pavel P. Laktionov; Polyurethanes in cardiovascular prosthetics. Polymer Bulletin 2018, 75, 4311-4325, 10.1007/s00289-017-2266-x.
- G M Bernacca; T G Mackay; R Wilkinson; D.J. Wheatley; Calcification and fatigue failure in a polyurethane heart value.. Biomaterials 1995, 16, 279–285, .
- Sandip Sarkar; Gaetano Burriesci; Adam Wojcik; Nicholas Aresti; George Hamilton; Alexander Seifalian; Manufacture of small calibre quadruple lamina vascular bypass grafts using a novel automated extrusion-phase-inversion method and nanocomposite polymer. Journal of Biomechanics 2009, 42, 722-730, 10.1016/j.jbiomech.2009.01.003.
- Igor V. Khudyakov; David R. Zopf; Nicholas J. Turro; Polyurethane Nanocomposites. Designed Monomers and Polymers 2009, 12, 279-290, 10.1163/156855509x448253.
- Ahmed, M.; Hamilton, G.; The performance of a small-caliber graft for vascular reconstructions in a senescent sheep model. Biomaterials 2014, 35, 9033–9040, .
- Susanna Sartori; Valeria Chiono; Chiara Tonda-Turo; Clara Mattu; Ciardelli Gianluca; Biomimetic polyurethanes in nano and regenerative medicine.. Journal of Materials Chemistry B 2014, 2, 5128-5144, 10.1039/c4tb00525b.
- Hong, Y. Electrospun fibrous polyurethane scaffolds in tissue engineering. In Advances in Polyurethane Biomaterials; Cooper, S.L., Guan, J., Eds.; Woodhead Publishing: Cambridge, UK, 2016; pp. 543–559.
- Miguel, S.P.; Figueira, D.R.; Simões, D.; Ribeiro, M.P.; Coutinho, P.; Ferreira, P.; Correia, I.J. Electrospun polymeric nanofibres as wound dressings: A review. Colloids Surf. B 2018, 169, 60–71.
- Cacciotti, I.; Fortunati, E.; Puglia, D.; Kenny, J.M.; Nanni, F. Effect of silver nanoparticles and cellulose nanocrystals on electrospun poly(lactic) acid mats: Morphology, thermal properties and mechanical behavior. Carbohydr. Polym. 2014, 103, 22–31.
- Cacciotti, I.; House, J.N.; Mazzuca, C.; Valentini, M.; Madau, F.; Palleschi, A.; Straffi, P.; Nanni, F. Neat and GNPs loaded natural rubber fibers by electrospinning: Manufacturing and characterization. Mater. Des. 2015, 88, 1109–1118.
- Goh, Y.F.; Shakir, I.; Hussain, R. Electrospun fibers for tissue engineering, drug delivery, and wound dressing. J. Mater. Sci. 2013, 48, 3027–3054.
- Cacciotti, I.; Calderone, M.; Bianco, A. Tailoring the properties of electrospun PHBV mats: Co-solution blending and selective removal of PEO. Eur. Polym. J. 2013, 49, 3210–3222.
- Sell, S.A.; McClure, M.J.; Garg, K.; Wolfe, P.S.; Bowlin, G.L. Electrospinning of collagen/biopolymers for regenerative medicine and cardiovascular tissue engineering. Adv. Drug Deliv. Rev. 2009, 61, 1007–1019.
- Ishii, O.; Shin, M.; Sueda, T.; Vacanti, J.P. In vitro tissue engineering of a cardiac graft using a degradable scaffold with an extracellular matrix–like topography. J. Thorac. Cardiovasc. Surg. 2005, 130, 1358–1363.
- Mani, M.P.; Jaganathan, S.K.; Faudzi, A.A.M.; Sunar, M.S.; Engineered electrospun polyurethane composite patch combined with Bi-functional components rendering high strenght for cardiac tissue engineering. Polymers 2019, 11, 705, .
- Javad Seyfi; Mahyar Panahi-Sarmad; Afrouz OraeiGhodousi; Vahabodin Goodarzi; Hossein Ali Khonakdar; Azadeh Asefnejad; Shahrokh Shojaei; Antibacterial superhydrophobic polyvinyl chloride surfaces via the improved phase separation process using silver phosphate nanoparticles. Colloids and Surfaces B: Biointerfaces 2019, 183, 110438, 10.1016/j.colsurfb.2019.110438.
- Sandeep K. Sehmi; Sacha Noimark; Jonathan Weiner; Elaine Allan; Alexander J. MacRobert; Ivan P. Parkin; Potent Antibacterial Activity of Copper Embedded into Silicone and Polyurethane. ACS Applied Materials & Interfaces 2015, 7, 22807-22813, 10.1021/acsami.5b08665.
