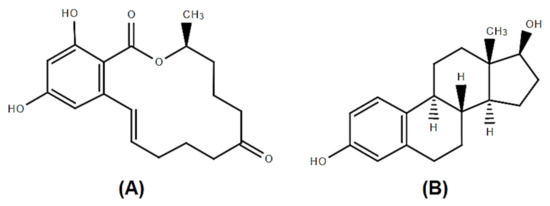
Zearalenone (ZEA) is an estrogenic fusariotoxin, being classified as a phytoestrogen, or as a mycoestrogen. ZEA and its metabolites are able to bind to estrogen receptors, 17β-estradiol specific receptors, leading to reproductive disorders which include low fertility, abnormal fetal development, reduced litter size and modification at the level of reproductive hormones especially in female pigs. ZEA has also significant effects on immune response with immunostimulatory or immunosuppressive results. This review presents the effects of ZEA and its derivatives on all levels of the immune response such as innate immunity with its principal component inflammatory response as well as the acquired immunity with two components, humoral and cellular immune response. The mechanisms involved by ZEA in triggering its effects are addressed.
- zearalenone
- cell immunity
- humoral immunity
1. Zearalenone
2. Effect of ZEA on Gut Immunity
3. Effect of ZEA on Innate Immune Response
4. Effect of Zearalenone on Adaptive Immune Response
4.1. Effect of Zearalenone on Humoral Immune Response
| Effect (s) | Species/Cell Type | Dose/Time of ZEA Administration |
References |
|---|---|---|---|
| ↑ IgE, ↓ IgM no changes of IgG and IgA |
BALB/c mice female | 20 mg/kg b.w. 14 days |
[38] |
| ↓ IgG, IgA ↑ IgM |
Pregnant rats | 100,150 mg/kg feed 7 days |
[70] |
| ↓ IgG, IgM, IgE no changes of IgA |
Wistar rats female |
0, 1, 5, 30 mg/kg b.w. 36 days |
[72] |
| ↓ Ig A, Ig G | BALB/c mice, female | 40 mg/kg b.w. 48h |
[71] |
| ↓ IgG ↑ Ig M |
Wistar rats male |
2 mg/kg b.w./week 3 weeks |
[69] |
| ↓ Ig G no changes of IgA, IgM |
Prepubertal gilts | 200, 800, 1600 μg/kg feed 14 days |
[73] |
| ↓ IgG, IgM no changes of IgA |
Piglets male |
0.8 mg/kg feed 4 weeks |
[74] |
| ↓ IgG, IgM in serum ↑ IgA in serum |
Kunming mice, female |
30 mg/kg b.w. 12 days |
[75] |
| ↓ IgG in serum no changes on IgA, IgM |
post-weaning female piglets |
1.1-3.2 mg/kg feed 18 days |
[76] |
| no effect of serum IgG, IgM, IgA | B6C3F1 mice | 10 mg/kg feed 6 weeks |
[77] |
| ↓ IgG, IgA, IgM in cell SN | Swine PBMC | 10 mM 7 days |
[19] |
| ↓ IgG ↓ IgM |
BALB/c mice | 5, 10, 15 mg/kg b.w./day 2 weeks |
[66] |
| Effect (s) | Species/Cell Type | Dose/Time of ZEA Administration | References |
|---|---|---|---|
| ↓ B cells producing IgM to SRBC 1 | Wistar rats female |
3 mg/kg b.w. 28 days |
[57] |
| No differences in humoral immune response against SRBC 1 | prepubertal gilts | 0.75 mg/kg feed 21 days |
[81] |
| ↓ Ab titer to porcine parvovirus | Wistar rats | 5 mg/kg b.w. 36 days |
[72] |
| ↓ Ab titer to swine plague | post-weaning female piglets | 1.1–3.2 mg/kg feed 18 days |
[76] |
| No effect on the splenic PFC 2 response to SRBC 1 Delayed hypersensitivity response to keyhole limpet hemocyanin |
B6C3F1 female mice | 10 mg/kg b.w. 2–8 weeks |
[79] |
4.2. Effect of Zearalenone on Cellular Immune Response
| Effect (s) | Species/Cell Type | Dose/Time of ZEA Administration | References |
|---|---|---|---|
| ↓ CD4+, CD8+, CD11c+ in spleen ↓ CD4+, CD8+, F4/80+ and ↑ CD19+ and CD11c+ in the mesenteric lymph nodes ↑TNFα and apoptosis, ↓ IL-6 |
BALB/c mice (female, 7-week-old) |
5,20 mg/kg b.w.2 weeks |
[38] |
| ZEA 100 and 150 mg/kg: ↓ viability of splenocytes ↓ T-cell proliferation Induce histopathological damage in spleen ZEA 150mg/kg: ↑ interleukin IL-6, IL-18 and IL-1β ↓ interferon-γ, TNFα and IL-10 in spleen |
Sprague Dawley Pregnant Rats | 50, 100, 150 mg/kg b.w. 7 days |
[70] |
| disrupt the proliferation of CD4+8+ in peripheral blood cells | Polish Landrace x Polish Large White crossbreeds |
0.5 mg/kg 6 weeks |
[105] |
| ↓ IL-1 in thymus and spleen ↓ IFN-γ in serum ↓ IL-2, IL-6, IL-10 in thymus ↓ IL-10 and IFN-γ in the spleen |
Wistar rat | 1, 5, 30 mg/kg b.w. 36 days |
[72] |
| ↓ CD3+, CD4+, CD8+, CD56+ cells | BALB/c mice | 40 mg/kg b.w. 48h |
[71] |
| ↓ CD4+, CD8+ cells in peripheral blood |
BPC and SPC Sheep | 3.07– 14.49 μg/kg feed winter time |
[106] |
| ZEA 40 µM: Inhibit T cell-chemotaxis by CCL19 ↑ CD4+ T cells induced by CCL19 chemotaxis ZEA 20 µM: ↑ CD8+ T cells induced by CCL21 chemotaxis ↓ expression of chemokine receptor CCR7 and CCR2 |
BALB/cmouse splenic lymphocytes |
10, 20, 40 µM 48h |
[107] |
| ↓ CD3+CD4+ T cells ↑ CD3+CD8+ T cells |
Female Kunming Mice | 20, 30 mg/kg b.w. 12 days |
[108] |
| ↓ CD21+B, CD2+T, CD4+CD8−T ↑ CD8+CD4− and TCRγδ+ T |
Polish Large White female | 0.1 mg/kg 42 days |
[109] |
| ↓ CD4+CD8+, CD4+, CD4+/CD8+(2 mg/kg) ↑ CD8+ (3.2 mg/kg) |
Landrace × Yorkshire × Duroc Piglets |
1.1, 2, 3.2 mg/kg feed 18 days |
[76] |
| ↑ IL-1β and IL-6, ↓ IFN-γ cytoplasmic edema chromatin deformation splenic damages |
Yorkshire × Landrace × Duroc Piglets |
1.1, 2.0, 3.2 mg/kg feed 18 days |
[110] |
| ↓ IFN-γ, IL-10↓ proliferation |
kidneys of piglets | 0.8 mg/kg 4 weeks |
[111] |
| ↑ IL-2, ↓ IL-6 | Isa Brown chicken splenic lymphocytes |
0.1–25 μg/mL 48 h |
[82] |
5. Effect of Zearalenone on Immune Organs
| Effect (s) | Species/Cell Type | Dose/Time of ZEA Administration |
References |
|---|---|---|---|
| Thymic atrophy with histological and thymocyte phenotype changes and decrease in the B cell percentage in the spleen |
Wistar rats | 3.0 mg/kg b.w. 28 days |
[57] |
| Atrophy of white pulp and swelling of red pulp | post-weanling gilts | 2.0, 3.2 mg/kg feed 18 days |
[110] |
| No effect on spleen and bursa of Fabricius weights | one-day-old broiler chicks | 10–800 mg/kg feed 21 days |
[113] |
| No effect on spleen and bursa of Fabricius weights | one-day -old broiler chicks | 50–800 mg/kg feed 3 weeks |
[114] |
| Enlargement of the spleen in males | Sprague Dawley rats | 1.25, 3.75 mg/kg b.w. 8 weeks |
[115] |
| No effect on spleen weight | Sprague Dawley rats | 0.5, 0.9, 1.8, 3.6 mg/kg b.w. 4 weeks |
[116] |
| No effect on spleen weight | BALB/c mice female, 7-weeks-old |
5, 20 mg/kg b.w. 14 days |
[38] |
| No effect on spleen weight | White Leghorn female chickens, 2-weeks-old |
50, 200, 400, 800 mg/kg b.w. 7 days |
[117] |
| No macroscopic changes and no histopathologic effect on lymph nodes | 32-day-old gilts | 0.75 mg/kg feed 21 days |
[81] |
| No effect on thymus and spleen weights No histopathologic changes |
B6C3F1 weanling female mice | 10 mg/kg feed 56 days |
[77] |
| Decreased immune organ weight and lymphocyte counts, lymphoid atrophy and depletion in the spleen | BALB/c female mice |
40, 80 mg ZEN/kg b.w. 28 days |
[118] |
This entry is adapted from the peer-reviewed paper 10.3390/toxins13040248
