Lactiplantibacillus plantarum (Basonym Lactobacillus plantarum) is a good candidate for developing oral vaccines because it survives gastrointestinal conditions transiently colonizing the intestinal tract, it beneficially modulates the mucosal immune responses not only locally (intestinal mucosa) but in distant mucosal sites as well (respiratory mucosa) and there are molecular techniques available for the manipulation of its genome.
- Lactiplantibacillus plantarum
- COVID-19
- SARS-CoV-2
- vaccine
- immunobiotics
- recombinant lactobacilli
- mucosal immunity
- antiviral immunity
1. Introduction
Coronaviruses are positive-sense single-stranded RNA (ssRNA) viruses with a wide range of hosts. To date, seven human coronaviruses (HCoV) were identified as human-pathogens; HCoV-229E, HCoV-OC43, HCoV-NL63 and HCoV-HKU1 (responsible for non-sever common cold), the Severe Acute Respiratory Syndrome coronavirus (SARS-CoV) isolated in 2003 in China and the Middle East Respiratory Syndrome coronavirus (MERS-CoV) that emerged in Middle Eastern countries in 2012 [1]. Both SARS-CoV and MERS-CoV are highly pathogenic viruses that caused nosocomial outbreaks with high case-fatality rates. The seventh and most recently identified human coronavirus is the SARS-CoV-2, responsible for the coronavirus disease 2019 (COVID-19).
COVID-19 emerged in December 2019 in Wuhan, China, and rapidly spread worldwide in a few months due to its high transmissibility and pathogenicity. Although SARS-CoV-2 induce a milder clinical commitment than SARS-CoV or and MERS-CoV, COVID-19 has affected more than 100 million people worldwide, causing the death of 2,217,005 persons according to the WHO’s situation report on 1 February 2021 (WHO, 2021) [2].
Several transmission-mitigation strategies have been implemented in most countries, including social distancing and lockdowns. In addition, a vaccine development race started as never seen before. Currently, several COVID-19 vaccines have finished the phase III clinical testing or been granted an emergency use authorization, including BBIBP-CorV (Sinopharm) and CoronaVac (Sinovac) in China, Pfizer-BioNTech COVID-19 vaccine (Pfizer) and mRNA-1273 vaccine (Moderna) in the United States, and Sputnik-V vaccine in Russia, offering hope for controlling the SARS-CoV-2 infection and stop the pandemic in the near future [3,4,5].
Since the protective immune responses against SARS-CoV-2 are poorly understood, it is unclear which vaccine strategies will be the most successful. The majority of COVID-19 vaccines have been designed to induce anti-SARS-CoV-2 neutralizing antibodies to prevent virus entry into the target cells. In some cases, vaccines are designed to induce both humoral and cellular immunity that could help limiting viral replication in the infected host [5]. Of note, most of the vaccines are designed for parenteral use, and therefore, are capable of mainly inducing systemic immunity despite of the fact that SARS-CoV-2 infects mucosal tissues and that human-to-human transmission is mediated by respiratory droplets and the fecal-oral transmission has not been ruled out [6,7]. The need to generate not only humoral but also cellular immunity against SARS-CoV-2 and to induce protective immunity in the mucosal surfaces where this virus initiates its replication allows us to speculate that this first generation of COVID-19 vaccines should be replaced later by a new generation of vaccines that allow overcoming the aforementioned limitations.
Protective mucosal immune responses are most effectively induced by mucosal immunization through oral or nasal routes, whereas injected vaccines are generally poor inducers of mucosal immunity. However, the induction of mucosal immune responses is challenging due to the physical-chemical barriers of the mucosal surfaces and the tendency to induce tolerance [8]. Therefore, mucosal vaccine delivery systems require high doses of antigens and efficient mucosal adjuvants. Lactic acid bacteria (LAB) have been proposed as both delivery vectors and mucosal adjuvants [9,10]. In the last decades, recombinant LAB have been tested as new-generation oral vaccine vectors due to their natural resistance to gastrointestinal conditions and their ability to modulate both intestinal innate and adaptive immune responses. In this sense, Lactiplantibacillus plantarum (Basonym Lactobacillus plantarum) is a good candidate for developing oral vaccines because it survives gastrointestinal conditions transiently colonizing the intestinal tract, it beneficially modulates the mucosal immune responses not only locally (intestinal mucosa) but in distant mucosal sites as well (respiratory mucosa) and there are molecular techniques available for the manipulation of its genome.
2. L. plantarum as Modulators of Antiviral Immune Responses in Mucosal Tissues
The intestinal microbiota plays a key role in maintaining mucosal antiviral immunity in both local mucosal tissues (intestinal mucosa) and in distal mucosal sites (respiratory mucosa) [80,81,82,83]. Of note, most scientific works highlighted the ability of the intestinal microbiota to modulate the innate antiviral defense mechanisms of the gut and the respiratory tract immune by interacting with epithelial and antigen presenting cells. Furthermore, this modulation of the mucosal innate immune response also influences the mucosal antiviral cellular and humoral adaptive immune responses [82,84,85]. Remarkably, not all the members of the intestinal microbiota contribute equally to the beneficial modulation of the mucosal antiviral immunity. This opened the possibility of exploring particular strains of beneficial bacteria with immunomodulatory capacities, referred to as immunobiotics, in order to increase antiviral defenses in mucosal tissues [82,84,85]. Among these beneficial microorganisms with immunomodulatory capabilities, some L. plantarum strains are interesting alternatives to improve local and distal antiviral immune responses when orally administered [86,87,88].
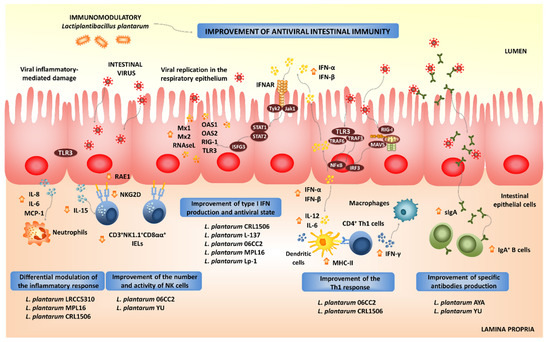
2.1. Modulation of Intestinal Antiviral Immune Responses by L. plantarum
2.2. Modulation of Respiratory Antiviral Immune Responses by L. plantarum
Experiments in animal models and human clinical trials have demonstrated that certain LAB strains, when orally administered, are effective in modulating the respiratory immunity and enhancing the resistance against bacterial and viral infections. This group of immunobiotic LAB improve the resistance of children, adults and the elderly to respiratory infections such as the pneumococcal pneumonia-, the common cold- and influenza-like symptoms [85]. Among the LAB strains that possess this unique immunomodulatory property, there is a group of strains belonging to the species L. plantarum (Figure 4).
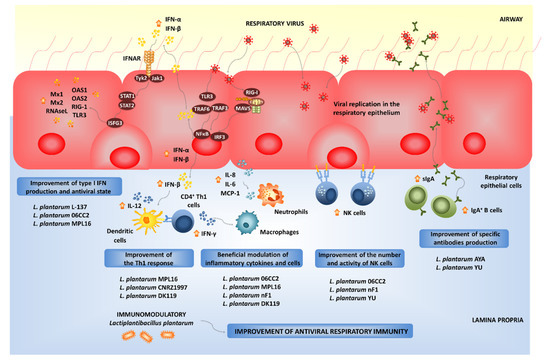
Not all lactobacilli strains possessing immunomodulatory abilities in the intestinal mucosa are capable of stimulating the respiratory immunity when orally administered [110,111,112,113,114,115,116]. Orally administered L. plantarum MPL16 but not L. plantarum CRL1506 was capable of modulating respiratory immunity. The MPL16 strain is capable of improving the levels of IFN-γ and type I IFNs in the respiratory tract, indicating its ability to modulate the function of CD4+IFN-γ+ T cells and CD11c+SiglecF+ alveolar macrophages. Moreover, the increased levels of respiratory IFN-γ and IFN-β found in L. plantarum MPL16-treated mice correlated with the improved resistance of mice to RSV infection [87].
The strain-dependent ability of orally administered LAB to modulate the respiratory immunity was also confirmed by other research groups. The capacity of several L. plantarum strains to modulate the respiratory immunity when orally administered was evaluated in a lethal model of IFV pneumonia [110]. Among the strains evaluated, L. plantarum 06CC2 stood out for its ability to improve the survival of mice infected with IFV, while the L. plantarum strains 05AM23, 06TCa8, 06TCa40 and 06CC9 induced no protective effect. Orally administered 06CC2 strain reduced IFV titers in lungs and improved Th1 response in the respiratory tract and NK cell activity in both lungs and spleens. In addition, in a large-scale screening of immunomodulatory LAB, several Lactiplantibacillus strains were evaluated in their ability to modulate immunity in both TNF-α-activated HT-29 cells and peripheral blood mononuclear cells [116]. Among the evaluated strains, L. plantarum CNRZ1997 was able to significantly increase the production of inflammatory cytokines in both epithelial and immune cells, while other L. plantarum strains showed no effect or demonstrated to have an anti-inflammatory capacity. Interestingly, the work demonstrated that the orally administered CNRZ1997 strain was capable of reducing the replication of IFV in the respiratory tract of mice. The oral treatment with L. plantarum CNRZ1997 was as effective as the oral treatments with L. rhamnosus GG or L. casei DN114-001 (two commercial probiotic strains with anti-IFV properties in preclinical and human trials) to protect mice against IFV infection [84].
It seems that viability is not a requisite for the beneficial modulation of the antiviral respiratory immunity, as was seen with heat-killed L. plantarum L-137, which improved Th1 immunity in healthy subjects [117]. The strain was capable of increasing concanavalin A-induced proliferation of blood lymphocytes and enhancing the percentages of CD4+IFN-γ+ T cells. Orally administered heat-killed L. plantarum L-137 beneficially modulated antiviral immunity in mice [118] and pigs [119], and stimulated the production of IFN-β in mice following IFV infection [118]. Further studies in pigs demonstrated that the L-137 strain significantly improved the expression of IFN-β in blood cells [119]. The treatment with L. plantarum L-137 was translated into a higher body weight gain of pigs when compared to controls, indicating an improved health status. The impact of the L-137 strain on upper respiratory tract infections was evaluated in human subjects with high psychological stress levels [120]. L. plantarum L-137 reduced the incidence, duration and severity of respiratory infections as well as the duration of medication. Similarly, the consumption of L. plantarum nF1-fortified yogurt improved IL-12 and IFN-γ production and NK cell activity in elderly subjects, indicating its potential to stimulate antiviral immunity [121]. In fact, the oral treatment of mice with heat-treated L. plantarum nF1 significantly increased the expression of IFN-γ, IL-2 and IL-12 in the spleen, the NK cell membrane marker Klrb1 and the NK and T cells activation marker CD69 after the challenge with IFV [122]. In line with these findings, a higher splenic NK activity was observed in nF1-treated mice. Those immunological changes induced by L. plantarum nF1 correlated with a reduction of IFV titers and an improved survival of mice [122,123].
Alveolar macrophages are key cells in the beneficial modulation of respiratory immunity induced by gut microorganisms. It was shown that the intestinal microbiota help to maintain the optimal antiviral functions of alveolar macrophages. Beneficial gut microbes are involved in the efficient capacity of alveolar macrophages to produce type I IFNs and antiviral factors including IRF7, IFNGR1, STAT1, STAT2, IFIT3, MX1 and OAS1 that improve the resistance to respiratory viral infections [81]. We have recently demonstrated that immunobiotics with the ability of modulating the respiratory immunity are able to functionally modulate the alveolar macrophages response to viral challenges. In fact, our results indicate that alveolar macrophages greatly contribute to the augment of IFN-γ and IFN-β in the respiratory tract of mice orally treated with L. rhamnosus CRL1505 [115] or L. plantarum MPL16 (submitted for publication). Moreover, an improved expression of IFNAR1, Mx2, OAS1, OAS2, RNAseL and IFITM3 in alveolar macrophages after the oral treatment with L. rhamnosus CRL1505 or L. plantarum MPL16 was detected in our experiments. In line with our results, it was reported that mice orally treated with L. plantarum DK119 had higher BAL IL-2 and IFN-γ levels, and a low degree of inflammation upon IFV infection [124]. The lactobacilli treatment reduced viral loads in the lungs and improved survival of infected mice. In contrast, the levels of IL-6 and TNF-α in the respiratory tract of DK119-treated mice were lower compared to those from control mice after IFV infection. Consistent with this pattern of cytokines, a significantly reduced degree of inflammation was observed in mice receiving L. plantarum DK119. In mice treated with clodronate liposomes to induce the depletion of CD3-CD11b-CD11c+F4/80+ alveolar macrophages, the administration of the DK119 strain could not induce modifications in the severe weight loss and mortality induced by IFV infection, indicating that alveolar macrophages have a key role in L. plantarum DK119-mediated protection [124].
The exact nature of the cellular and molecular signals used by orally administered immunobiotics to modulate the respiratory antiviral immunity remain to be determined. Our recent experiments blocking CD4+ T cells and IFN-γ allow the speculation of a potential mechanism that could explain the remote effect induced by orally administered immunobiotics [115]. The existence of the so-called common mucosal immune system implies that the immune cells activated in one mucosal tissue can mobilize and reach distant mucosal sites, where they can influence immune responses. Then, the mobilization of B and T cells from the intestinal mucosa to the respiratory tract could be involved in the beneficial effects exerted by orally administered immunobiotics [85,115]. Strains such as L. plantarum MPL16 would induce the mobilization CD4+IFN-γ+ T cells from the intestine to the lungs, and the local production of IFN-γ would modulate the respiratory tract innate immune microenvironment, leading to the activation of local immune cells such as alveolar macrophages. As mentioned in the previous section, L. plantarum 06CC2 enhances the expression of IFN-γ and IL-12 in Peyer’s patches, as well as in the respiratory tract supporting the hypothesis that the 06CC2 strain elicited its protective effect in the respiratory tract through intestinal immunity [110]. On the other hand, L. plantarum YU was shown to strongly induce the in vitro production of IL-12 by antigen presenting cells from murine Peyer’s patches, mesenteric lymph nodes and spleen [125], which was associated to TLR2 stimulation. Orally administered L. plantarum YU was able to reduce body weight loss and lung viral replication after a challenge with IFV, to enhance intestinal IgA concentration and splenic NK cell activity. Of note, the levels of IFV-specific secretory IgA in BAL samples were also increased by the oral treatment with L. plantarum YU [125]. Several LAB strains were evaluated according to their ability to stimulate the production of IgA in primary cultures of immune cells isolated from mice Peyer’s patches [126]. Among the strains evaluated, L. plantarum AYA and N63 had the ability to significantly increase IgA levels in vitro. However, when the two strains were evaluated in vivo, only L. plantarum AYA increased the levels of intestinal IgA in orally treated mice. Of note, the immunomodulatory effect was obtained with both the viable bacterium as well as the heat-killed L. plantarum AYA. The oral administration of the AYA strain stimulated DCs by modulating their expression of IL-6 and significantly increased the numbers of IgA+B220+ cells in mice Peyer´s patches. Mice treated with AYA strain and then challenged with IFV had an improved resistance to the viral infection. This protective effect was associated to the induction of higher levels of IgA in the respiratory tract [126]. The work suggested that L. plantarum AYA stimulate IL-6 production in intestinal DCs, which in turn promotes the differentiation of IgA+ B cells into plasma cells improving intestinal IgA production (Figure 3). Moreover, L. plantarum AYA would also induce the mobilization of IgA+ B cells from the intestinal mucosa to the respiratory tract, enhancing the IgA production in the context of a viral respiratory infection (Figure 4).
All in all, these data indicate that appropriate immunobiotic L. plantarum strains could be used to improve antiviral immunity on both the intestinal and the respiratory mucosa at the same time, and therefore, they are an interesting biotechnological resource for the development of mucosal vaccines.
This entry is adapted from the peer-reviewed paper 10.3390/microorganisms9040683
