The phenomenon of pain sensation is defined differently, depending on the specialty. From the point of view of psychology or psychiatry, pain is a difficult to define and a subjective experience. Being a result of awareness of nerve impulses reaching the brain and caused by noxious stimuli of adequate strength, pain can be also defined as a psychic factor, triggering defensive reflexes. From a biological point of view, pain is a warning signal about a danger or tissue injury. Pain is a sensory impression, formed by the action of various stimuli that damage tissues; therefore, pain provides information about the action site of the harmful factor (stressor). Pain can be experienced as a local sensation or as widespread pain when the response to stimulus is intense and the effect of the damage lasts for an extended duration. Controversies still exist regarding nomenclature and definitions specifying the phenomenon of pain. According to the Taxonomy Committee of the International Association for the Study of Pain (IASP), pain is defined as an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.
- pain
- pathomechanisms
- nonspecific therapy
- sheep
1. Introduction
Since the earliest times, living organisms receive stimuli from their environment. Many of these stimuli are beneficial; however, some stimuli cause discomfort to individuals. These adverse stimuli usually cause discomfort of a painful (nociceptive), even damaging (noxa), and sometimes toxic nature. Organisms have to avoid or counter situations when the body’s homeostasis is disturbed by these adverse factors or painful stimuli [1], regardless of the nature of the stimulus (physical, chemical, or psychological) [2]. Homeostasis is restored in humans by neuroendocrine reactions or, when these are not sufficient, e.g., when the nociceptive factor exceeds the adaptability of organisms, by using substances that restore a sense of comfort. The same procedure applies to all vertebrate animals that react similarly to humans.
2. Historical Outline
Pain has been known since the dawn of time, for as long as living organisms have existed. Considered as a complex physiological phenomenon, pain provides evidence of the effective impact of the external and internal environment on organisms. Pain is regarded as a special type of experience that results in various affective reactions with strong emotional components. As far back as 1550 BCE, opium was used to relieve pain and was described on Ebers papyrus. Hippocrates (460–377 BC), named by posterity the father of medicine, claimed that pain is one of the actual symptoms of disease. According to him, the brain was the main location of pain sensation; therefore, it is not surprising that, for many centuries, pain was considered to be a symptom of disease of the soul and heart. Galen (130–201) and Avicenna (980–1037) were pioneers in identifying the location and causes of pain formation, claiming that the phenomenon of pain develops in the brain and nerves because of sudden shifts in the distribution of body fluids and changes in tissue continuity. Leonardo da Vinci (1442–1519) presented a still valid hypothesis that pain was associated with touch sensation, being a consequence of an excessive stimulus action, currently termed a noxious stimulus. Descartes (1569–1650) presented in his work “Tractatus de homine”, a description of a hypothetical path through which impulses pass from the site of action to a center in the brain. It was not until the 20th century that a breakthrough in research occurred concerning on pain perception. The results of experimental studies carried out in the last two decades have provided biological evidence for progress in the recognition of both the morphological and the functional basis of the phenomenon of pain perception. However, controversies and inconsistencies of this fascinating phenomenon are still evident. In particular, in recent years, other endogenous opioids, termed endogenous morphines (endomorphin-1, endomorphin-2), were discovered [3,4,5] and the presence and structure of a presumed endogenous pain transmitter (nociceptin) was reported, but the transmitter’s biological role in living organisms is still being elucidated [6,7].
Since the time of Sertürner, who, in 1804, isolated the substance he named after the god of sleep, Morpheus, it is known that the compound that reduces or abolishes the adverse effects of pain stimuli is morphine, a phenanthrene opium alkaloid from Papaver somniferum with analgesic and narcotic effects (addictive and tolerance-inducing). Fifty years after its isolation, morphine was added to the arsenal of drugs used in the treatment of postoperative and chronic pain [8].
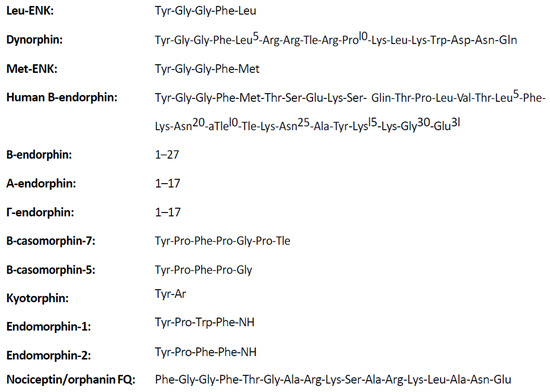
Alleviation of endogenous pain by an exogenous alkaloid brought up an assumption that a morphine-specific locus of action must exist in living organisms. Over time, the presence of receptors for morphine, later named opioid receptors, was validated, and other receptors were subsequently identified, named, and localized. The existence of three basic groups of opioid receptors (µ, δ, and κ) was determined, and the division into subtypes of these groups (µ1, µ2, δ1, δ2, κ1, κ2, and κ3) was suggested by some authors (Table 1). These receptors are distributed over the central and peripheral nervous system and organs (Table 2) and are present at the highest density in the structures responsible for reception and conductivity of pain stimuli in humans and other vertebrates [3,4,7]. Furthermore, the presence of various opioid receptors in the organism’s structures suggested the existence of endogenous substances specific for these receptors. The existence of compounds with morphine-like activity was, thus, proven and named endogenous morphine (endorphins), which are peptides with opioid activity (endogenous opioid peptides; EOPs) (Figure 1). To distinguish endorphins from opioid-like substances of exogenous origin, exogenous substances were named opiates. Subsequently, numerous endorphins were identified in the body (Figure 1) [4,6].
| Receptor | Subtypes | Location | Function | G Protein Subunit |
|---|---|---|---|---|
| delta (δ) DOR OP1 (I) |
δ1, δ2 |
|
|
Gi |
| kappa (κ) KOR OP2 (I) |
κ1, κ2, κ3 |
|
|
Gi |
| mu (μ) MOR OP3 (I) |
μ1, μ2, μ3 |
|
μ1:
|
Gi |
| Nociceptin receptor NOR OP4 (I) |
ORL1 |
|
|
|
| zeta (ζ) ZOR |
|
|
| Receptor Subtype | µ | δ | κ | |
|---|---|---|---|---|
| Effect | ||||
| Analgesia | ||||
| Supraspinal | +++ | − | − | |
| Spinal | ++ | ++ | + | |
| Peripheral | ++ | − | ++ | |
| Inhibition of respiration | +++ | ++ | − | |
| Miosis | ++ | − | + | |
| Inhibition of gastrointestinal motility | ++ | ++ | + | |
| Euphoria | +++ | − | − | |
| Dysphoria | − | − | +++ | |
In the wake of the achievements of theoretical sciences, exogenous substances that mimic the effects of endogenous endorphins were soon developed. Some of the obtained opiate substances proved to be 1000–80,000 times more potent in analgesic tests than their protoplast, morphine [1,10]. However, these substances have certain adverse effects in some species, particularly ruminants [1,11]. Effects are excitant and sympathomimetic, and, in humans, there is stimulation of the reward system (addiction) and inducement of tolerance to these drugs. Differences are due to the fact that companion animals have well-developed analgesic and preanesthetic processes [8,11] and farm animals suffer from a constant deficiency of these processes [12,13].
Non-narcotic analgesics for suitability for use in ruminant anesthesiology (α2-adrenergic receptor agonists, nonsteroidal anti-inflammatory drugs (NSAIDs) [8], local anesthetics, ionotropic glutaminergic receptor antagonists (iGluRAs) such as ketamine, and voltage-gated calcium channel inhibitors (VGCCIs; diltiazem, nifedipine, verapamil, type 1 cholecsystokinin receptor antagonists—CCK1)) have been the subject of recent research interests. Sheep, for example, have many behavioral and biochemical reactions that are similar to human reactions [13]. This was a main reason for undertaking this study to investigate a new method for determining visceral pain during the viscero-visceral inhibitory reflex test in use since the 1990s [14].
3. Types of Pain
According to nociceptive stimuli action areas, the following types of pain are distinguished: (1) superficial (skin) pain, (2) deep pain resulting from damage of the musculoskeletal system, and (3) visceral pain, a consequence of ongoing disease processes in internal organs [19]. The first two types are called physiological pain. Superficial pain is experienced because of the action of nociceptive stimuli on the pain receptors in the skin (nociceptors), whereas deep pain can cause bone injury, damage, or straining of the articular capsule or tendon. For each type of pain, as mentioned above, the sensations may be local or diffuse pain. Pain can also be divided into physiological and pathological types. Pathological pain includes postoperative, chronic, inflammatory, and cancer pains, as well as pain associated with muscle ischemia (ischemic pain), rheumatoid pain (related to musculoskeletal disorders), and neuropathic pain that occurs in nerve diseases, whereas physiological pain is derived from nondisease stimuli [20,21].
This entry is adapted from the peer-reviewed paper 10.3390/ani11030909
