Cancer related fatigue is a common and distressing symptom for patients with cancer during and after primary treatment, and also in the palliative phase of the disease trajectory.
- fatigue
- palliative care
- cancer
- cancer related fatigue
1. Introduction
Fatigue is one of the most distressing symptoms experienced by patients with cancer and has a high prevalence in cancer patients [1]. Fatigue can occur before, during and after treatment and persist for a long time [2][3]. Different definitions have been used, but today the most widely used definition stems from the National Comprehensive Cancer Network, NCCN, “Cancer-Related Fatigue is a distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to recent activity and interferes with usual functioning” [4].
The concept of fatigue as a multidimensional symptom has been challenged by the notion that fatigue rather should be regarded as a set of multiple symptoms to be addressed separately [5][6]. The trajectory of fatigue may also change in accordance with development of the cancer disease, with physical but not mental fatigue reported to be more severe in advanced stage cancer patients compared to cancer survivors or healthy individuals [7][8][9]. Cancer related fatigue (CRF) could have a negative impact on patients physical, psychological, social and existential wellbeing, with an impaired experience of quality of life (QoL) as a result [3]. Most research regarding treatment strategies to reduce CRF has been performed in younger patients, with a bias towards women with breast cancer during or after primary treatment [10].
Various measurements are being used to assess presence, frequency and severity of symptoms in palliative care [7][11][12]. The presence of fatigue in patients with cancer with palliative needs is of risk of being overseen by health care personnel due to difficulties in identifying the symptom but also due to a lack of enhanced knowledge of mechanisms causing fatigue. There is a risk that patients suffering from fatigue underreport the symptom if assessment is not made or if health care personnel do not acknowledge the symptom and bring it up for discussion [13]. Patient reported outcome might differ from physician reported outcome [14], suggesting the importance of using validated assessment tools when measuring fatigue.
Cancer Related Fatigue in Patients in Palliative Care
The World Health Organization (WHO) stresses the importance of alleviating distressing symptoms to improve QoL in patients suffering from a life shortening disease [15]. Early identification and symptom management has a key role in palliative care regarding the patients’ physical, psychosocial and existential needs. The improvement of treatments of non-curable diseases can facilitate a prolonged lifetime for patients with life shortening diseases, hence the importance of an active palliative care to improve QoL [16]. The recently proposed revision of the definition of palliative care emphasizes the need for evidence-based practice [17].
Continuous improvement of oncological treatment strategies has steadily improved survival times for patients with cancer in the palliative phase. During these longer disease trajectories, fatigue is a clinical problem for many individuals. Aggregated data from studies on cancer patients with fatigue as a primary outcome show that physical activity and psychological interventions are the best method to alleviate symptoms [10]. However, increased physical activity may not always be an option in the palliative phase, and pharmacological methods must therefore be considered. Neither have psychological interventions been shown to relieve fatigue in patients with advanced stage cancer during and after primary treatment [18], in contrast to patients earlier in their disease trajectory [10]. There is a lack of studies on both physical activity and psychological interventions on patients in the late palliative phase of the cancer disease.
In a previous study on fatigue in patients admitted to palliative care (n = 228) it was shown that fatigue increased closer to death [8]. However, fatigue was more distressing and associated with impaired QoL in patients with 2–6 months left in life while the association between fatigue and QoL disappeared during the last days and weeks of life [8].
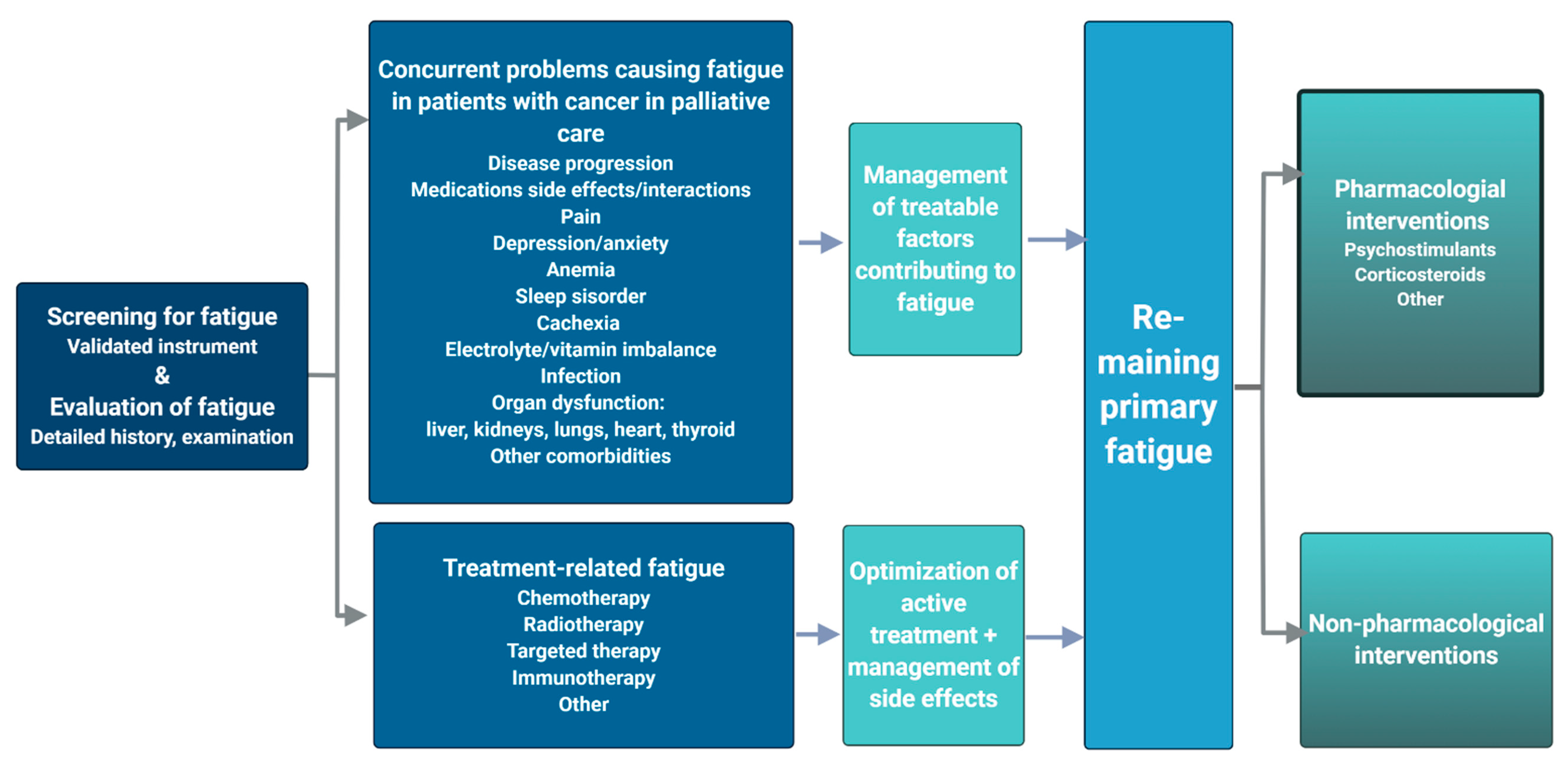
2. Etiology of Cancer Related Fatigue
Fatigue in cancer patients in the palliative phase may be due to both preventable and treatable concurrent conditions, e.g., depression, infections, anemia, sleep disorders, pain, vitamin imbalance, etc. (Figure 1). These should be identified through a detailed medical history, physical examination and relevant investigations [4] and treated according to guidelines/best practice with regard to patients’ wishes and functional status [19]. Additionally, side effects of active oncological treatment include fatigue, and it is important to screen patients in a palliative phase of their disease trajectory for self-assessed fatigue to optimize systemic oncological treatment. Further, fatigue is as such a self-assessed, subjective measure subject to variations in social, emotional and existential status [3][20].
The mechanistic, pathophysiologic underpinning for cancer related fatigue that remains when other factors have been treated/excluded, so called “primary fatigue” according to European Association of Palliative Care (EAPC) 2008 [2], is elusive, but several underlying mechanisms have been proposed in recent reviews [3][22][23]: peripheral immune activation and inflammatory dysfunction due to both to immune system response to tumor tissue and triggered by anticancer treatment; skeletal muscle and mitochondrial dysfunction (in conjunction with cancer cachexia) and neuronal disorders. This adheres well to the categorization of causative concepts by Bower et al. in 2014 in two categories—inflammation and neuroendocrine alterations.
The etiology of fatigue may differ in the early palliative phase compared to the late phase. In the early phase, fatigue and change in fatigue often show an association with inflammation biomarkers [24]. However, in the late stage, close to death, an improvement in fatigue is often difficult to achieve and recovery of inflammatory biomarkers is seldom possible. The experience of fatigue in the very last days of life is also influenced by other symptoms, and the fact that life comes to an end. Despite the same influential etiology, the experience and meaning of fatigue can differ in End-of-Life compared to earlier palliative phases [8].
Both the European Society for Medical Oncology, ESMO and the United States National Comprehensive Cancer Network (NCCN), and other national medical organizations publish consensus-based clinical practice guidelines regarding management of cancer related fatigue with recent updates available [4][25][26]. ESMO does not differentiate between patients in different phases of their disease in their guidelines, but considers patients aged 65 or above separately, since little data on both fatigue assessment and best treatment practice is available for this group [25]. NCCN identifies three groups of cancer patients: undergoing active treatment with focus on curative treatment, post treatment patients and patients in End-of-Life, but does not specifically consider patients in an earlier palliative phase [4]. According to NCCN guidelines, both methylphenidate and shorter courses of corticosteroids can be considered in End-of-Life management of CRF. ESMO, on the other hand, could not reach a consensus on the benefits regarding methylphenidate, but advocates shorter courses of corticosteroids in patients with metastatic cancer [25]. No other pharmacological interventions are deemed beneficial in this setting by either ESMO or NCCN.
This entry is adapted from the peer-reviewed paper 10.3390/cancers13050985
References
- Yennurajalingam, S.; Bruera, E. Review of Clinical Trials of Pharmacologic Interventions for Cancer-Related Fatigue. Cancer J. 2014, 20, 319–324.
- Radbruch, L.; Strasser, F.; Elsner, F.; Gonçalves, J.F.; Løge, J.; Kaasa, S.; Nauck, F.; Stone, P. Fatigue in palliative care patients—An EAPC approach. Palliat. Med. 2008, 22, 13–32.
- Bower, J.E. Cancer-related fatigue—Mechanisms, risk factors, and treatments. Nat. Rev. Clin. Oncol. 2014, 11, 597–609.
- National Comprehensive Cancer Network. NCCN Guidelines Version 1.20201 Cancer-Related Fatigue. 2020. Available online: (accessed on 15 December 2020).
- Thong, M.S.Y.; Mols, F.; Van De Poll-Franse, L.V.; Sprangers, M.A.G.; Van Der Rijt, C.C.D.; Barsevick, A.M.; Knoop, H.; Husson, O. Identifying the subtypes of cancer-related fatigue: Results from the population-based PROFILES registry. J. Cancer Surviv. 2017, 12, 38–46.
- De Raaf, P.J.; De Klerk, C.; Van Der Rijt, C.C.D. Elucidating the behavior of physical fatigue and mental fatigue in cancer patients: A review of the literature. Psychooncology 2012, 22, 1919–1929.
- Hagelin, C.L.; Wengström, Y.; Fürst, C.J. Patterns of fatigue related to advanced disease and radiotherapy in patients with cancer—A comparative cross-sectional study of fatigue intensity and characteristics. Support. Care Cancer 2008, 17, 519–526.
- Hagelin, C.L.; Wengstrom, Y.; Ahsberg, E.; Furst, C.J. Fatigue dimensions in patients with advanced cancer in relation to time of survival and quality of life. Palliat. Med. 2009, 23, 171–178.
- De Raaf, P.J.; De Klerk, C.; Timman, R.; Hinz, A.; Van Der Rijt, C.C. Differences in Fatigue Experiences Among Patients with Advanced Cancer, Cancer Survivors, and the General Population. J. Pain Symptom Manag. 2012, 44, 823–830.
- Mustian, K.M.; Alfano, C.M.; Heckler, C.; Kleckner, A.S.; Kleckner, I.R.; Leach, C.R.; Mohr, D.; Palesh, O.G.; Peppone, L.J.; Piper, B.F.; et al. Comparison of Pharmaceutical, Psychological, and Exercise Treatments for Cancer-Related Fatigue. JAMA Oncol. 2017, 3, 961–968.
- Al Maqbali, M.; Hughes, C.; Gracey, J.; Rankin, J.; Dunwoody, L.; Hacker, E. Quality assessment criteria: Psychometric properties of measurement tools for cancer related fatigue. Acta Oncol. 2019, 58, 1286–1297.
- Al Maqbali, M.; Al Sinani, M.; Al Naamani, Z.; Al Badi, K.; Tanash, M.I. Prevalence of Fatigue in Patients with Cancer: A Systematic Review and Meta-Analysis. J. Pain Symptom Manag. 2021, 61, 167–189.
- Mock, V. Fatigue management: Evidence and guidelines for practice. Cancer 2001, 92, 1699–1707.
- Tanioka, H.; Miyamoto, Y.; Tsuji, A.; Asayama, M.; Shiraishi, T.; Yuki, S.; Kotaka, M.; Makiyama, A.; Shimokawa, M.; Shimose, T.; et al. Prophylactic Effect of Dexamethasone on Regorafenib-Related Fatigue and/or Malaise: A Randomized, Placebo-Controlled, Double-Blind Clinical Study in Patients with Unresectable Metastatic Colorectal Cancer (KSCC1402/HGCSG1402). Oncology 2018, 94, 289–296.
- WHO. Definition of Palliative Care. Available online: (accessed on 5 October 2020).
- Verkissen, M.N.; Hjermstad, M.J.; Van Belle, S.; Kaasa, S.; Deliens, L.; Pardon, K. Quality of life and symptom intensity over time in people with cancer receiving palliative care: Results from the international European Palliative Care Cancer Symptom study. PLoS ONE 2019, 14, e0222988.
- Radbruch, L.; De Lima, L.; Knaul, F.; Wenk, R.; Ali, Z.; Bhatnaghar, S.; Blanchard, C.; Bruera, E.; Buitrago, R.; Burla, C.; et al. Redefining Palliative Care—A New Consensus-Based Definition. J. Pain Symptom Manag. 2020, 60, 754–764.
- Poort, H.; Peters, M.; Bleijenberg, G.; Gielissen, M.F.; Goedendorp, M.M.; Jacobsen, P.; Verhagen, S.; Knoop, H. Psychosocial interventions for fatigue during cancer treatment with palliative intent. Cochrane Database Syst. Rev. 2017, 2017.
- Koornstra, R.H.; Peters, M.; Donofrio, S.; Borne, B.V.D.; De Jong, F.A. Management of fatigue in patients with cancer–A practical overview. Cancer Treat. Rev. 2014, 40, 791–799.
- Peters, M.E.; Goedendorp, M.M.; Verhagen, S.A.; Smilde, T.J.; Bleijenberg, G.; Van Der Graaf, W.T.A. A prospective analysis on fatigue and experienced burden in informal caregivers of cancer patients during cancer treatment in the palliative phase. Acta Oncol. 2015, 54, 500–506.
- Bower, J.E.; Bak, K.; Berger, A.; Breitbart, W.; Escalante, C.P.; Ganz, P.A.; Schnipper, H.H.; Lacchetti, C.; Ligibel, J.A.; Lyman, G.H.; et al. Screening, Assessment, and Management of Fatigue in Adult Survivors of Cancer: An American Society of Clinical Oncology Clinical Practice Guideline Adaptation. J. Clin. Oncol. 2014, 32, 1840–1850.
- Yang, S.; Chu, S.; Gao, Y.; Ai, Q.; Liu, Y.; Li, X.; Chen, N. A Narrative Review of Cancer-Related Fatigue (CRF) and Its Possible Pathogenesis. Cells 2019, 8, 738.
- O’Higgins, C.M.; Brady, B.; O’Connor, B.; Walsh, D.; Reilly, R.B. The pathophysiology of cancer-related fatigue: Current controversies. Support. Care Cancer 2018, 26, 3353–3364.
- Paulsen, Ø.; Laird, B.; Aass, N.; Lea, T.; Fayers, P.; Kaasa, S.; Klepstad, P. The relationship between pro-inflammatory cytokines and pain, appetite and fatigue in patients with advanced cancer. PLoS ONE 2017, 12, e0177620.
- Fabi, A.; Bhargava, R.; Fatigoni, S.; Guglielmo, M.; Horneber, M.; Roila, F.; Weis, J.; Jordan, K.; Ripamonti, C. Cancer-related fatigue: ESMO Clinical Practice Guidelines for diagnosis and treatment. Ann. Oncol. 2020, 31, 713–723.
- Vilchynska, T.; Beard, B. Cancer-related fatigue in palliative care: A global perspective. Int. J. Palliat. Nurs. 2016, 22, 244–252.