The metabolism of tryptophan is intimately associated with the differential regulation of diverse physiological processes, including in the regulation of responses to severe acute respiratory syndrome, coronavirus-2 (SARS-CoV-2) infection that underpins the COVID-19 pandemic.
- tryptophan
- severe acute respiratory syndrome
1. Introduction
There is a growing appreciation that tryptophan and its metabolites are crucial aspects of the severe acute respiratory syndrome, coronavirus-2 (SARS-CoV-2) pathophysiology that has driven the COVID-19 pandemic. SARS-CoV-2 severity and fatality are strongly driven by advanced age as well as pre-existing co-morbidities, such as obesity and type 2 diabetes (T2D), as well as by stress-associated conditions, including racial discrimination stress [1]. It is widely accepted that it is alterations in the immune response that drive an individual’s susceptibility to severe SARS-CoV-2 infection. This is supported by the World Health Organization (WHO), which recently admitted that their recommended treatments, viz Remdesivir, Lopinavir, β-interferon (IFN), and Hydroxychloroquine proved of little utility, whilst treatments more directly targeting the immune response, such as Dexamethasone, were more beneficial [2].
Tryptophan and its metabolites, including kynurenine and indole-3-pyruvate (I3P), can be differentially regulated over the course of SARS-CoV-2 infection, which is strongly determined by the influence of pre-existing high-risk conditions, such as obesity/T2D and ageing, on the immune response [1]. The influence of the tryptophan metabolites, kynurenine and 13P, are mediated via the activation of the aryl hydrocarbon receptor (AhR). The AhR can have a number of complex effects, that may be partly ligand-dependent as well as from the complex interactions of the AhR with metabolic and circadian processes [3].
2. Integrating Tryptophan Metabolism into COVID-19 Pathophysiology
As indicated throughout, variations in the regulation of tryptophan and its metabolites are intimately linked to key processes underpinning SARS-CoV-2 pathophysiology. The raised levels of pro-inflammatory cytokines during the initial ‘cytokine’ storm will drive the upregulation of IDO and its conversion of tryptophan to kynurenine. This has two important consequences, viz increasing AhR activation and decreasing the availability of tryptophan for the serotonergic and melatonergic pathways. As SARS-CoV-2 may increase AhR ligands independently of IDO induction, it is proposed that SARS-CoV-2, like other viral infections, may be associated with the upregulation of IL4I1, and thereby with the driving of tryptophan to the production of other AhR ligands, viz I3P and I3A [4]. See Figure 1.
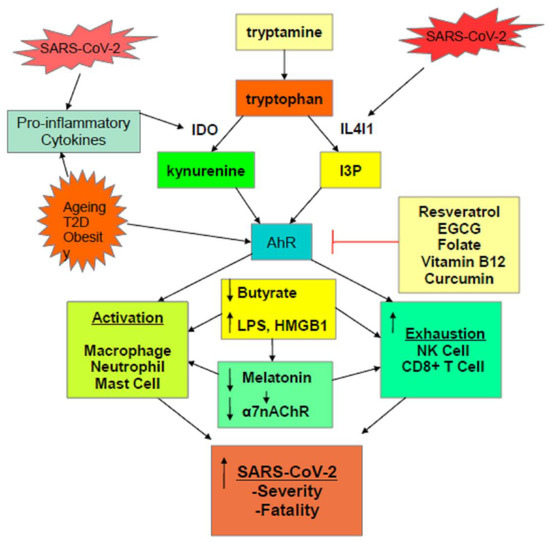
Figure 1. Scheme showing how the SARS-CoV-2 virus, and pre-existent high-risk medical conditions, shift tryptophan metabolism to increase AhR ligands. The activation of the AhR alters the nature of the initial ‘cytokine storm’ and suppresses the endogenous antiviral responses of NK cells and CD8+ T cells, leading to a prolonged activation of macrophages, neutrophils, and mast cells, as evident in severe SARS-CoV-2 infection. The driving to tryptophan to kynurenine and I3P, along with the elevated pro-inflammatory cytokines of the ‘cytokine storm’, also suppresses pineal melatonin production and therefore the induction of the α7nAChR by melatonin, thereby contributing lost vagal dampening of immune activity and raising sympathetic nervous system activation. The elevation in pro-inflammatory cytokines also increases gut dysbiosis/permeability, leading to a decrease in butyrate and raising LPS levels, further contributing to metabolic dysregulation of patterned immune responses to SARS-CoV-2 infection. A number of readily available nutraceuticals, such as resveratrol, EGCG, folate, vitamin B12, and curcumin, by AhR inhibition, may act to modulate how many processes influence SARS-CoV-2 pathophysiology.
Increased AhR activation will dysregulate the immune response, contributing to a heightened pro-inflammatory phase during the initial ‘cytokine storm’, whilst also suppressing the endogenous antiviral cell responses of NK cells and CD8+ T cells. Consequently, there is prolongation of heightened pro-inflammatory activity in the initial phase of infection, at least in part driven by the suppressed antiviral responses of NK cells and CD8+ T cells, which would typically control the immune response around 7 days after initial infection. It has been recognized that this dysregulated immune response is the major driver of SARS-CoV-2 severity and fatality.
SARS-CoV-2 severity risk factors, including elderly age, obesity, and T2D, prime for an altered immune response by a number of mechanisms. These conditions are all associated with an increase in AhR levels and activity as well as an increase in pro-inflammatory cytokines/IDO/kynurenine, leading to AhR activation. Diet is known to regulate IL4I1 [5], suggesting that dietary factors contributing to obesity and T2D may be acting in part via the upregulation of IL4I1 and I3P.
As well as regulating the immune response, AhR activation primes platelets for activation, coagulation, and thrombin formation, as does TLR4 activation that may arise from gut permeability-derived LPS and HMGB1. Gut dysbiosis/permeability and AhR activation are therefore important contributors to the association of activated platelets to SARS-CoV-2 fatality. The gut is intimately associated with the regulation of tryptophan and its metabolites. Many of the beneficial effects of butyrate are mediated by its upregulation of the melatonergic pathway, highlighting that the driving of tryptophan to the production of AhR ligands and away from serotonin, NAS, and melatonin production, will attenuate the beneficial effects of butyrate. This may be of particular relevance in immune cells, where butyrate’s induction of PDC/acetyl-CoA/OXPHOS/TCA cycle/melatonergic pathway are important to a more optimized antiviral immune response by NK cells and CD8+ T cells.
The important role of the circadian rhythm may also be similarly modulated by variations in tryptophan regulation. Recent work would indicate that the importance of pineal melatonin to immune cell ‘resetting’ over the circadian rhythm may be mediated by the activation of the Bmal1/SIRT1/SIRT3/PDC/acetyl-CoA/OXPHOS/TCA cycle/melatonergic pathway [3]. The driving of tryptophan away from serotonin production will attenuate pineal melatonin’s influence on the metabolism of immune cells. Importantly, AhR activation arising from the induction of kynurenine and I3P will increase AhR-induced CYP1B1, thereby backward converting melatonin to NAS, whilst the ability of AhR activation to suppress 14-3-3 [6] can prevent the activation of the AANAT and the melatonergic pathway. 14-3-3 is necessary for the stabilization of AANAT, indicating that AhR suppression of 14-3-3 may inhibit mitochondrial and cytoplasmic melatonin production. As the release and autocrine effects of melatonin are required to switch immune cells from an M1-like pro-inflammatory phenotype to an M2-like, anti-inflammatory, pro-phagocytic phenotype [7], the induction of tryptophan metabolites can significantly alter the nature of the immune response. As such, as well as modulating circadian regulation of the immune system, an increase in tryptophan metabolite-driven AhR activation can change the nature of the activation–deactivation processes in individual immune cells.
There is a growing appreciation of the pathophysiological and treatment relevance of vitamin D in the SARS-CoV-2 infection. By regulating serotonin levels [8], vitamin D will modulate the serotonin-melatonergic pathway, whilst the suppression of pro-inflammatory cytokine production by vitamin D [9] will attenuate cytokine-induced IDO and the pro-inflammatory route for activation of the AhR by kynurenine. As noted, melatonin can bind the vitamin D receptor, thereby potentiating some vitamin D-driven transcription [10]. The suggests that attenuation of the tryptophan/serotonin/melatonin pathway by IDO, TDO, and IL4I1 can suppress vitamin D-driven transcription. As such, the effects of vitamin D in the SARS-CoV-2 infection may be intimately linked to alterations in tryptophan metabolism.
This entry is adapted from the peer-reviewed paper 10.3390/ijms22041597
References
- Anderson, G.; Carbone, A.; Mazzoccoli, G. Aryl Hydrocarbon Receptor Role in Co-Ordinating SARS-CoV-2 Entry and Symptomatology: Linking Cytotoxicity Changes in COVID-19 and Cancers; Modulation by Racial Discrimination Stress. Biology 2020, 9, 249.
- WHO Solidarity Trial Consortium; Pan, H.; Peto, R.; Henao-Restrepo, A.M.; Preziosi, M.P.; Sathiyamoorthy, V.; Abdool Karim, Q.; Alejandria, M.M.; Hernández García, C.; Kieny, M.P.; et al. Repurposed Antiviral Drugs for Covid-19—Interim WHO Solidarity Trial Results. N. Engl. J. Med. 2020.
- Anderson, G. Tumour Microenvironment: Roles of the Aryl Hydrocarbon Receptor, O-GlcNAcylation, Acetyl-CoA and Melatonergic Pathway in Regulating Dynamic Metabolic Interactions across Cell Types—Tumour Microenvironment and Metabolism. Int. J. Mol. Sci. 2020, 22, 141.
- Turski, W.A.; Wnorowski, A.; Turski, G.N.; Turski, C.A.; Turski, L. AhR and IDO1 in pathogenesis of Covid-19 and the “Systemic AhR Activation Syndrome:” a translational review and therapeutic perspectives. Restor. Neurol. Neurosci. 2020, 38, 343–354.
- Arpon, A.; Riezu-Boj, J.I.; Milagro, F.I.; Marti, A.; Razquin, C.; Martinez-Gonzalez, M.A.; Corella, D.; Estruch, R.; Casas, R.; Fito, M.; et al. Adherence to Mediterranean diet is associated with methylation changes in inflammation-related genes in peripheral blood cells. J. Physiol. Biochem. 2016, 73, 445–455.
- Zhao, Y.; Fu, Y.; Sun, Y.; Zou, M.; Peng, X. Transcriptional Regulation of gga-miR-451 by AhR:Arnt in Mycoplasma gallisepticum (HS Strain) Infection. Int. J. Mol. Sci. 2019, 20, 3087.
- Muxel, S.M.; Pires-Lapa, M.A.; Monteiro, A.W.A.; Cecon, E.; Tamura, E.K.; Floeter-Winter, L.M.; Markus, R.P. NF-κB Drives the Synthesis of Melatonin in RAW 264.7 Macrophages by Inducing the Transcription of the Arylalkylamine-N-Acetyltransferase (AA-NAT) Gene. PLoS ONE 2012, 7, e52010.
- Kaneko, I.; Sabir, M.S.; Dussik, C.M.; Whitfield, G.K.; Karrys, A.; Hsieh, J.-C.; Haussler, M.R.; Meyer, M.B.; Pike, J.W.; Jurutka, P.W. 1,25-Dihydroxyvitamin D regulates expression of the tryptophan hydroxylase 2 and leptin genes: Implication for behavioral influences of vitamin D. FASEB J. 2015, 29, 4023–4035.
- Li, H.; Li, W.; Wang, Q. 1,25-dihydroxyvitamin D3 suppresses lipopolysaccharide-induced interleukin-6 production through aryl hydrocarbon receptor/nuclear factor-κB signaling in oral epithelial cells. BMC Oral Health 2019, 19, 236.
- Fang, N.; Hu, C.; Sun, W.; Xu, Y.; Gu, Y.; Wu, L.; Peng, Q.; Reiter, R.J.; Liu, L.-F. Identification of a novel melatonin-binding nuclear receptor: Vitamin D receptor. J. Pineal Res. 2019, 68, 12618.
