The attention to transgender medicine has changed over the last decade and the interest is most likely going to increase in the future due to the fact that gender-affirming treatments are now being requested by an increasing number of transgender people. Even if gender-affirming hormone therapy (GAHT) is based on a multidisciplinary approach, this review is going to focus on the procedures adopted by the endocrinologist in an out-clinic setting once an adult patient is referred by another specialist for ‘gender affirming’ therapy.
- transgender
- healthcare
- hormonal treatment
- follow-up
- endocrinologist
1. Introduction
Over the past 10 years, awareness about transgender medicine has increased. Gender identity refers to “a person’s deeply-felt, inherent sense of being a boy, a man, or a male, a girl, a woman, or a female, or an alternative gender (e.g., genderqueer, gender nonconforming, gender neutral) that may or may not correspond to a person’s gender assigned at birth or to a person’s primary or secondary sex characteristics” [1]. In this narrative review, we shall focus our attention on the endocrine clinical and therapeutic approach of people experiencing Gender Dysphoria (GD) as defined by a distress due to “a marked incongruence between a person’s gender assigned at birth and gender identity” [2].
It has been estimated a GD prevalence rate of 0.005–0.014% for assigned male at birth (AMAB) and 0.002–0.003% for assigned female at birth (AFAB) people [3].
In addition to binary GD, health-care professionals (HCPs) working with transgende people should also recognize individuals who do not identify themselves exclusively as either men or women (i.e., non-binary individuals). Patients asking for a gender-affirming medical approach should be evaluated by HCPs with expertise in mental health to also identify the need of a mental health professional’s intervention [4].
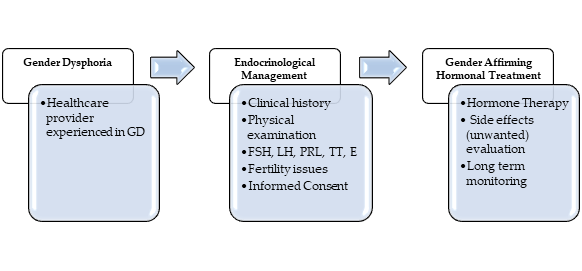
GD should be managed by a multidisciplinary team and diagnosis should be done by an expert physician with specific skills and abilities [5]. Based on fulfillment of diagnostic criteria by prior HCP’s evaluations, we aimed to describe the role of the endocrinologist in the management of the different gender-affirming treatment options and of clinical monitoring in transgender adults in our multidisciplinary single-center medical clinic dedicated to outpatients. In fact, also during the diagnostic workup, the endocrinologist is required to investigate on possible medical contraindications to the Gender Affirming Hormonal Treatment (GAHT). When a specific hormonal treatment for GD is practicable, it can be started without further investigations [6] after informing each patient about efficacy and possible side effects of GAHT and fertility preservation techniques [7]. The distress of living in an incongruent body and gender role is often present since childhood and adolescence, but the treatment of youths with gender incongruence is not a matter of discussion of the present review. Our general diagnostic-therapeutic approach is depicted in Figure 1.
Figure 1. Diagnostic-therapeutic algorithm in Gender Dysphoria (GD). Legends: FSH = Follicle-Stimulating Hormone; LH = Luteinizing Hormone; PRL = Prolactin; TT = total testosterone; E = estradiol.
2. The Endocrinological Management of Transgender Men
In AFAB individuals experiencing GD and asking for full virilization, the main targets of GAHT are to suppress endogenous female hormones secretion, to reduce female secondary sexual characteristics, and to induce virilization, to satisfy patient’s gender identification.
Before starting hormonal therapy, particularly the patient’s-oriented contraindications for testosterone administration must be assessed. The endocrinologist should also evaluate the presence/absence of other risk factors, such as alcoholism, smoking, chronic use of drugs, and intercurrent illness[8].
Before starting hormonal therapy, it is also necessary to discuss fertility options. To preserve fertility in transgender men there are some options available: Oocytes, embryo, and ovarian tissue banking [9]. Oocyte cryopreservation does not immediately require a partner or a sperm donor because there is no fertilization before banking. Embryo cryopreservation after hormonal stimulation and oocyte aspiration offer to AFAB individuals the possibility of a genetically related child with male partner. A sperm donor could be employed to create embryos; in addition, if the uterus is removed in transgender men undergoing gender affirming surgery, a recipient uterus is required (i.e., surrogate mother). Ovarian tissue banking needs a surgical procedure that could be performed during gender affirming surgery [10].
3. The Endocrinological Management of Transgender Women
In transgender women, the main targets of GAHT are to suppress male secondary sexual characteristics and to enhance feminine ones to satisfy patient’s expectations.
Before starting the hormonal treatment, clinicians should evaluate possible risk factors for thromboembolic events such as personal history of deep vein thrombosis or modifiable factors (e.g., obesity or smoking). The presence of pathological conditions that could be worsened by estrogen therapy (e.g., hyperprolactinemia, hypertriglyceridemia, cerebrovascular disease) [11] should be also assessed. Furthermore, fertility preservation techniques (e.g., sperm cryopreservation, surgical sperm extraction, and testicular tissue cryopreservation) should be discussed before starting GAHT[9].
This entry is adapted from the peer-reviewed paper 10.3390/sexes2010009
References
- American Psychological Association. Guidelines for Psychological Practice with Transgender and Gender Nonconforming People. Am. Psychol. J. 2015, 70, 832–864.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; Arlington, VA, USA, 2013.
- Nguyen, H.B.; Chavez, A.M.; Lipner, E.; Hantsoo, L.; Kornfield, S.L.; Davies, R.D.; Epperson, C.N. Gender-Affirming Hor-mone Use in Transgender Individuals: Impact on Behavioral Health and Cognition. Curr. Psychiatry Rep. 2018, 20, 110, doi:10.1007/s11920-018-0973-0.
- T’Sjoen, G.; Arcelus, J.; De Vries, A.L.C.; Fisher, A.D.; Nieder, T.O.; Özer, M.; Motmans, J. European Society for Sexual Medi-cine Position Statement “Assessment and Hormonal Management in Adolescent and Adult Trans People, With Attention for Sexual Function and Satisfaction.” J. Sex. Med. 2020, 17, 570–584, doi:10.1016/j.jsxm.2020.01.012.
- Hembree, W.C.; Cohen-Kettenis, P.; Delemarre-van de Waal, H.A.; Gooren, L.J.; Meyer, W.J.; Spack, N.P.; Tangpricha, V.; Montori, V.M. Endocrine Treatment of Transsexual Persons:An Endocrine Society Clinical Practice Guideline. J. Clin. Endo-crinol. Metab. 2009, 94, 3132–3154, doi:10.1210/jc.2009-0345.
- Hembree, W.C.; Cohen-Kettenis, P.T.; Gooren, L.; Hannema, S.E.; Meyer, W.J.; Murad, M.H.; Rosenthal, S.M.; Safer, J.D.; Tangpricha, V.; T’Sjoen, G.G. Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Socie-ty* Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 3869–3903, doi:10.1210/jc.2017-01658.
- Wierckx, K.; Stuyver, I.; Weyers, S.; Hamada, A.; Agarwal, A.; De Sutter, P.; T’Sjoen, G. Sperm Freezing in Transsexual Women. Arch. Sex. Behav. 2012, 41, 1069–1071, doi:10.1007/s10508-012-0012-x.
- Dekker, M.J.H.J.; Wierckx, K.; Van Caenegem, E.; Klaver, M.; Kreukels, B.P.; Elaut, E.; Fisher, A.D.; van Trotsenburg, M.A.A.; Schreiner, T.; den Heijer, M.; et al. A European Network for the Investigation of Gender Incongruence: Endocrine Part. J. Sex. Med. 2016, 13, 994–999, doi:10.1016/j.jsxm.2016.03.371.
- T’Sjoen, G.; Van Caenegem, E.; Wierckx, K. Transgenderism and Reproduction: Curr. Opin. Endocrinol. Diabetes Obes. 2013, 20, 575–579, doi:10.1097/01.med.0000436184.42554.b7.
- De Roo, C.; Tilleman, K.; T’Sjoen, G.; De Sutter, P. Fertility Options in Transgender People. Int. Rev. Psychiatry 2016, 28, 112–119, doi:10.3109/09540261.2015.1084275.
- T’Sjoen, G.; Arcelus, J.; Gooren, L.; Klink, D.T.; Tangpricha, V. Endocrinology of Transgender Medicine. Endocr. Rev. 2019, 40, 97–117, doi:10.1210/er.2018-00011.