Finger pulse oximeters are widely used to monitor physiological responses to high-altitude exposure, the progress of acclimatization, and/or the potential development of high-altitude related diseases.
- pulse oximetry
- high altitude
- acclimatization
- rest and exercise
- acute mountain sickness
1. Introduction
Wearable sensors can provide athletes, coaches, patients and physicians with useful physiological data, e.g., on the actual cardiovascular and respiratory stress of the individual [1,2,3]. Such information may be gathered by continuous or spot measurements depending on specific objectives. For example, the monitoring of bio-vital markers like heart rate and peripheral oxygen saturation has become a standard of patient care [4] but is also frequently applied by people visiting high altitudes for sight-seeing, trekking, skiing or climbing [5,6]. Simple and inexpensive devices, finger pulse oximeters, are widely used to monitor physiological responses to high-altitude exposure, the progress of acclimatization, and/or the potential development of high-altitude related diseases [7,8,9]. Although there is increasing evidence for the usefulness of pulse oximetry at high altitude some controversy remains [10,11]. This is largely due to differences in individual preconditions, different evaluation purposes, different measurement methods, not considering limitations of devices in certain conditions, the use of different devices, and the lacking ability to interpret data correctly [12].
2. Basic Principles of Functioning, Most Relevant Pitfalls and Possible Countermeasures for Pulse Oximetry Particularly Concerning Healthy People Going to High Altitudes
| Causes of Unreliable SpO2 Readings | Effects on The Measurement Result | Special Influence Conditioned by The High Altitude | Feasible Countermeasures |
|---|---|---|---|
| Excessive movement | Motion artefacts may cause a decrease of measured SpO2 [13,32,33], however modern devices implement advanced algorithm to reduce motion artefacts [14,15,17,33,34]. These devices may be identified by indications such as “motion tolerant” or “motion resistant” [34,35,36]. | With increasing altitude, the temperature drops. This may result in cold extremities and an increased shivering and affects the sensor position and the sensor signal. | During measurement, keep the measuring position steady and avoid too much trembling. |
| Poor probe positioning | The red or infrared light of the sensor may bypass the tissue or too high levels of ambient light hit the light-detector of the sensor [13,15]. This results in a wrong SpO2 reading. | None | An imperfectly fitting of the sensor should be avoided, and the sensor should always be used in the appropriate position. If these countermeasures do not achieve the desired results, measurement at a different site (e.g., earlobe or forehead) may be considered. |
| Excess ambient light | Excessive ambient light can lead to erroneous SpO2 readings. However, modern devices are capable of handling strong ambient light more effectively [13,37]. |
Especially snow-covered areas with high solar radiation can lead to increased ambient light intensity at the sensor. | Protect the sensor from sunlight (e.g., by covering the measuring site). |
| Decreased arterial pressures of oxygen (PaO2) | A decrease in PaO2 (<60 mmHg) results in a significant change in oxygen saturation where small variations of the pressure have a strong effect on the saturation [12,38,39]. | Increasing altitude results in a decreasing PaO2. Especially at altitudes above 3000 m a PaO2 below 60% can be expected [12,40,41]. | To reduce fluctuations in PaO2, SpO2 measurements should be conducted after the person keeps silent and gentle breathing for several minutes. The measurement duration should be extended over a few minutes and the most frequent occurring value should be used [27]. |
| SpO2 saturation below 70% | Devices complying with the international standard ISO 80601-2-61 (medical electrical equipment. Part 2-61: Specific requirements for basic safety and essential performance of pulse oximeter equipment) must measure accurate oxygen saturations (Arms ≤ 4%) between 70–100%. Below 70%, they are less reliable [11,12,16,23,25,42]. | the oxygen saturation is estimated based on human calibration data measured from 100% to 70%. Saturation values below 70% are only based on an extrapolation of this determined curve [13,25]. At high altitudes, however, the occurrence of low saturation values is not abnormal. |
The possibility of a slight deviation of the measured value should be considered if oxygen saturation is below 70%. Especially when comparing data with devices of several manufacturers. |
| Cold-induced vasoconstriction (poor perfusion) | Cold skin temperatures reduce SpO2 reading accuracy [43,44,45]. This effect is based on a reduced blood flow due to cold-induced vasoconstriction [12,31]. However, modern devices can handle this condition and/or report it to the user. These devices may be identified by indications such as “oximeter with perfusion index” or “sensitivity to low perfusion signals”. |
With increasing altitude, the temperature drops. | Warming the measuring site before and preferably during the measurement (e.g., using heating pads). |
| Skin pigmentation | Pulse oximeters are possibly less accurate during hypoxia in dark-skinned individuals at lower saturation (<80%) resulting in overestimations [46,47]. Feiner et al. mentioned [48]: “further study is needed to confirm these observations in the relevant populations.” However, an actual study is consistent with Bickler et al. and Feiner et al. [49]. |
At high altitude, the occurrence of saturation values below 80% is not abnormal [12,50]. | Until the scientific data is more definite, the possibility of a slight overestimation (about +2% [51]) of the measured value should be kept in mind when interpreting the data for a person with oxygen saturation below approx. 90% combined with a dark pigmentation of the skin. |
| Nail polish | Some fingernail polish can lower the SpO2 readings [48]. Previous studies, however, have shown that the variance is not clinically relevant using actual devices [51,52,53,54]. | None | Especially with older devices, the nail polish should be removed to avoid variations in the measurement accuracy. However, the deviation in the SpO2 readings is less than 2% [53,54]. |
| Limited knowledge of technology (devices) and data interpretation | A lack of knowledge regarding device application and interpretation of the measurement data can lead to incorrect conclusions [14,23]. | Conditions at high altitudes complicate the use of the device and the accurate interpretation of the data [12,27,50]. | As Tannheimer et al. [50] concluded it “requires an experienced examiner who can include altitude anamnesis, clinical examination and mountaineering aspects in the overall assessment” to avoid possible pitfalls during SpO2 measurement and interpretation on high altitudes. |
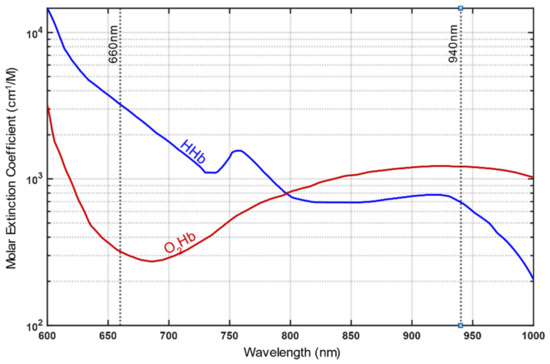
| Dyshemoglobins (carboxyhemoglobin and methemoglobin) | Based on an absorption of the red and infrared light, methemoglobin (MetHb) and carboxyhemoglobin (HbCO) cause SpO2 overestimation and mask serious hypoxia [14,23,48]. However, as already mentioned, certain multiple-wavelengths devices are capable of detecting dyshemoglobins. | Unlikely at high altitude, however, it can be a danger using a cooking stove in small, enclosed areas like tents. In the worst case, this can lead to carbon monoxide poisoning [12,55]. | When using devices that are not capable of analyzing dyshemoglobins, possible carbon monoxide poisoning should be considered if the person has remained in a small, enclosed space for an extended period while a combustion process (e.g., a stove) has taken place. Symptoms of carbon monoxide poisoning may include headache, nausea and drowsiness. However, these symptoms are similar to those associated to altitude sickness [56]. |
Reference (Editors will rearrange the references after the entry is submitted)
- Li, R.T.; Kling, S.R.; Salata, M.J.; Cupp, S.A.; Sheehan, J.; Voos, J.E. Wearable Performance Devices in Sports Medicine. Sports Health Multidiscip. Approach 2016, 8, 74–78.
- Ma, C.Z.; Wong, D.W.; Lam, W.K.; Wan, A.H.; Lee, W.C. Balance Improvement Effects of Biofeedback Systems with State-of-the-Art Wearable Sensors: A Systematic Review. Sensors 2016, 16, 434.
- Altini, M.; Casale, P.; Penders, J.; Ten Velde, G.; Plasqui, G.; Amft, O. Cardiorespiratory fitness estimation using wearable sensors: Laboratory and free-living analysis of context-specific submaximal heart rates. J. Appl. Physiol. 2016, 120, 1082–1096.
- Welsh, E.J.; Carr, R. Pulse oximeters to self monitor oxygen saturation levels as part of a personalised asthma action plan for people with asthma. Cochrane Database Syst. Rev. 2015, 9, CD011584.
- Otani, S.; Miyaoka, Y.; Ikeda, A.; Ohno, G.; Imura, S.; Watanabe, K.; Kurozawa, Y. Evaluating Health Impact at High Altitude in Antarctica and Effectiveness of Monitoring Oxygen Saturation. Yonago Acta Med. 2020, 63, 163–172.
- Tannheimer, M.; Lechner, R. The correct measurement of oxygen saturation at high altitude. Sleep Breath. 2019, 23, 1101–1106f
- Koehle, M.S.; Guenette, J.A.; Warburton, D.E. Oximetry, heart rate variability, and the diagnosis of mild-to-moderate acute mountain sickness. Eur. J. Emerg. Med. 2010, 17, 119–122.
- Burtscher, M.; Flatz, M.; Faulhaber, M. Prediction of susceptibility to acute mountain sickness by SaO2 values during short-term exposure to hypoxia. High Alt. Med. Biol. 2004, 5, 335–340.
- Tannheimer, M.; Thomas, A.; Gerngross, H. Oxygen saturation course and altitude symptomatology during an expedition to broad peak (8047 m). Int. J. Sports Med. 2002, 23, 329–335.
- Reuland, D.S.; Steinhoff, M.C.; Gilman, R.H.; Bara, M.; Olivares, E.G.; Jabra, A.; Finkelstein, D. Prevalence and prediction of hypoxemia in children with respiratory infections in the Peruvian Andes. J. Pediatr. 1991, 119, 900–906.
- Ottestad, W.; Kåsin, J.I.; Høiseth, L.Ø. Arterial Oxygen Saturation, Pulse Oximetry, and Cerebral and Tissue Oximetry in Hypobaric Hypoxia. Aerosp. Med. Hum. Perform. 2018, 89, 1045–1049.
- Luks, A.M.; Swenson, E.R. Pulse oximetry at high altitude. High Alt. Med. Biol. 2011, 12, 109–119.
- Chan, E.D.; Chan, M.M.; Chan, M.M. Pulse oximetry: Understanding its basic principles facilitates appreciation of its limitations. Respir. Med. 2013, 107, 789–799.
- Jubran, A. Pulse oximetry. Crit. Care 2015, 19, 272.
- Tamura, T. Current progress of photoplethysmography and SPO2 for health monitoring. Biomed. Eng. Lett. 2019, 9, 21–36.
- Lipnick, M.S.; Feiner, J.R.; Au, P.; Bernstein, M.; Bickler, P.E. The Accuracy of 6 Inexpensive Pulse Oximeters Not Cleared by the Food and Drug Administration: The Possible Global Public Health Implications. Anesth. Analg. 2016, 123, 338–345.
- Petterson, M.T.; Begnoche, V.L.; Graybeal, J.M. The effect of motion on pulse oximetry and its clinical significance. Anesth. Analg. 2007, 105, S78–S84.
- Zaouter, C.; Zavorsky, G.S. The measurement of carboxyhemoglobin and methemoglobin using a non-invasive pulse CO-oximeter. Respir. Physiol. Neurobiol. 2012, 182, 88–92.
- Feiner, J.R.; Rollins, M.D.; Sall, J.W.; Eilers, H.; Au, P.; Bickler, P.E. Accuracy of carboxyhemoglobin detection by pulse CO-oximetry during hypoxemia. Anesth. Analg. 2013, 117, 847–858.
- Prahl, S. Tabulated Molar Extinction Coefficient for Hemoglobin in Water; Oregon Medical Laser Center: Portland, OR, USA, 1998.
- Nitzan, M.; Romem, A.; Koppel, R. Pulse oximetry: Fundamentals and technology update. Med. Devices 2014, 7, 231–239.
- Center for Devices and Radiological Health. Pulse Oximeters—Premarket Notification Submissions [510 (k)s] Guidance for Industry and Food and Drug Administration Staff; U.S. Department of Health and Human Services: Washington, DC, USA, 2013.
- Pretto, J.J.; Roebuck, T.; Beckert, L.; Hamilton, G. Clinical use of pulse oximetry: Official guidelines from the Thoracic Society of Australia and New Zealand. Respirology 2014, 19, 38–46.
- Hudson, A.J.; Benjamin, J.; Jardeleza, T.; Bergstrom, C.; Cronin, W.; Mendoza, M.; Schultheis, L. Clinical Interpretation of Peripheral Pulse Oximeters Labeled “Not for Medical Use”. Ann. Fam. Med. 2018, 16, 552–554.
- Luks, A.M.; Swenson, E.R. Pulse Oximetry for Monitoring Patients with COVID-19 at Home. Potential Pitfalls and Practical Guidance. Ann. Am. Thorac. Soc. 2020, 17, 1040–1046.
- Smith, R.N.; Hofmeyr, R. Perioperative comparison of the agreement between a portable fingertip pulse oximeter v. a conventional bedside pulse oximeter in adult patients (COMFORT trial). S. Afr. Med. J. 2019, 109, 154–158.
- Ross, E.M.; Matteucci, M.J.; Shepherd, M.; Barker, M.; Orr, L. Measuring arterial oxygenation in a high altitude field environment: Comparing portable pulse oximetry with blood gas analysis. Wilderness Environ. Med. 2013, 24, 112–117.
- Bradke, B.; Everman, B. Investigation of Photoplethysmography Behind the Ear for Pulse Oximetry in Hypoxic Conditions with a Novel Device (SPYDR). Biosensors 2020, 10, 34.
- Longmore, S.K.; Lui, G.Y.; Naik, G.; Breen, P.P.; Jalaludin, B.; Gargiulo, G.D. A Comparison of Reflective Photoplethysmography for Detection of Heart Rate, Blood Oxygen Saturation, and Respiration Rate at Various Anatomical Locations. Sensors 2019, 19, 1874.
- Yamaya, Y.; Bogaard, H.J.; Wagner, P.D.; Niizeki, K.; Hopkins, S.R. Validity of pulse oximetry during maximal exercise in normoxia, hypoxia, and hyperoxia. J. Appl. Physiol. 2002, 92, 162–168.
- Lorente-Aznar, T.; Perez-Aguilar, G.; García-Espot, A.; Benabarre-Ciria, S.; Mendia-Gorostidi, J.L.; Dols-Alonso, D.; Blasco-Romero, J. Estimation of arterial oxygen saturation in relation to altitude. Med. Clin. 2016, 147, 435–440.
- Barker, S.J. “Motion-resistant” pulse oximetry: A comparison of new and old models. Anesth. Analg. 2002, 95, 967–972.
- Clarke, G.W.J.; Chan, A.D.C.; Adler, A. Effects of motion artifact on the blood oxygen saturation estimate in pulse oximetry. In Proceedings of the 2014 IEEE International Symposium on Medical Measurements and Applications, Lisabon, Portugal, 11–12 June 2014; pp. 1–4.
- Giuliano, K.K.; Higgins, T.L. New-generation pulse oximetry in the care of critically ill patients. Am. J. Crit. Care 2005, 14, 26–37.
- Louie, A.; Feiner, J.R.; Bickler, P.E.; Rhodes, L.; Bernstein, M.; Lucero, J. Four Types of Pulse Oximeters Accurately Detect Hypoxia during Low Perfusion and Motion. Anesthesiology 2018, 128, 520–530.
- Cannesson, M.; Talke, P. Recent advances in pulse oximetry. F1000 Med. Rep. 2009, 1, 66.
- Fluck, R.R.; Schroeder, C.; Frani, G.; Kropf, B.; Engbretson, B. Does ambient light affect the accuracy of pulse oximetry? Respir. Care 2003, 48, 677–680.
- World Health Organization. Pulse Oximetry Training Manual; WHO Press: Geneva, Switzerland, 2011.
- Hafen, B.B.; Sharma, S. Oxygen Saturation. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2020.
- Peacock, A.J. ABC of oxygen: Oxygen at high altitude. BMJ 1998, 317, 1063–1066.
- West, J.B. High-altitude medicine. Am. J. Respir. Crit. Care Med. 2012, 186, 1229–1237.
- Severinghaus, J.W.; Naifeh, K.H.; Koh, S.O. Errors in 14 pulse oximeters during profound hypoxia. J. Clin. Monit. 1989, 5, 72–81.
- Jeong, I.C.; Yoon, H.; Kang, H.; Yeom, H. Effects of skin surface temperature on photoplethysmograph. J. Healthc. Eng. 2014, 5, 429–438.
- Khan, M.; Pretty, C.G.; Amies, A.C.; Elliott, R.; Shaw, G.M.; Chase, J.G. Investigating the Effects of Temperature on Photoplethysmography. IFAC PapersOnLine 2015, 48, 360–365.
- Khan, M.; Pretty, C.G.; Amies, A.C.; Elliott, R.; Chiew, Y.S.; Shaw, G.M.; Chase, J.G. Analysing the effects of cold, normal, and warm digits on transmittance pulse oximetry. Biomed. Signal Process. Control 2016, 26, 34–41.
- Feiner, J.R.; Severinghaus, J.W.; Bickler, P.E. Dark skin decreases the accuracy of pulse oximeters at low oxygen saturation: The effects of oximeter probe type and gender. Anesth. Analg. 2007, 105, S18–S23.
- Bickler, P.E.; Feiner, J.R.; Severinghaus, J.W. Effects of skin pigmentation on pulse oximeter accuracy at low saturation. Anesthesiology 2005, 102, 715–719.
- Ralston, A.C.; Webb, R.K.; Runciman, W.B. Potential errors in pulse oximetry. III: Effects of interferences, dyes, dyshaemoglobins and other pigments. Anaesthesia 1991, 46, 291–295.
- Sjoding, M.W.; Dickson, R.P.; Iwashyna, T.J.; Gay, S.E.; Valley, T.S. Racial Bias in Pulse Oximetry Measurement. N. Engl. J. Med. 2020, 383, 2477–2478.
- Tannheimer, M. The Use of Pulse Oximetry at High Altitude. Res. Investig. Sports Med. 2020, 6, 10–13.
- Rodden, A.M.; Spicer, L.; Diaz, V.A.; Steyer, T.E. Does fingernail polish affect pulse oximeter readings? Intensive Crit. Care Nurs. 2007, 23, 51–55.
- Chan, M.M.; Chan, M.M.; Chan, E.D. What is the effect of fingernail polish on pulse oximetry? Chest 2003, 123, 2163–2164.
- Yeganehkhah, M.; Dadkhahtehrani, T.; Bagheri, A.; Kachoie, A. Effect of Glittered Nail Polish on Pulse Oximetry Measurements in Healthy Subjects. Iran. J. Nurs. Midwifery Res. 2019, 24, 25–29.
- Ballesteros-Pena, S.; Fernandez-Aedo, I.; Picon, A.; Lorrio-Palomino, S. Influence of nail polish on pulse oximeter readings of oxygen saturation: A systematic review. Emergencias 2015, 27, 325–331.
- Foutch, R.G.; Henrichs, W. Carbon monoxide poisoning at high altitudes. Am. J. Emerg. Med. 1988, 6, 596–598.
- Buchheit, M.; Simpson, B.M.; Garvican-Lewis, L.A.; Hammond, K.; Kley, M.; Schmidt, W.F.; Aughey, R.J.; Soria, R.; Sargent, C.; Roach, G.D.; et al. Wellness, fatigue and physical performance acclimatisation to a 2-week soccer camp at 3600 m (ISA3600). Br. J. Sports Med. 2013, 47, i100–i106.
This entry is adapted from the peer-reviewed paper 10.3390/s21041263
