Since its initial approval in 1989 by the US Food and Drug Administration for the treatment of blepharospasm and other facial spasms, botulinum toxin (BoNT) has evolved into a therapeutic modality for a variety of neurological and non-neurological disorders. With respect to neurologic movement disorders, BoNT has been reported to be effective for the treatment of dystonia, bruxism, tremors, tics, myoclonus, restless legs syndrome, tardive dyskinesia, and a variety of symptoms associated with Parkinson’s disease. More recently, research with BoNT has expanded beyond its use as a powerful muscle relaxant and a peripherally active drug to its potential central nervous system applications in the treatment of neurodegenerative disorders. Although BoNT is the most potent biologic toxin, when it is administered by knowledgeable and experienced clinicians, it is one of the safest therapeutic agents in clinical use. The primary aim of this article is to provide an update on recent advances in BoNT research with a focus on novel applications in the treatment of movement disorders.
1. Introduction
Clostridium botulinum, an anaerobic, rod-shaped bacterium, produces a neurotoxin called botulinum toxin (BoNT) during sporulation [
1,
2,
3]. BoNT is the most potent biological toxin, as it causes botulism manifested by paralysis of muscles and eventual fatal respiratory failure [
4,
5]. When an action potential arrives at the cholinergic presynaptic nerve terminal, there is an influx of calcium into the presynaptic terminal, which then facilitates acetylcholine vesicle fusion with the presynaptic membrane; this fusion is facilitated by a group of proteins referred to as SNARE (soluble N-ethylmaleimide-sensitive factor attachment receptor) proteins, which include SNAP 25 (25 kD synaptosomal-associated protein) and Syntaxin [
6,
7]. BoNT acts at the cholinergic presynaptic nerve terminal by cleaving and inactivating SNARE proteins, thus inhibiting release of acetylcholine, which in turn prevents muscle contraction and results in local weakness and paralysis [
7,
8]. BoNT acts at both the extrafusal and intrafusal muscle fibers, thereby preventing contraction of both agonist and antagonist muscles [
8,
9]. This biologic effect of BoNT has been turned into an advantage in patients troubled by involuntary muscle contractions, excessive secretions, pain, and other conditions [
7]. The paralytic effects of BoNT were initially described in 1817 by Justinus Kerner, a German physician, who suggested that the toxin may be potentially useful in the treatment of St. Vitus’ dance, hypersalivation, and hyperhidrosis [
10]. The mechanism of action of BoNT injections to account for the typical 3–4 months of duration has not been fully elucidated, and the original proposal that axonal sprouting occurs at the presynaptic nerve terminal after the injection, after which time the neuromuscular junction integrity is restored when the original nerve terminals regain their exocytic function, hence necessitating repeat injections [
11], has been challenged [
12].
In 1981, Dr. Jankovic initially injected BoNT into a patient for treatment of blepharospasm (BSP) [
10] and subsequently published the results of the first double-blind, placebo-controlled trial of BoNT in cranial–cervical dystonia [
13]. The results of this trial, along with additional data, were used by the United States Food and Drug Administration (FDA) to approve BoNT in 1989 for the treatment of BSP and facial nerve disorders such as hemifacial spasm (HFS) [
14]. Although only BoNT types A and B have been approved for clinical use by the FDA, there are a total of eight different subtypes: BoNT A to H [
6].
There are currently four FDA approved BoNT formulations: the three types of botulinum toxin type A (BoNTA) available are onabotulinumtoxinA (Botox; Allergan, CA, USA), abobotulinumtoxinA (Dysport; Ipsen-Pharma, UK), and incobotulinumtoxinA (Xeomin; Merz Pharma, Germany); rimabotulinumtoxinB (Myobloc in the USA; Supernus Pharmaceuticals, Inc, Rockville, MD; Neurobloc in Europe, Sloan Pharma, Switzerland) is a BoNTB preparation [
6,
10].
There are several BoNT preparations that are currently in development but have not yet been approved by the FDA. DaxibotulinumtoxinA is a novel BoNTA preparation that was recently evaluated in a phase 3 trial (ASPEN-1) in cervical dystonia (
https://www.businesswire.com/news/home/20201014005360/en/). This study enrolled 301 patients from 60 sites in the U.S., Canada, and Europe and confirmed the findings of an earlier phase 2 study [
15] in that it found that daxibotulinumtoxinA is safe and effective. Interestingly, at doses of 125 U, it has a median duration of effect (based on the median time to loss of 80% of the peak treatment effect) of 24 weeks. This relatively long duration of action offers potential advantage over other formulations in that it may allow increasing the intervisit interval beyond the conventional 3–4 months. LanbotulinumtoxinA (Prosigne; Shanghai, China) is a new preparation of BoNTA marketed chiefly in Asia [
16,
17].
The doses of different formulations are not interchangeable, but based on prior studies, the following ratios are often used in clinical practice when switching from one to another BoNT product to achieve similar results: onabotulinumtoxinA:incobotulinumtoxinA = 1:1; onabotulinumtoxinA:abobotulinumtoxinA = 1:2.5, and onabotulinumtoxinA:rimabotulinumtoxinB = 1:50 [
10].
With long term use of BoNT, there is a risk of developing neutralizing antibodies (NAbs) [
18], and patients may stop responding to BoNT. Factors that increase the risk of developing resistance to BoNT include a high protein load in some formulations, large individual and cumulative doses of BoNT, and short intervisit intervals, especially booster injections [
18,
19,
20,
21,
22,
23]. Immunogenicity varies among the different products and has been reported as low as 0% for incobotulinumtoxinA and as high as 42.4% for rimabotulinumtoxinB [
20]. Brin et al. [
23] noted a 1.2% frequency of NAbs based on mouse protection assay (MPA) in patients treated for cervical dystonia with onabotulinumtoxinA. In contrast, Albrecht et al. [
18] reported a prevalence of 14% of NAbs in 596 treated with BoNTA, mostly abobotulinumtoxinA, for a mean of 5.3 years based on mouse hemidiaphragm assay (MHDA). Since biological assays such as MPA and MHDA are difficult to perform and they involve sacrificing animals, there is a huge unmet need to develop a simple, inexpensive, sensitive, and specific test for BoNT-blocking antibodies. If a patient reports lack of improvement (less than 25%) after at least two or three consecutive treatment visits, this raises a high level of suspicion of immunoresistance [
20]. In this case, unilateral brow injection may be performed as a clinically useful test [
20]. This involves injection of BoNT in the right medial eyebrow and reassessing in 1–2 weeks for paralysis of the right procerus/corrugator as manifested by asymmetric frowning, which would disprove immunoresistance [
20]. We have not included spasticity in this article, as we believe it is beyond the scope of this review. The reader is referred to some recent reviews on this topic [
24,
25,
26].
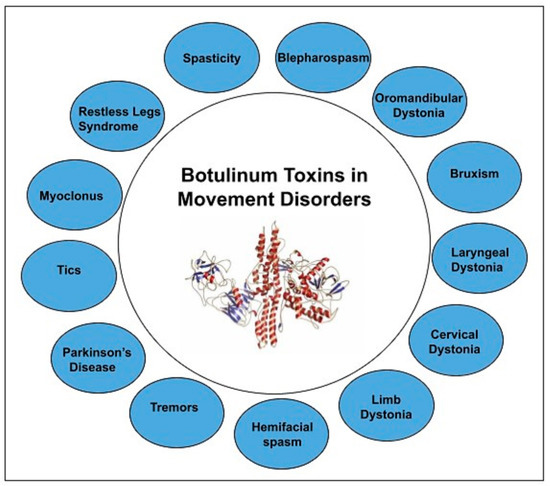
Our manuscript provides a comprehensive review of botulinum toxin in movement disorders. depicts the variety of movement disorders where botulinum toxin is used for therapeutic purposes.
Figure 1. BoNT in Movement disorders.
2. Discussion of BoNT Use in Different Indications
2.1. Dystonia
Dystonia is defined as a movement disorder characterized by sustained or intermittent muscle contractions causing abnormal, often repetitive, patterned movements, postures, or both [
27,
28].
It is frequently associated with activity but may also be present at rest and worsens with stress, anxiety, and fatigue [
29]. The prevalence has been reported to range between 15 and 225 per 100,000 individuals [
30].
We conducted a PubMed search on 28 May 2020; using the title words botulinum and dystonia, a total of 438 articles were identified. 340 of these were in English and were human studies. Of the 340 articles, 71 were review articles, 154 were either prospective or retrospective trials, 32 were randomized controlled trials (RCTs), 58 were case reports, 6 were commentaries, 8 were unavailable for review, and 11 articles were irrelevant. The clinical composition of 340 articles were different types of dystonia: 2 axial, 1 blepharospasm (BSP), 49 multiple types, 186 cervical dystonia (CD), 1 cranial, 15 unspecified, 17 laryngeal, 28 limb, 5 lingual, 30 oromandibular dystonia (OMD), 1 torsion, and 5 tardive.
2.2. Hemifacial Spasm
Hemifacial spasm (HFS) is a peripherally induced unilateral facial movement disorder characterized by irregular, clonic, or tonic contractions of muscles innervated by the ipsilateral facial nerve. Its estimated prevalence is around 10 in 100,000 [
174,
175]. The condition usually begins as spasms of lower eyelid on one side of the face, which eventually spreads to upper eyelid and other muscles in ipsilateral face, often associated with elevation of ipsilateral eyebrow referred to as the “other Babinski sign” [
34,
176]. The estimated prevalence is 14.5 and 7.4 per 100,000 in women and men, respectively [
174]. Primary HFS is thought to be related to compression of the facial nerve at the exit zone by an aberrant blood vessel loop. Secondary HFS is related to prior facial nerve injury or Bell’s palsy or brain stem damage [
177]; 76% and 21% of HFS are primary and secondary respectively [
178]. There is some evidence that facial motor nucleus excitability is reduced after BoNT injections [
179].
We conducted a PubMed search on 21 April 2020. Using botulinum and hemifacial as title words, we identified 157 articles; of these, 118 were in English and were human studies. Of the 118 articles, 9 were review articles, 74 were either prospective or retrospective trials, 13 were RCTs, 5 were case reports, 6 were commentaries, and 11 articles were irrelevant.
In 1985, Savino et al. published one of the earliest case series in 15 patients who experienced relief of HFS after BoNT injections [
180]. In a series of patients with BSP (
n = 70), HFS (
n = 13), CD (
n = 195), hand dystonia (
n = 22), and oromandibular dystonia (
n = 45) who underwent BoNT injections, 94%, 92%, 90%, 77%, and 73% experienced relief of their symptoms, respectively [
181]. In another series, 98% of 130 patients with HFS patients experienced relief of symptoms after BoNT injection [
182]. In a retrospective review of 100 HFS patients who were treated with a mean dose of 28 U of onabotulinumtoxinA and were followed for 4 years, showed a mean duration of effect of around 3.1 months and latency to onset of effect of 7.1 days [
183]. There are numerous prospective and retrospective trial which evaluated the use of BoNTA injections that showed safety and benefit in patients with HFS [
184,
185,
186,
187,
188,
189]. Cakmur et al. evaluated pretarsal versus preseptal injections in 28 and 25 patients with HFS and BSP, respectively, and found that pretarsal BoNTA had better relief of symptoms, longer duration of effect, and lower incidence of ptosis [
190]. Results from another study of 72 HFS and 38 BSP patients with a crossover design concluded that pretarsal and preseptal injections provided similar beneficial effects; however, the pretarsal group had longer duration of benefit [
191]. A systematic review that was published recently stated that they did not identify RCTs of BoNTA in HFS [
192]. In our practice, we inject mainly in the pretarsal portion of the orbicularis oculi in patients with BSP and HFS. Cochrane review (based on a single study with study size = 11) concluded that the benefit rate of BoNT in HFS was between 76–100% and that due to this effect size, it would be extremely hard and unethical to conduct new placebo-controlled trials with a large sample size [
193].
Side effects of BoNT for HFS include ptosis (7.8–36%), double vision (1.6%), blurred vision (2.5%), dry eyes/exposure keratitis (2.5%), dysphagia (5.5%), facial droop (3.5–5.5%), eye lid swelling/ecchymosis (3.8%), nausea (2.5%), and conjunctival redness [
190,
194,
195].
Tunc et al. [
196] assessed BoNT injections efficacy in 69 patients with idiopathic HFS (
n = 46) and those with HFS due to definite neurovascular compression (
n = 23) and found that those with idiopathic HFS had more robust improvement with BoNT. Although some favor surgical vascular decompression as a treatment of HFS, most neurologists prefer BoNT, as there is a lower risk of permanent adverse effects such as facial paralysis and deafness [
197]. discusses the various randomized trials involving BoNT and HFS.
2.3. Tremors
Tremor, an involuntary, rhythmic, oscillatory movement of a body part, is the most common movement disorder in a movement disorder clinic [
204,
205]. When oral medications do not adequately control the tremors, as is the case in 30% of patients with essential tremor (ET), BoNT should be considered as a therapeutic option [
206]. We conducted a PubMed search on 9 July 2020; using botulinum and tremor as title words, a total of 49 articles were identified. Of those, 43 of these were in English and were human studies. Of the 43 articles, 4 were review articles, 18 were either prospective or retrospective trials, 8 were RCTs, 12 were case reports, and 1 was commentary. The clinical subsets of the 43 articles were 8 ET, 2 ET PD, 3 jaw tremor, 6 palatal, 5 multiple tremor types, 9 vocal, 1 each for PD, tremor/tic, orthostatic, head tremor with CD, neuropathy-associated, head tremor, and multiple sclerosis associated with Holmes tremor.
In 1981, Jankovic and colleagues reported the earliest series of 51 patients with different tremor types who benefited from BoNT [
207]. Trosh and Pullman published a prospective study with 26 patients (12 and 14 of PD and ET, respectively) who also benefited from BoNT [
208]. Fixed doses, limited muscles being injected, and complicating weakness postinjections initially made BoNT use for tremors unsatisfactory [
205]. In 2015, a series of 28 PD patients with tremors underwent muscle selection of incobotulinumtoxinA and patients improved at 16 weeks [
209]. In an open-label prospective trial, 31 ET patients received 3 cycles of BoNTA based on kinematic analysis guided muscle selection and dose administered [
206]; it showed that BoNTA reduced tremor by 47.7% at 6 weeks and the improvement lasted 18–30 weeks. In a series of 10 patients with ET who received BoNTA using kinematics every 16 weeks, a 33.8% functional improvement was noted when selected muscles were injected [
210]. The series was later expanded to include 28 PD and 24 ET patients who were injected with BoNTA using computer-based kinematics [
210].
Mittal and Jankovic (2019) had provided a systematic review of BoNT in tremors [
204] and concluded that most studies were open-label and that there was a need for well-designed controlled trials of BoNT in the treatment of ET and PD tremors. In a retrospective analysis by Niemann and Jankovic [
211] of 91 patients (53 ET, 31 dystonic, 9 PD, 1 cerebellar), 81.3% of whom received injections into flexor carpi radialis or ulnaris (mean dose per limb 71.8 units of onabotulinumtoxinA), only 12.2% had transient weakness. This is in contrast to earlier double-blind, placebo-controlled studies by Jankovic et al. [
212] and Brin et al. [
213], during which the wrist extensors were also injected and, as a result, many patients experienced finger extensor weakness. Therefore, we no longer inject the extensor hand muscles [
211]. In a series of 19 patients with proximal tremors, injections in muscles such as supra/infraspinatus, teres major/minor, biceps, triceps, deltoid, and pectoralis major resulted in at least moderate benefit in 63%, but 15% had no benefit [
214]. In 20 patients with severe ET, BoNT (mean total dose 95.5 ± 40.58 per patient) improvement was noted in activities of daily living and in severity tremor scale [
215]. The investigators also concluded that excluding extensor carpi muscle did not affect efficacy of BoNT. lists RCTs associated with tremors and BoNT.
Table 6. RCTs in tremors and BoNT.
Parkinson’s Disease
PD is a neurodegenerative disease with incidence around 118 per 100,000 person years [
223]. There are a variety of symptoms in PD that have been amenable to the treatment with BoNT including hand tremors, jaw tremors, axial dystonia, rectal dystonia, freezing of gait, sialorrhea, and levodopa-induced dyskinesias [
14,
204,
224]. We conducted a PubMed search on 11 July 2020; using botulinum and Parkinson as title words, a total of 58 articles were identified. Of these, 49 of these were in English and were human studies. Of the 49 articles, 7 were review articles, 19 were either prospective or retrospective trials, 14 were RCTs, 7 were case reports, 1 was unavailable for review, and 1 was a commentary. lists PD-related conditions amenable to BoNT treatment. lists RCTs associated with PD and BoNT.
Table 7. Parkinson’s disease (PD)-related conditions amenable to treatment with BoNT.
Table 8. RCT associated with PD and BoNT.
This entry is adapted from the peer-reviewed paper 10.3390/toxins13010042