Osteoporotic spine fractures (OSF) are common sequelae of osteoporosis. OSF are directly correlated with increasing age and incidence of osteoporosis. OSF are treated conservatively or surgically. We review the current state of the art in the field of wearable robots for trunk support.
- osteoporotic spine fracture
- spinal orthosis
- exoskeleton
- wearable robotics
- active orthosis
1. introduction
At present, 125 million people are aged 80 years or older. By 2050, there will be almost 434 million people in this age group worldwide. Between 2010 and 2060, the number of people aged above 65 years will increase from 17.4% to 29.5% of the total population [1]. One in two women and one in five men over 50 years of age will suffer an osteoporotic fracture. During the year 2000, there were an estimated 9 million new fragility fractures worldwide, of which 1.4 million were symptomatic vertebral fractures [2]. Osteoporotic spine fractures (OSF) are more common in women compared to men (a 4:1 ratio). They cause severe pain, disability, deformities, and even death. This has a significant impact on their activities of daily living (ADLs) and quality of life (QOL) [3,4]. Hence, OSF are gaining well-deserved recognition in the medical field [5]. Osteoporotic fractures exert a tremendous burden on older people and healthcare budgets.
Biomechanics of the Spine
The human spine, with the lumbar region in particular, carries three major motions: sagittal plane flexion/extension, lateral bending, and axial rotation, of which the sagittal plane flexion/extension is the most significant in terms of the range of movement (ROM, see Figure 1).
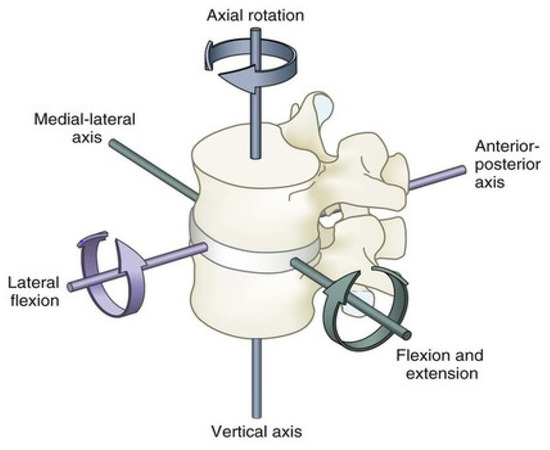
Figure 1. Standard range of movements for the human lumbar spine.
The overall ROM of the lumbar spine itself is usually supported by two main groups of muscle. We may classify them as the anterior and the posterior groups of muscle. Models of the human spine suggest that the lumbar spine can be modeled as one additional joint in the contribution for flexion and extension on the sagittal plane [6]. Lumbar spine ROM parameters are as follows: flexion 40–60 degrees, extension 20–35 degrees, lateral bending 15–20 degrees, and axial rotation 3–18 degrees.
The posterior spinal muscle group consists of a thick superficial layer of thoracolumbar fascia, which is attached to the spinous processes and the supraspinous ligaments. It extends bilaterally to cover the erector spinae muscles (the iliocostalis, longissimus, spinalis muscles). Beneath this thick fascia lies the erector spinae muscles which arise from the sacrum, iliac crest, and the spinous processes of the thoracolumbar spine. They act as part of the posterior column. Together with the facet joint and posterior ligamentous complexes, these muscles form the posterior tension band for spinal stabilization, and, most importantly, they are also the main muscles for thoracolumbar spine ROM.
The anterior group of spinal muscles consists of the quadratus lumborum and the psoas major muscles. They do not contribute to the overall spinal stability, but they help with ROM of the spine. Hence, the posterior muscle group is considered the principle muscle group for thoracolumbar spinal movements (see Figure 2).
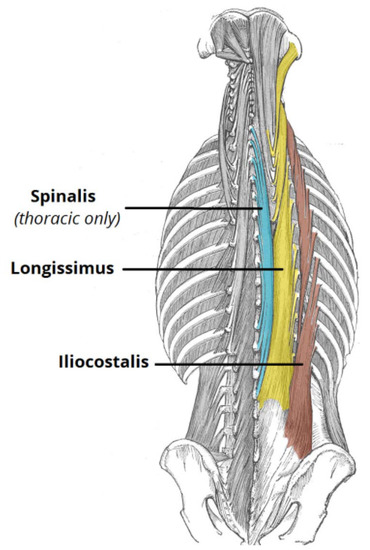
Figure 2. The principle posterior spinal muscles.
Human vertebral bodies and intervertebral discs together are designed to resist large compression forces (ranging between 2 N and 14,000 N), while the shearing forces are mostly loaded onto the posterior facet joints (ranging between 600 to 2800 N). Each lumbar intervertebral disc can also bear shearing forces between 380 and 760 N [7].
The mean back extensor strength of human lumbar spine decreases with age, and it measures from 284 N, to 267 N, 262 N, and 172 N for females in age groups between 40–49, 50–59, 60–69, and 70–79, respectively [8]. The posterior spinal muscles play a crucial role in the posterior tension band that maintains our normal posture by balancing the biomechanical tendency of the spine to fall forward. This function coincidentally reduces mechanical stress on the vertebral bodies [9].
There are various biomechanical models which have been developed to estimate lumbar spinal loading and forces [10]. Recent studies estimated these forces during symmetric lifting and asymmetric lifting tasks using a whole-body musculoskeletal modelling approach and found that torsion of the spine during asymmetric lifting required more trunk muscle contractions than symmetric lifting. Lifting with a twisting movement of the spine increased the three-dimensional lumbar spinal forces at the L5/S1, L4/L5, and L3/L4 joints from 3000 N to 5000 N. The torque for asymmetric lifting was also greater and up to 180Nm for a 12kg load [11,12].
Flexion-relaxation of the posterior spinal muscles occurs in positions of quiet standing with substantial trunk flexion. One study found that the myoelectric activity (EMG) is diminished on 40 degrees flexion of the lumbar vertebrae, and it is nearly absent in quiet standing at maximum flexion, i.e., no further muscle contractions are required. The forces required to maintain the equilibrium at the full range flexion, provided by the passive muscle tissue, tendons, and ligaments, were measured to be 700 N [13].
2. Passive Spine Braces in the Treatment of Osteoporotic Spine Fractures (OSF)
Treatment of OSF can be classified as surgical or non-surgical, depending on the morphology of the fracture pattern as well as the clinical condition of the patient. Stable fracture patterns include those of vertebral body compression fractures which involve only the anterior spinal column while the posterior muscular–ligamentous complex remains intact [14,15]. These stable OSF are treated non-surgically.
The start of non-surgical treatment for stable OSF usually consists of initial bed rest, analgesia, early physiotherapy, early rehabilitation, and a rigid spinal brace (orthosis). Pain related to the OSF may last up to 4 months [16]. Spinal braces are usually applied for a minimum of 3 weeks and up to 12 months, depending on the patient’s symptoms and the fracture healing progress [17,18,19,20]. Patients are encouraged to apply the spinal brace at all times unless they are lying down, for example, during bedrest. Typically, these braces are usually fixed and rigid (for example, TLSO, thoracolumbar spinal orthosis, see Figure 3) [21].

Figure 3. Adapted from Trulife—C.A.S.H. Orthosis.
Progressive vertebral body collapse is a known complication for patients with OSF. It is a potential complication due to lack of proper spinal support. This may eventually result in progressive kyphotic deformity of the spine. Radiologically, this is regularly seen as worsening kyphosis of the spine on follow-up, when compared to initial radiological images taken at time of injury. Hyper-kyphosis of the spine itself imposes further stress on the anterior spinal column. This increases the risk of new fractures and disrupts normal balance, thereby increasing the risk of falls and, as a result, other injuries and fractures [22]. The most important point to note is that progressive vertebral body collapse with kyphotic deformity may result in conversion of a benign OSF into a burst fracture type pattern, which will lead to neurological compromise from a spinal cord with cauda equina compression.
The goals of traditional orthotic treatment involve a combination of limiting motion and correcting posture, thus reducing pain and fatigue, and improving overall function or participation at rehabilitation. A spinal brace in OSF can prevent pain from truncal movements by stabilizing the spine [23] through axial spinal support and reducing the effort of the para-spinal muscles. This in turn will promote fracture healing [24] (see Figure 4). The effects of these braces on the stabilization of the injured vertebral body have been demonstrated by previous biomechanical studies [9,25,26]. In the meantime, early (within a few days of injury, if possible) mobilization of this group of patients is recommended, as it will significantly avoid the complications of prolonged bedrest [27].

Figure 4. (Left): Adapted from Alberta Association of Orthotists and Prosthetists. (Right): Adapted from the Steeper Group—Oasis Spinal Brace.
As mentioned above, the posterior spinal muscles are an important part of the human posterior tension band, which maintains the truncal posture. Thus, strengthening the posterior spinal muscles will improve lumbar lordosis and posture and will reduce acute fracture pain as well as chronic back pain associated with kyphotic deformity from progressive vertebral body collapse [18,28]. This reinforcement is especially important since axial musculature decreases in strength with age, particularly among women, who are most at risk for OSF [29]. Studies have also demonstrated that back extension strength and lumbar mobility are the most important factors for quality of life compared to other relevant factors such as lumbar kyphosis angle and bone mineral density, especially in females with osteoporosis [30].
2.1. Limitations with Traditional Spine Braces in OSF
While rigid spinal braces are widely prescribed in the conservative, non-surgical management of OSF, there is a lack of high-quality evidence for their effectiveness. Traditional rigid spine braces aim to restore the normal curvature of the spine by applying a set of displacements at different levels of the torso, which are typically achieved by adjusting the geometry of the brace or adding soft pads inside the brace. This process relies mostly on bi-planar radiographs of the spine taken in the sagittal and coronal planes, surface topography of the torso, and the experience of the orthotist who has limited quantitative data.
A recent meta-analysis looking at the effect of a brace on OSF concluded that a Spino-med orthosis, which work with a concept of improving the strength of users’ trunk muscle, unlike traditional rigid braces which offer immobilization of the spine, may subsequently reduce pain, reduce kyphosis angle deterioration, and improve quality of life [16]. However, due to the high risk of bias in the blinding process and outcome assessment in the included studies, only low-quality evidence proved using Spino-med braces could bring large and significant beneficial effect to patients with subacute osteoporotic vertebral fractures [18]. Spinal braces are part of the conservative, non-surgical care regime for conservatively managed OSF and have been compared to external support provided by a variety of orthoses or casting. As a result, it is not possible to properly quantify a comparison between the designs, and it makes the true treatment effect of an orthosis difficult to elucidate. There are also wide variations in terms of outcome measurements and the duration of brace application in different studies. Currently, there is no study which evaluates the long-term outcomes of the traditional rigid spinal brace application.
Although spinal braces for OSF are known to improve trunk muscle strength, posture, and body height, all which will improve quality of life and ability to perform activities of daily living (ADL) for patients with OSF [30], these rigid spinal braces have a number of limitations due to their rigid, static, and sensorless features. The rigidity of the brace makes it difficult to wear over extended periods of time, and it interferes with ADLs. User compliance will subsequently become a main issue. The braces statically hold the torso in a set posture without detection of the forces/moments exerted on the torso. These excessive forces are known to cause skin breakdown, pressure sores, and even worsening of spinal deformities [31,32]. The lack of freedom of control of the correction provided by the brace at the coronal and sagittal planes makes it difficult to adapt to natural changes of the spine and may impair healing and lead to diminished effectiveness. Non-static braces have been designed to address some of these limitations. However, non-static braces are only useful for temporary relief of symptoms. As they do not provide spinal support, their function in preventing progressive kyphosis, for example in patients post-OSF and especially at the junctional thoracolumbar levels, is known to not be effective [16].
A systemic review of spinal braces in OSF showed no evidence to support the regular use of rigid TLSO [33]. Potential downfalls of a rigid spinal brace such as TLSO are well documented in literature. As mentioned above, these include patient discomfort, which may decrease compliance. There are also risks for skin breakdown if the brace edges are not carefully padded. In addition, a brace that is too restrictive may impede the patient’s respiratory volume and effort and may eventually lead to chest infections. With prolonged periods of bracing, there is also a high chance for deconditioning and atrophy of the trunk and erector spinae muscles, which in turn will lead to increased risk of future falls and further injuries and/or fractures [16,21,29,33,34].
A semi-rigid backpack or bell-style thoracolumbar orthosis (TLO) could reduce pain and improve participation in activities of daily life [24]. A weighted orthosis seems to improve balance, while there is little to no current evidence to suggest that bracing will negatively affect wedging and kyphotic progression of the spine in OSF [17,33].
Reference (Editors will rearrange the references after the entry is submitted)
- United Nations Population Division. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2017_Highlights.pdf (accessed on 10 January 2021).
- International Osteoporosis Federation Data and Publications: Facts and Statistics. Available online: https://www.osteoporosis.foundation/facts-statistics (accessed on 10 January 2021).
- Kim, H.-J.; Yi, J.-M.; Cho, H.-G.; Chang, B.-S.; Lee, C.-K.; Kim, J.H.; Yeom, J.S. Comparative Study of the Treatment Outcomes of Osteoporotic Compression Fractures without Neurologic Injury Using a Rigid Brace, a Soft Brace, and no Brace: A Prospective Randomized Controlled Non-inferiority Trial. J. Bone Jt. Surg. Am. Vol. 2014, 96, 1959–1966.
- Oleksik, A.M.; Ewing, S.; Shen, W.; Van Schoor, N.M.; Lips, P. Impact of Incident Vertebral Fractures on Health-related Quality of Life (HRQOL) in Postmenopausal Women with Prevalent Vertebral Fractures. Osteoporos. Int. 2005, 16, 861–870.
- Choi, H.; Seo, K.; Hyung, S.; Shim, Y.; Lim, S.-C. Compact Hip-Force Sensor for a Gait-Assistance Exoskeleton System. Sensors 2018, 18, 566.
- Christophy, M.; Senan, N.A.F.; Lotz, J.C.; O’Reilly, O.M. A Musculoskeletal Model for the Lumbar Spine. Biomech. Modeling Mechanobiol. 2012, 11, 19–34.
- Adams, M.A. The Biomechanics of Back Pain. Acupunct. Med. 2004, 22, 178–188.
- Sinaki, M.; Nwaogwugwu, N.C.; Phillips, B.E.; Mokri, M.P. Effect of Gender, Age, and Anthropometry on Axial and Appendicular Muscle Strength. Am. J. Phys. Med. Rehabil. 2001, 80, 330–338.
- Miyakoshi, N.; Hongo, M.; Maekawa, S.; Ishikawa, Y.; Shimada, Y.; Itoi, E. Back Extensor Strength and Lumbar Spinal Mobility are Predictors of Quality of Life in Patients with Postmenopausal Osteoporosis. Osteoporos. Int. 2007, 18, 1397–1403.
- Cafolla, D.; Marco, C. Design and Simulation of Humanoid Spine. Mech. Mach. Sci. 2014, 24, 585–593.
- Kim, H.K.; Zhang, Y. Estimation of Lumbar Spinal Loading and Trunk Muscle Forces during Asymmetric Lifting Tasks: Application of Whole-body Musculoskeletal Modelling in OpenSim. Ergonomics 2017, 60, 563–576.
- Shirazi-Adl, A.; Ahmed, A.M.; Shrivastava, S.C. Mechanical Response of a Lumbar Motion Segment in Axial Torque Alone and Combined with Compression. Spine 1986, 11, 914–927.
- Schultz, A.B.; Haderspeck-Grib, K.; Sinkora, G.; Warwick, D.N. Quantitative Studies of the Flexion-relaxation Phenomenon in the Back Muscles. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 1985, 3, 189–197.
- Blattert, T.R.; Schnake, K.J.; Gonschorek, O.; Gercek, E.; Hartmann, F.; Katscher, S.; Mörk, S.; Morrison, R.; Müller, M.; Partenheimer, A.; et al. Nonsurgical and Surgical Management of Osteoporotic Vertebral Body Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Glob. Spine J. 2018, 8, 50S–55S.
- Lyles, K.W. Management of Patients with Vertebral Compression Fractures. Pharmacotherapy 1999, 19, 21S–24S.
- Jin, Y.Z.; Lee, J.H. Effect of Brace to Osteoporotic Vertebral Fracture: A Meta-Analysis. J. Korean Med. Sci. 2016, 31, 1641–1649.
- Pfeifer, M.; Begerow, B.; Minne, H.W. Effects of a New Spinal Orthosis on Posture, Trunk Strength, and Quality of Life in Women with Postmenopausal Osteoporosis. A Randomized Trial. Am. J. Phys. Med. Rehabil. 2004, 83, 177–186.
- Li, M.; Law, S.-W.; Cheng, J.; Kee, H.-M.; Wong, M.S. Comparison Study on the Efficacy of SpinoMed® and Soft Lumbar Orthosis for Osteoporotic Vertebral Fracture. Prosthet. Orthot. Int. 2015, 39, 270–276.
- The Effect of Posture Support Corset on Balance, Quality of Life, Dorsal Kyphosis in Patients with Kyphosis due to Osteoporosis. Available online: https://www.researchgate.net/publication/288156692_The_effect_of_posture_support_corset_on_balance_quality_of_life_dorsal_kyphosis_in_patients_with_kyphosis_due_to_osteoporosis (accessed on 10 January 2021).
- Chang, V.; Holly, L.H. Bracing for Thoracolumbar Fractures. Neurosurg. Focus 2014, 37.
- Alcalá-Cerra, G.; Díaz-Becerra, C.; Fernandes-Joaquim, A.; Moscote-Salazar, L.R.; Paternina-Caicedo, A.J. Orthosis for Thoracolumbar Burst Fractures without Neurologic Deficit: A Systematic Review of Prospective Randomized Controlled Trials. J. Craniovertebral Junction Spine 2014, 5, 25–32.
- Prather, H.; Watson, J.O.; Gilula, L.A. Nonoperative Management of Osteoporotic Vertebral Compression Fractures. Injury 2007, 38 (Suppl. S3), 40–48.
- Slavici, A.; Rauschmann, M.; Fleege, C. Conservative Management of Osteoporotic Vertebral Fractures: An Update. Eur. J. Trauma Emerg. Surg. 2016, 43, 19–26.
- Agabegi, S.S.; Asghar, F.A.; Herkowitz, H.N. Spinal Orthoses. J. Am. Acad. Orthop. Surg. 2010, 18, 657–667.
- Lantz, S.A.; Schultz, A.B. Lumbar Spine Orthosis Wearing. I. Restriction of Gross Body Motions. Spine 1986, 11, 834–837.
- Longo, U.G.; Loppini, M.; Denaro, L.; Maffulli, N.; Denaro, V. Osteoporotic Vertebral Fractures: Current Concepts of Conservative Care. Br. Med Bull. 2012, 102, 171–189.
- Esses, S.I.; McGuire, R.; Jenkins, J.; Finkelstein, J.; Woodard, E.; Watters, W.C.; Goldberg, M.J.; Keith, M.; Turkelson, C.M.; Wies, J.L.; et al. The Treatment of Symptomatic Osteoporotic Spinal Compression Fractures. J. Am. Acad. Orthop. Surg. 2011, 19, 176–182.
- Möller, A.; Hasserius, R.; Redlund-Johnell, I.; Ohlin, A.; Karlsson, M.K. Nonoperatively Treated Burst Fractures of the Thoracic and Lumbar Spine in Adults: A 23- to 41-year follow-up. Spine 2007, 7, 701–707.
- Valentin, G.H.; Pedersen, L.N.; Maribo, T. Wearing an Active Spinal Orthosis Improves Back Extensor Strength in Women with Osteoporotic Vertebral Fractures. Prosthet. Orthot. Int. 2014, 38, 232–238.
- Sinaki, M.; Itoi, E.; Wahner, H.; Wollan, P.; Gelzcer, R.; Mullan, B.; Collins, D.; Hodgson, S. Stronger Back Muscles Reduce the Incidence of Vertebral Fractures: A Prospective 10 year Follow-up of Postmenopausal Women. Bone 2002, 30, 836–841.
- Dionyssiotis, Y.; Trovas, G.; Thoma, S.; Lyritis, G.; Papaioannou, N. Prospective Study of Spinal Orthoses in Women. Prosthet. Orthot. Int. 2015, 39, 487–495.
- Newman, M.; Lowe, C.M.; Barker, K.L. Spinal Orthoses for Vertebral Osteoporosis and Osteoporotic Vertebral Fracture: A Systematic Review. Arch. Phys. Med. Rehabil. 2016, 97, 1013–1025.
- Rzewuska, M.; Ferreira, M.; McLachlan, A.J.; Machado, G.C.; Maher, C.G. The Efficacy of Conservative Treatment of Osteoporotic Compression Fractures on Acute Pain Relief: A Systematic Review with Meta-analysis. Eur. Spine J. 2015, 24, 702–714.
- Influence of Spinal Orthosis on Gait and Physical Functioning in Women with Postmenopausal Osteoporosis. Available online: https://www.researchgate.net/publication/51851552_Influence_of_spinal_orthosis_on_gait_and_physical_functioning_in_women_with_postmenopausal_osteoporosis (accessed on 10 January 2021).
This entry is adapted from the peer-reviewed paper 10.3390/healthcare9010070
