The difficulty of Chronic kidney disease (CKD) management lies in how it is a comorbid and progressive disease. A pure biomedical approach is inadequate. It is recommended that an integrated Patient-Centered Self-Management (PCSM) approach with health literacy and information technology intervention, which unifies and integrates patient education, can address the difficulties that are contributing to unsuccessful treatment outcomes. An integrated PCSM model should be implemented systematically and methodologically into future CKD management and health policies.
- chronic kidney disease
- empowerment
- health-literacy
- integrated care
- patient-centered
- self-management
- self-regulation
1. Introduction
Chronic kidney disease (CKD) is a worldwide health problem. According to the 2017 Global Burden of Disease Study, CKD ranked 12th in the list of causes of deaths worldwide, affecting 13.4% of the global population [1]. Moreover, all-age prevalence of CKD has increased by 29.3% since 1990 [1,2]. Taiwan has the highest prevalence and incidence of CKD in the world [3]. The prevalence of CKD is increasing as people are living longer lives while the global population continues to rise. Longevity exists side by side with population aging and chronic elderly illnesses, which are major concerns for governments worldwide, as they pose hefty social and financial burdens to the individual, society, and health systems [4,5]. Symptoms of CKD are inapparent at the early stages of the disease [6], which usually allows for it to progress rapidly to end-stage renal disease (ESRD). Living with ESRD can be burdensome, particular when the demand for dialysis treatment increases, causing overwhelming financial and mental liabilities for individuals, their families, and health systems [7]. Lifestyle changes and early interventions are central to preventing disease or deferring progression of disease. Such is the case for CKD, which can abruptly deteriorate if the patient’s lifestyle changes do not follow a strict regimen. Thus, precautionary prevention becomes a health care priority. Treatment of CKD is focused on the prevention of disease progression towards ESRD, and one of the key factors of prevention is self-management (SM).
The concept of SM is central to many chronic conditions, as it is the gold standard of chronic care, and CKD is a classic example. Patients with chronic diseases usually have to live their entire lives with their disease. Thus, the treatment goal lies in improving their quality of life through SM. Chronic disease SM refers to an individual’s ability to handle the various aspects of living with a chronic condition [8,9], as well as “the everyday tasks an individual must undertake to control or reduce the impact of disease on physical health status [10,11].” Risk factors that predispose an individual to CKD can directly contribute to its severity and progression, but are modifiable through early detection and prevention through SM. These risk factors are usually lifestyle factors, primarily determined by the individual’s behavior and often shape the outcome of treatment. The impact of patients’ behavioral choices places patient-centered self-management (PCSM) at the core of chronic care and prevention models.
Patient-centered care (PCC) is a fundamental approach for improving the quality of health care and a promising paradigm where the patients’ values, goals, needs, and preferences are taken into consideration in the process of decision-making and delivery of health care [12]. A pure biomedical approach to chronic disease management does not adequately assess the health status of patients, and biomedical characteristics and biomarkers are often inadequate for predicting the patient’s actual wellbeing. Multiple facets of individuals and their environment must be considered in the treatment of disease, which denotes that a PC approach is vital in attaining effective SM in CKD treatment. Considering patient experience and standpoint can improve the accuracy of assessment and prediction in the treatment of disease. This gave rise to health frameworks with a focus on PCC (the PCC paradigm), which offers a much more comprehensive and all-rounded approach to understanding the patients’ overall wellbeing. I
2. Patient-Centered Self-Management in Patients with Chronic Kidney Disease
2.1. Recommendations for Future Direction
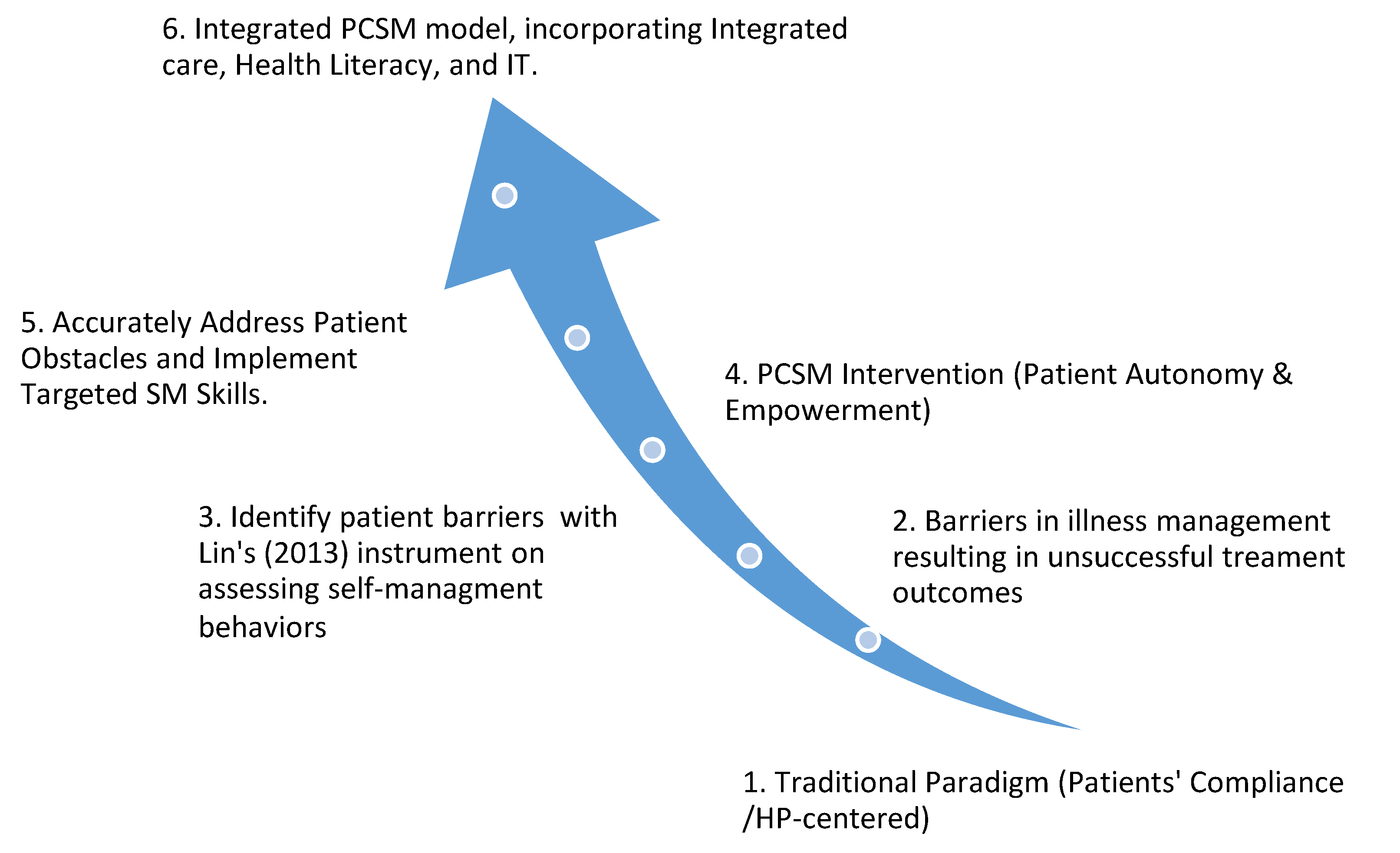
We described important attributes of PCSM and its implementation on obstacles in CKD treatment and concluded that achieving success in treatment of CKD requires an integrated PCSM approach along with health literacy and information technology (IT) intervention, which unifies and integrates patient education. Synthesis of inclusion studies indicate that a pure biomedical approach to chronic disease management is inadequate, and that PCC is vital in attaining effective management. A focus on integrated PCC, health literacy, and IT can address the difficulties in SM interventions that may improve CKD treatment outcomes. A sequenced summary of integrated PCC, health literacy, and IT is as follows:
2.1.1. Health Literacy
Patient’s knowledge and awareness of SM skills determine the effectiveness of treatment and is important in impeding advancement of CKD [54]. For patients to be effective at SM, they must possess the ability to utilize health information, a skill referred to as health literacy. Campbell et al. [59] indicated that low health literacy is associated with an increase in mortality and poorer overall health status of patients with CKD. While Grubbs et al. [60] stated that limited health literacy is associated with decreased access to transplantation, poor blood pressure control, and poor SM skills. Health literacy can impact a patient’s awareness and understanding of the importance of active participation in management of their illness. Put simply, health literacy can play a significant role in reducing the complications of CKD and preventing its progression [61].
Improving health literacy is the foundation for successful SM intervention [62], and health literacy can be developed through patient education [59]. Educational or therapeutic interventions used to promote patients’ level of health literacy are not only intended to reduce complications, but also to promote SM behaviors [59], and further improve patients’ quality of life [63]. Young [64] advises nephrologists to improve on their knowledge of the adverse effects of health literacy on patient health, and Campbell et al. [59] suggests fostering health literacy in patient education and implementing it into diverse SM interventions [54]. In an era of information explosion today, patients tend to utilize diverse resources from health professionals, family or friends, educational courses, or the Internet. Educating, detecting, and critically appraising health information of patients with CKD are some of the challenges faced in health literacy [65].
2.1.2. Information Technology
IT is widely adopted in SM interventions nowadays to aid patients with CKD [66]. IT refers to mobile applications (apps), personal digital assistants (PDAs), wearable devices, computer systems, etc. IT is constructive in promoting education, empowerment, collaboration, and communication in SM [23,67], and offers HPs and patients a convenient and easily accessible platform where knowledge can be shared, and ideas can be exchanged. Specifically, apps helped patients in understanding specific biomarkers and self-monitoring of disease progression [68]. Web-based SM applications can be used to educate patients about CKD, monitor their progress, engage them to set goals, and provide an interactive tool for collaborating with clinicians in general [69,70]. IT interventions that target health behaviors, personal feedback mechanism, and collaborative platform between patients and HPs can lead to improved patient empowerment [61,70].
However, challenges were also identified in Ong et al. [69]’s study with a web-based SM application, called My Kidney Care Kiosk. Patients felt that the Kiosk application improved healthcare quality and strengthened interaction with HPs, but there were areas that needed improvements, such as a lack of integration of the application with the hospital electronic medical record system and high dependency on healthcare staff to promote the use of app. The change in staff workflow created increased workload and increased patient waiting time. Choi and Lee [6] cautions that direct, in-person interactions with HPs should not be replaced entirely by IT. Individualized consultations should be employed collectively with IT to address patient’s conditional needs.
2.1.3. Integrated Patient-Centered Care
Integrated care is termed “a coherent set of methods and models designed to create connectivity, alignment, and collaboration within and between patients and health systems” [71]. Integrated care seeks to systematize and standardize a uniform and well-coordinated care system, in contrast to sporadic care, which contributes to unsuccessful treatment outcomes [72]. The goal of these methods and models is to enhance efficiency and reduce gaps in treatment of illnesses. It is the process by which professionals, resources, health sectors come together to form a comprehensive delivery of quality health care [71].
Patients with CKD often experience co-morbidity accompanying multiple interrelated illnesses (such as diabetes, cardiovascular disease, hypertension, obesity [52]). When these diseases are treated individually, it often leads to confusion and misperceptions, which builds on unnecessary costs and produces additional waste of medical resources. There is a need for further primary research on the effect of PC integrated care on patients with CKD that follows a uniform standard of data collection. The challenge is to develop a uniform and universal PC integrated care model that incorporates the interrelated co-morbidity factors that underlie the burden of CKD [72,73,74].
The lack of an organized and uniform method of data collection specifically focused on PC integrated CKD care management resulted in a marked lack of high-quality evidence available for literature reviews [74]. There was a lack of data available for organization-level care integration, methodologic limitations that reduced the confidence of data, a lack of long-term studies with follow-up beyond 12 months, and a lack of significant statistical values due to small sample sizes and low-quality data [72]. Future research direction should focus on establishing conceptual clarity and consolidate practical know-how with long-term follow-ups in the design and implementation of integrated care models.
2.2. Implications
The difficulty of CKD management lies in that it is a comorbid and progressive disease, which can abruptly worsen without adequate lifestyle modification, early intervention, and long-term adherence. Thus, SM programs for patients with CKD require an emphasis on PC integrated care, which requires active participation and a positive change in patients’ attitudes [18], while HPs offer personalized patient education support aimed at improving patients’ self-regulation abilities [6]. Altogether, this review proposes that an integrated PCSM model with health literacy and IT intervention, which unifies and integrates patient education, can address the difficulties that are contributing to unsuccessful patient treatment outcomes. Achieving success in treatment of patients with CKD requires a shift from compliance paradigm to a PCSM approach, which comprises concepts like empowerment and self-regulation, along with health policies that incorporate systematic integrated care, while health literacy and IT intervention consolidate patient education. Figure 1 summarizes the main idea of this literature review and clarifies the process of evolving a more effective and wholesome integrated PCSM paradigm from the traditional paradigm, where patient compliance is the main focus.
This entry is adapted from the peer-reviewed paper 10.3390/ijerph17249443
