Healthy aging makes the practice of physical activity (PA) a necessity. However, PA guidelines achievement in older adults is scarce. The use of behavioral theories such as Transtheoretical Model (TTM), helps in older adults PA promotion. The aim of this review was to identify the use of TTM for PA in older adults (>60 years). PubMed, SPORTdiscus, and Medline databases were used to conduct the search. All steps of the process followed the recommendations of the PRISMA flow-diagram. We identified eight studies: Six were descriptive cross-sectional studies, one prospective-cohort study and one with a quasi-experimental design. Only two papers evaluated the four behavior change dimensions within the same study, three evaluated the processes of change and the decisional balance, four evaluated the exercise self-efficacy and all assessed the stages of change for PA behavior.
Thanks so much for your check. We sincerely hope you may create this entry, since you are the expert in this academic research. All the contents is the draft we prepared for you. You can click the “submit” icon to upload and revise it. And the entry will be online only after authors edit and submit it. We will help you layout. Moreover, we will link your article at the entry, and more scholars and students can benefit from it. (You can remove this note when submitting.)
(Draft for you)
1. Introduction
Physical activity (PA) is considered as one of the most effective strategies to promote healthy aging [
1]. Regular PA practice in older adults is associated with improvements in functional fitness (maintains muscle strength and balance), chronic diseases risk prevention (coronary heart disease, diabetes, and stroke), improvement of mental capacity (self-esteem, maintenance of the cognitive function, reduce anxiety, and depression), and improvement in social response [
2,
3,
4,
5,
6,
7]. PA is a good predictor of healthy aging and decreases the probability of disability in people over 65 years [
8].
Recommendations for adults and older adults state the need to achieve at least 150 min of PA at moderate intensity per week, together with muscle strength activities for an improvement in bone mass and activities to improve flexibility, at least 2–3 days per week [
9].
However, despite the important health benefits of PA, a little proportion of the population over 65 years meet World Health Organization (WHO) PA guidelines [
10]. In fact, this group is the least physically active out of all [
11]. According to WHO [
12], having a sedentary lifestyle is the fourth primary risk factor of non-communicable diseases. The good news are that those who practice regular PA can reduce their risk of pathologies at a rate between 20 and 30% [
1].
Older adults’ exercise adherence is a multifactorial process, influenced by: Program characteristics (preference of exercise type), personal factors (demographic, health related, physical, and psychological factors) [
13,
14], social determinants, and environmental factors [
15]. It is important that interventions to promote physical exercise in older adults are based on theories that explain the behavior change, tailored to individual characteristics of the participants [
15]. Theory-based interventions to promote PA behavior seem to have a more successful effect than interventions without an established theoretical base [
16,
17]. In addition, interventions based on a single theory reported greater impact on PA behavior than those interventions with a combination of theories [
17].
One of the models that better understands and predicts the behavioral–cognitive changes in the adoption of PA/exercise behavior, is the Transtheoretical Model of Change (TTM), proposed by Prochaska and Di Clemente [
18]. The TTM is a most comprehensive and integrated model of behavioral changes among health behavioral models [
19], this model began to be used in smoking cessation studies [
18], but over time its use has extended to the study of healthy lifestyle promotion, including PA, to become one of the most popular models to understand the PA behavior [
20]. This model is a cyclical model and explains the behavior change as a dynamic process, through a temporal dimension by describing them as a sequence of stages and processes by which the individual progress to adapt a regular behavior [
21].
2.Related Studies
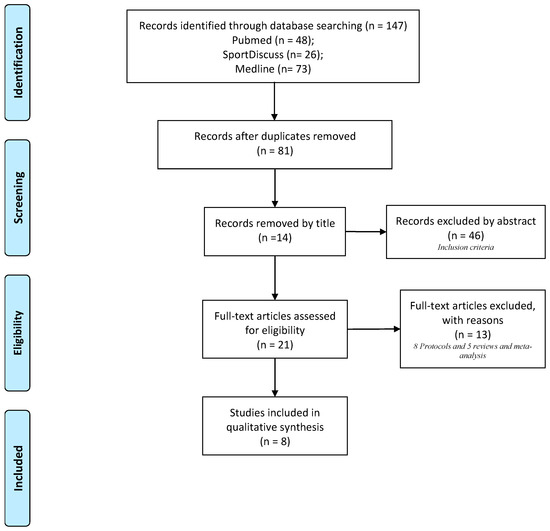
details all the steps of the processes followed according to the recommendations of the PRISMA flowchart in the studies selection. We identified a total of eight studies published between 2014 and 2019 which were included in the systematic review from the original 147 papers identified by the literature search [
37,
38,
39,
40,
41,
42,
43,
44]. The most common reason for excluding studies was that they did not meet the inclusion criteria, mainly by the age.
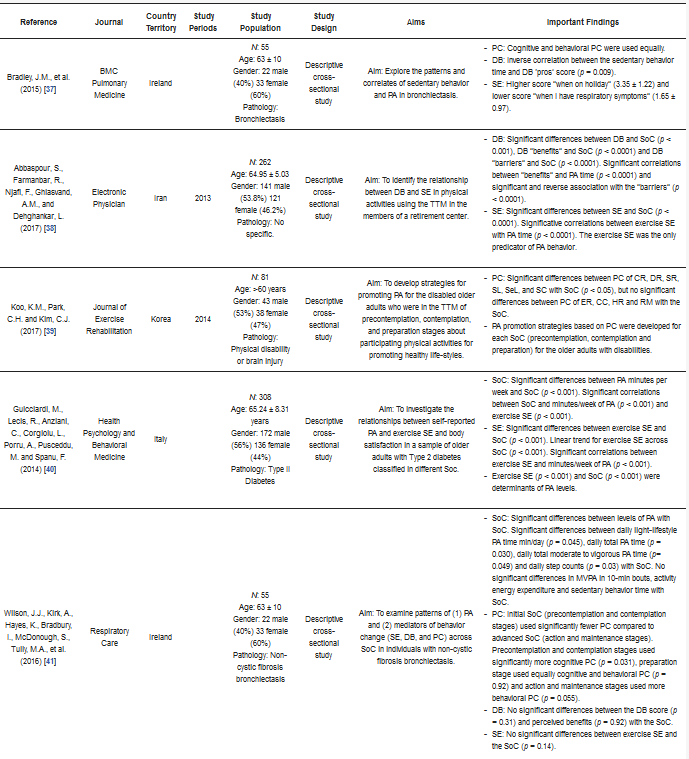
The main characteristics, TTM dimensions, outcomes, and key findings for each of the 8 articles included in this review are listed in and . Of these eight articles, six studies were descriptive-cross-sectional studies [
37,
38,
39,
40,
41,
44], one was a prospective cohort study [
42] and one was a quasi-experimental design [
43]. Two of the studies originated from Ireland [
37,
41], two more from Taiwan [
42,
43] and individual studies from Iran [
38], Korea [
39], Japan [
44], and Italy [
40]. According to the study population, the review gather a total of 2304 participants, included both men (51.65%) and women (48.35%). Only three of the studies (37.5%) worked with healthy older adults [
38,
43,
44] and the rest with pathologies (62.5%) (bronchiectasis [
37], non-cystic fibrosis bronchiectasis [
41], physical disability or brain injury [
39], type II diabetes [
40], and patients after open heart surgery [
42]). Regarding to TTM-interventions characteristics, we can find the following topics: Measuring PA levels [
40,
42], to identified daily patterns of PA [
41], to understand the levels of PA and sedentarism [
37], to identify knowledge of muscle strength exercise recommendations [
44] to create PA-interventions tailored to specific SoC [
39,
43] and to corroborate the usefulness of this model in older adults [
38].
Figure 1. PRISMA flow-chart.
Table 3. TTM in older adults.
In the following sections, we “drill down” in the different constructs of TTM to examine what has been found regarding the influence TTM on PA.
2.1. Stages of Change (SoC)
The SoC have been considered as predictors of PA [
40]. Significant differences (
p < 0.05) were found between the minutes of PA/week [
40,
41,
42], daily total PA time, daily light-lifestyle PA time, daily total moderate to vigorous physical activity (MVPA) time and daily steps counts [
41] according to the different SoC. The average of bouts (10-min) MVPA and activity energy expenditure increased and the sedentary behavior time decreased regarding to SoC but not significantly [
41]. Moreover, there was an increase in PA levels and a decrease of sedentary behavior time as we moved through to more advanced SoC (action and maintenance stages) [
40,
41,
42]. Finally, advanced stages of behavior change corresponded to greater benefits and lower perceived barriers referred to the achievement of muscle strength exercise recommendations [
44].
2.2. Processes of Change (PC)
The PC are the techniques and strategies that people use to change or modify their behavior. PC were clearly identified in patients with bronchiectasis, showing a likewise use of cognitive and behavioral processes in their PA behavior [
37]. In patients with non-cystic fibrosis bronchiectasis, it was observed as initial SoC (precontemplation and contemplation stages) used significantly fewer PC compared to more advanced SoC (action and maintenance stages) (
p > 0.01), on the other hand, precontemplation and contemplation stages tended to use cognitive PC (
p = 0.031), preparation stage used behavioral and cognitive PC equally (
p = 0.92) and action and maintenance stages tended to use of behavioral PC (
p = 0.055) [
41]. In patients with physical disability or brain injury, no significant differences were found among PC of ER, CC, HR, and RM across the SoC (
p > 0.05), while, the patterns of use PC of CR, DR, SR, SL, SeL, and SC varied significantly across precontemplation, contemplation, and preparation stages (
p < 0.05) [
39]. Finally, the use of PC to create and tailor interventions with the aim of promoting PA in the older adults, favored the progression of participants to more proactive SoC (action and maintenance) and therefore improved the acquisition of healthy habits [
43].
2.3. Decisional Balance (DB)
There were a significant differences (
p < 0.001) between the DB score among the different SoC [
38]. The DB can be divided in two dimensions: Benefits and barriers. According to benefits, there was a direct association (
p < 0.001) between perceived benefits and PA levels [
38] and an inverse association (
p = 0.009) with sedentary time [
37]. Significant differences were observed between SoC and perceived benefits (
p < 0.001) [
38]. Regarding the barriers, we observed an inverse correlation (
p < 0.001) between perceived barriers and levels of PA, in addition, there were significant differences between SoC and perceived barriers (
p < 0.001) [
38]. In patients with bronchiectasis [
41] there were no significant differences between the DB score (
p = 0.31) and the benefits perceived (
p = 0.92) with the SoC.
2.4. Self-Efficacy (SE)
The SE refers to people’s confidence in their ability to make a change in specific situations. Two of the articles considered SE as predictor of PA [
38,
40]. Significant differences were found between the SE score and the SoC (
p < 0.01) [
38,
40]. In addition, a direct association between SE and PA levels was observed (
p < 0.01) [
38,
40]. Advanced SoC (action and maintenance stages) had higher SE scores [
38] with a linear trend (
p < 0.001) in the result [
40]. On the other hand, studies with older adults with respiratory pathologies did not find any significant differences (
p = 0.14) between SE score and SoC [
41] and they reported that their SE was reduced when they experienced situations related to symptoms of their disease [
37].
This entry is adapted from the peer-reviewed paper 10.3390/ijerph17249262