While schizophrenia is traditionally managed through pharmacological treatment, many patients continue to experience persistent symptoms, cognitive impairment, and reduced quality of life. Meditation—particularly mindfulness-based interventions—has emerged as a promising complementary strategy that targets emotional regulation, stress response, and attentional control through neuroplastic mechanisms. Drawing on quantitative findings from a 12-week intervention, the entry highlights significant reductions in symptom severity, including both positive and negative symptoms, alongside improvements in working memory, executive functioning, and psychological well-being. Qualitative insights from patients and healthcare providers further illustrate increased self-awareness, reduced hallucination distress, stronger coping skills, and improved emotional stability. By synthesizing clinical outcomes with neuroscience perspectives, this entry underscores meditation’s potential to bridge biological, psychological, and social dimensions of schizophrenia care. It positions meditation as an accessible, patient-centered, and culturally adaptable tool that can enhance traditional treatment models and support holistic recovery.
- Schizophrenia
- Meditation
- Mindfulness-Based Interventions
- Neuroplasticity
- Symptom Reduction
- Cognitive Enhancement
- Psychosocial Recovery
1. Introduction
Schizophrenia is a chronic psychiatric disorder characterized by hallucinations, delusions, cognitive impairments, and emotional dysregulation[1]. Although antipsychotic medication forms the basis of treatment, these drugs frequently fail to address negative symptoms and cognitive deficits[2]. Meditation has gained scientific interest as a complementary therapy capable of improving emotion regulation and cognitive functioning through changes in neural networks such as prefrontal–amygdala pathways[3][4]. Mindfulness practices have been shown to reduce stress, enhance cognitive flexibility, improve working memory[5], and increase emotional resilience[6]. These mechanisms make meditation suitable as a holistic adjunctive tool within schizophrenia care.[7]
2. Study Overview
The study used a 12-week mindfulness-based intervention (MBI) with:
- 10 patients diagnosed with schizophrenia,
- 10 healthcare providers,
- A mixed-methods design combining standardized quantitative measurements and qualitative interviews.
Quantitative data were drawn from PANSS, Digit Span Tests[5] , Trail Making Tests[8], and the WHO-QOL-BREF[9].
The dataset is documented in the Harvard Dataverse[7].
3. Quantitative Results
3.1. Symptom Reduction (PANSS)
The intervention produced significant clinical improvements across all PANSS domains[7]:
|
Symptom Domain |
Baseline |
Post-Intervention |
p-value |
Effect Size (d) |
|---|---|---|---|---|
|
Positive Symptoms |
22.4 ± 3.1 |
18.2 ± 2.8 |
<0.05 |
0.8 |
|
Negative Symptoms |
24.6 ± 4.0 |
21.3 ± 3.5 |
<0.01 |
0.7 |
|
General Psychopathology |
30.1 ± 5.2 |
26.7 ± 4.9 |
<0.01 |
0.9 |
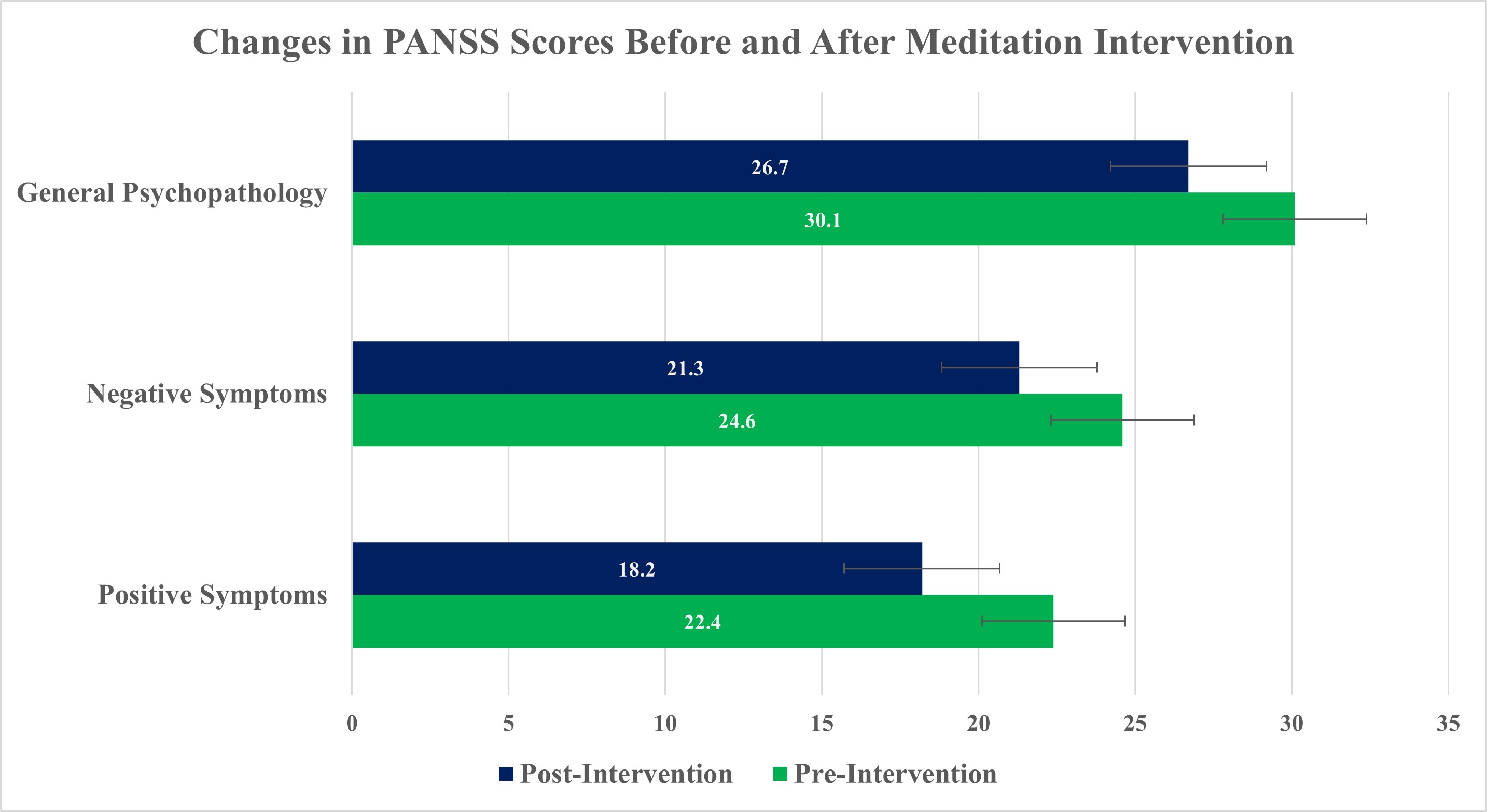
These reductions align with research showing that meditation enhances neural regulation and executive control in psychiatric disorders[6][10].
3.2. Cognitive Improvements
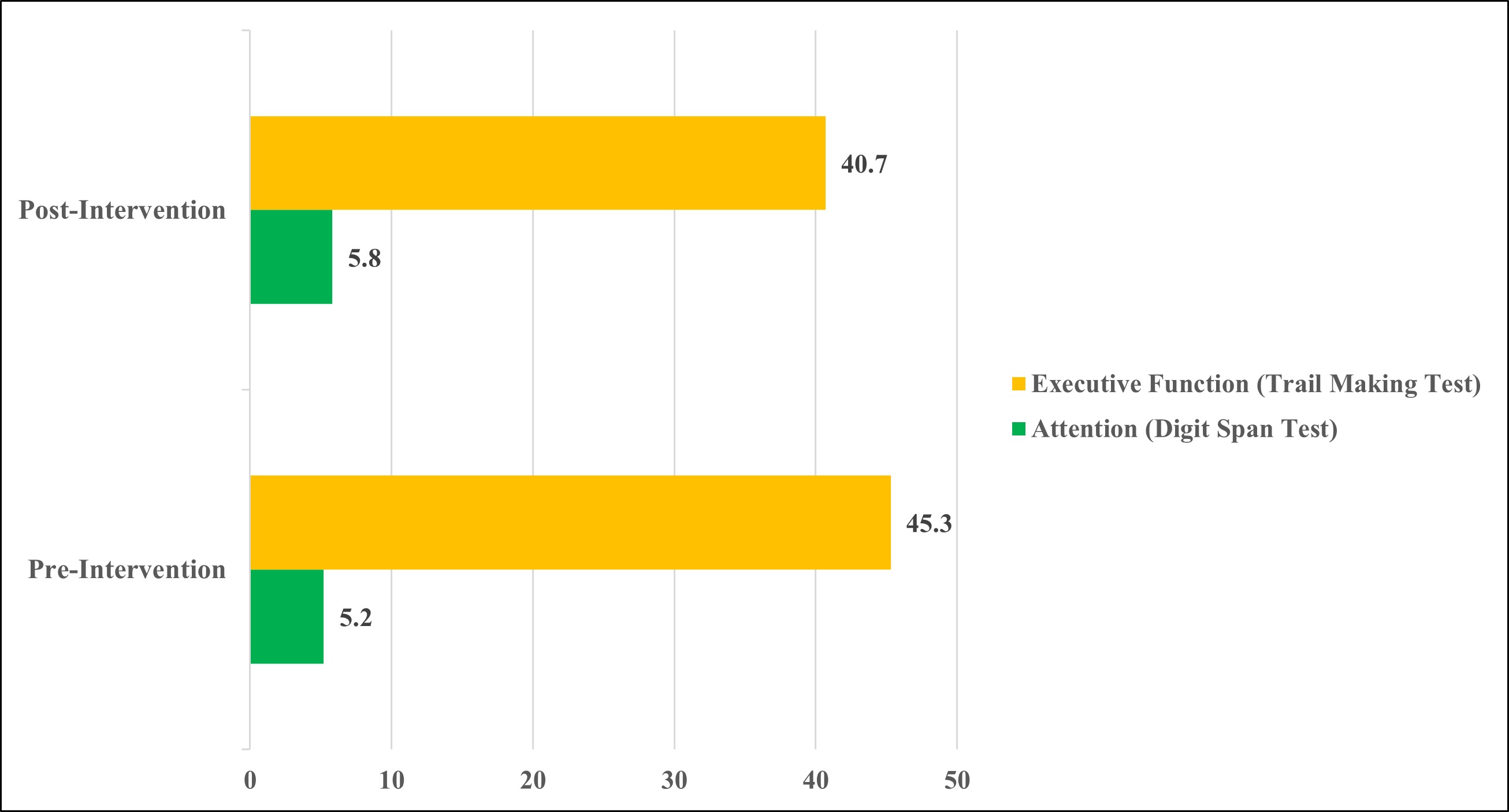
Cognitive performance increased meaningfully:
- Digit Span (Attention): ↑ 12% (p < 0.05)[5]
- Trail Making Test (Executive Function): ↑ 10% (p < 0.05)[8]
Meditation is known to enhance working memory capacity and attentional control[11].
Table 1. Changes in Symptom Severity, Cognitive Performance, and Quality of Life.
|
Measure |
Pre-Intervention (Mean ± SD) |
Post-Intervention (Mean ± SD) |
p-value |
Effect Size (Cohen’s d) |
|---|---|---|---|---|
|
PANSS – Positive Symptoms |
22.4 ± 3.1 |
18.2 ± 2.8 |
< 0.05 |
0.8 |
|
PANSS – Negative Symptoms |
24.6 ± 4.0 |
21.3 ± 3.5 |
< 0.01 |
0.7 |
|
PANSS – General Psychopathology |
30.1 ± 5.2 |
26.7 ± 4.9 |
< 0.01 |
0.9 |
|
Digit Span Test (Attention) |
5.2 ± 1.1 |
5.8 ± 1.0 |
< 0.05 |
0.6 |
|
Trail Making Test (Executive Function) |
45.3 ± 8.2 |
40.7 ± 7.5 |
< 0.05 |
0.6 |
|
WHO-QOL-BREF – Psychological Well-being |
60.5 ± 10.2 |
69.6 ± 9.8 |
< 0.05 |
0.9 |
|
WHO-QOL-BREF – Social Relationships |
55.3 ± 12.4 |
66.4 ± 11.2 |
< 0.01 |
0.9 |
3.3. Quality of Life Improvements
Quality-of-life scores improved significantly[7]:
Mindfulness-based therapies are associated with better social functioning and emotional well-being[12].
4. Qualitative Results
Six themes emerged from patient and provider interviews:
- Enhanced Self-Awareness and Insight
Patients developed clearer understanding of their thoughts and emotions, consistent with mindfulness mechanisms[10]. - Reduced Distress from Hallucinations
Many participants described quieter or less intrusive auditory hallucinations, aligning with evidence that meditation reduces symptom distress[12]. - Cultural Sensitivity
Tailoring meditation to cultural practices improved engagement, reflecting findings in cross-cultural mindfulness research[13]. - Improved Coping Strategies
Patients applied breathing and grounding exercises to manage stress, consistent with previous MBI outcomes[11]. - Enhanced Emotional Regulation
Participants reported fewer emotional outbursts and better mood stability, a core benefit of mindfulness[10]. - Greater Empowerment and Agency
Meditation increased confidence and active participation in recovery, echoing mindfulness-based empowerment frameworks[14].
5. Discussion
The results of this study provide compelling evidence that mindfulness-based interventions (MBIs) offer a meaningful and multidimensional contribution to schizophrenia treatment. The significant improvements across symptom severity, cognitive performance, and quality-of-life domains demonstrate that meditation can complement traditional pharmacological approaches by addressing areas often resistant to medication, such as negative symptoms and cognitive impairments[1][2]. These findings add to a growing body of literature indicating that mindfulness practices exert both neurobiological and psychosocial effects, ultimately enhancing functional outcomes for individuals with schizophrenia.
One of the most notable outcomes was the consistent reduction across all PANSS domains, including positive, negative, and general psychopathology symptoms. Positive symptom reductions—such as decreased hallucination intensity and emotional distress—suggest that meditation may play a role in altering how individuals relate to intrusive sensory experiences. This aligns with previous findings showing that meditation enhances prefrontal regulation of limbic activation, thereby reducing emotional overreactivity and promoting calmer responses to internal stimuli[4][10]. The improvements in negative symptoms, which included reductions in social withdrawal and flat affect, are particularly promising, as these symptoms are notoriously difficult to treat and heavily impair daily functioning[2]. The medium-to-large effect sizes observed in this study suggest that mindfulness may address motivational and emotional domains often overlooked in conventional care.
Cognitive improvements further highlight the therapeutic potential of meditation. The Digit Span and Trail Making Test gains indicate enhanced attention, working memory, and executive functioning—domains closely linked to prefrontal cortex activation. Prior research demonstrates that meditation strengthens attentional networks by increasing cortical thickness, improving connectivity between attention-regulating regions, and reducing automatic cognitive drift[11][10]. This neuroplastic capacity may help counter cognitive deficits commonly present in schizophrenia, potentially improving treatment engagement, problem-solving, and decision-making.
The quality-of-life improvements—particularly in psychological well-being and social relationships—underscore meditation’s capacity to enhance emotional resilience and interpersonal functioning. These outcomes reflect meditation’s broader psychosocial benefits, including increased emotional regulation, reduced stress reactivity, and greater sense of grounding. Enhanced social relationships may stem from reduced irritability, improved emotional responses, and increased presence during interpersonal interactions. These findings align with global evidence connecting mindfulness with decreased rumination, increased positive affect, and improved interpersonal empathy[12][15].
The qualitative findings add depth and context to the quantitative improvements, revealing the personal and experiential dimensions of meditation practice. Increased self-awareness and emotional insight are consistent with the S-ART (self-awareness, self-regulation, and self-transcendence) model of mindfulness, which explains how meditation reshapes one’s relationship with internal experiences[14]. Reduced distress from hallucinations provides real-world evidence for meditation’s capacity to modify the emotional and cognitive appraisal of positive symptoms. Importantly, participants frequently described feeling empowered and more in control of their mental health—a transformative shift that traditional medication alone may not facilitate.
Cultural sensitivity emerged as a crucial factor in intervention success. Meditation practices tailored to individual cultural backgrounds, beliefs, and symptom profiles facilitated engagement and comfort. This highlights an important consideration for global mental health: culturally adapted care significantly improves adherence, therapeutic alliance, and patient satisfaction[13]. Because mindfulness originated in Asian contemplative traditions, including those practiced in Myanmar, culturally grounded delivery may increase relevance and accessibility in similar contexts.
Despite promising results, the study’s limitations include its modest sample size (n = 10 patients, n = 10 providers) and relatively short duration. Long-term studies are needed to determine whether improvements persist and whether meditation affects relapse rates, medication adherence, or long-term functional outcomes. Additionally, neuroimaging data would provide stronger mechanistic evidence by showing direct changes in brain structure and connectivity. Future research should explore integrating MBIs into routine clinical practice, training providers in culturally sensitive mindfulness delivery, and evaluating group-based versus individual meditation formats.
The combination of quantitative improvements and rich qualitative experiences suggests that meditation can address both biological and experiential components of schizophrenia.
Meditation reduces amygdala hyperactivity, strengthens prefrontal regulation[4], and promotes neuroplastic adaptations[15].
Psychosocially, it enhances emotional resilience, reduces stress, and improves interpersonal functioning[12][10].
Given that negative symptoms and cognitive impairments are often resistant to medication[1][2], meditation represents a powerful complementary tool in schizophrenia treatment.
6. Conclusion
Overall, this study reinforces that meditation is not merely a relaxation technique but a sophisticated therapeutic modality capable of influencing neural, cognitive, and emotional systems central to schizophrenia. When integrated thoughtfully into treatment plans, meditation may significantly enhance patient well-being, promote active recovery, and contribute to a more holistic, person-centered model of mental health care.
This entry is adapted from: https://scienceable.net/mindfulness-meditation-schizophrenia-symptom-relief-neuroplasticity-study/
References
- Christoph U Correll; Nina R Schooler; Negative Symptoms in Schizophrenia: A Review and Clinical Guide for Recognition, Assessment, and Treatment. Neuropsychiatr. Dis. Treat. 2020, ume 16, 519-534, .
- Dawn Bruijnzeel; Rajiv Tandon; Antipsychotic treatment of schizophrenia. We can do better. Asian J. Psychiatry 2017, 28, A1-A2, .
- Fadel Zeidan; Susan K. Johnson; Bruce J. Diamond; Zhanna David; Paula Goolkasian; Mindfulness meditation improves cognition: Evidence of brief mental training. Conscious. Cogn. 2010, 19, 597-605, .
- Yi-Yuan Tang; Britta K. Hölzel; Michael I. Posner; The neuroscience of mindfulness meditation. Nat. Rev. Neurosci. 2015, 16, 213-225, .
- Kirk V. Szczepkowski; George J. Demakis. Wechsler Adult Intelligence Scale; Springer Nature: Durham, NC, United States, 2017; pp. 1-4.
- Britta K. Hölzel; Sara W. Lazar; Tim Gard; Zev Schuman-Olivier; David R. Vago; Ulrich Ott; How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspect. Psychol. Sci. 2011, 6, 537-559, .
- Aung, Htet Lin, 2025, "Meditation and Symptom Relief in Schizophrenia: Supporting Data for Neuropsychological and ClinicalOutcomes", https://doi.org/10.7910/DVN/P2UNTY, Harvard Dataverse, V1
- Ralph M. Reitan; Validity of the Trail Making Test as an Indicator of Organic Brain Damage. Percept. Mot. Ski. 1958, 8, 271-276, .
- WHOQOL-BREF: Introduction, administration, 397 scoring, and generic version of the assessment. World Health Organization. Retrieved 2025-11-23
- Shauna L. Shapiro; Linda E. Carlson; John A. Astin; Benedict Freedman; Mechanisms of mindfulness. J. Clin. Psychol. 2005, 62, 373-386, .
- Antoine Lutz; Heleen A. Slagter; John D. Dunne; Richard J. Davidson; Attention regulation and monitoring in meditation. Trends Cogn. Sci. 2008, 12, 163-169, .
- Bassam Khoury; Tania Lecomte; Guillaume Fortin; Marjolaine Masse; Phillip Therien; Vanessa Bouchard; Marie-Andrée Chapleau; Karine Paquin; Stefan G. Hofmann; Mindfulness-based therapy: A comprehensive meta-analysis. Clin. Psychol. Rev. 2013, 33, 763-771, .
- Marina A. Khusid; Meena Vythilingam; The Emerging Role of Mindfulness Meditation as Effective Self-Management Strategy, Part 1: Clinical Implications for Depression, Post-Traumatic Stress Disorder, and Anxiety. Mil. Med. 2016, 181, 961-968, .
- David R. Vago; David A. Silbersweig; Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Front. Hum. Neurosci. 2012, 6, 296, .
- Michelle Melis; Gwen Schroyen; Juliette Pollefeyt; Filip Raes; Ann Smeets; Stefan Sunaert; Sabine Deprez; Katleen Van der Gucht; The Impact of Mindfulness-Based Interventions on Brain Functional Connectivity: a Systematic Review. Mindfulness 2022, 13, 1857-1875, .
