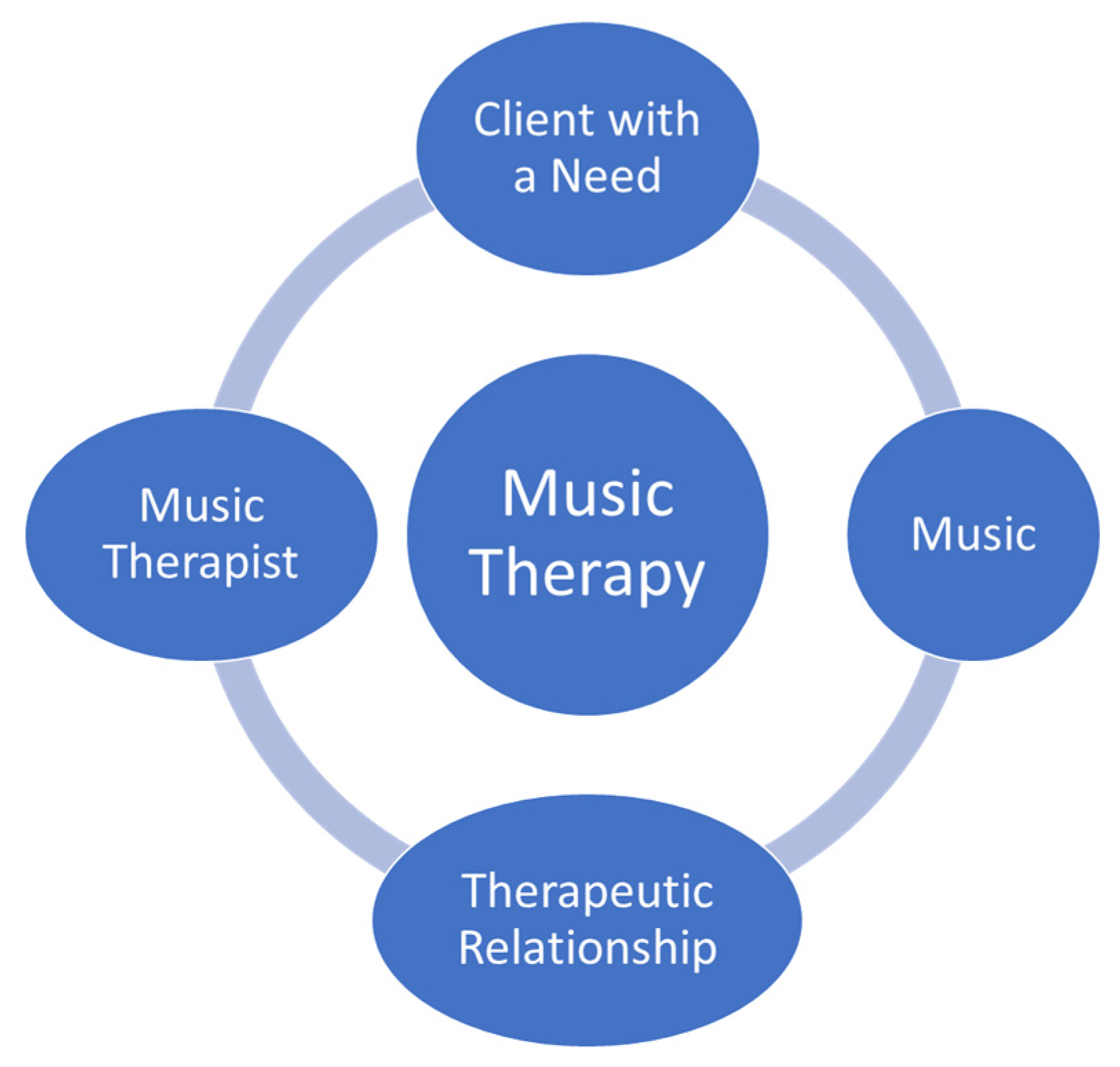
Certified music therapists use music within therapeutic relationships to address human needs, health, and well-being with a variety of populations. Palliative care and music therapy are holistic and diverse fields, adapting to unique issues within end-of-life contexts. Palliative care music therapy has been formally practiced since the late 1970s and affords a variety of benefits, including pain and anxiety reduction, enhancement of quality of life, emotional expression, and relationship completion.
- palliative care
- music therapy
- end-of-life
- relationships
1. Palliative Care
2. Music Based Interventions and Music Therapy in Palliative Care
3. What is the Evidence to Support Music Therapy in Palliative Care?
4. Education & Training to Become a Music Therapist
5. Clinical Supervision of Music Psychotherapy
-
Be a member in good standing of a regulatory college;
-
Have five years’ extensive clinical experience;
-
Complete 1000 direct client contact hours and 150 h of clinical supervision;
-
Provide a signed declaration noting they understand CRPO’s definitions of clinical supervision, clinical supervisor, and the scope of practice of psychotherapy [23]
This entry is adapted from the peer-reviewed paper 10.3390/healthcare12040459
References
- Hilliard, R.E. Music Therapy in Hospice and Palliative Care: A Review of the Empirical Data. Evid. Based Complement. Alternat. Med. 2005, 2, 173–178.
- Pommeret, S.; Chrusciel, J.; Verlaine, C.; Filbet, M.; Tricou, C.; Sanchez, S.; Hannetel, L. Music in palliative care: A qualitative study with patients suffering from cancer. BMC Palliat. Care 2019, 18, 78.
- Srolovitz, M.; Borgwardt, J.; Burkart, M.; Clements-Cortés, A.; Czamanski-Cohen, J.; Ortiz Guzman, M.; Hicks, M.G.; Kaimal, G.; Lederman, L.; Potash, J.S.; et al. Top ten tips palliative care clinicians should know about music therapy and art therapy. J. Palliat. Med. 2021, 25, 135–144.
- Warth, M.; Kessler, J.; Hillecke, T.K.; Bardenheuer, H.J. Trajectories of Terminally Ill Patients’ Cardiovascular Response to Receptive Music Therapy in Palliative Care. J. Pain Symptom Manag. 2016, 52, 196–204.
- Canadian Association of Music Therapists. What Is Music Therapy? 2020. Available online: https://www.musictherapy.ca/about-camt-music-therapy/about-music-therapy/ (accessed on 11 December 2023).
- Bradt, J.; Dileo, C.; Shim, M. Music interventions for pre-operative anxiety. Cochrane Database Syst. Rev. 2013, 6, CD006908.
- Clements-Cortés, A.; Bartel, L. Are we doing more than we know? Possible mechanisms of response to music therapy. Front. Med. 2018, 5, 255.
- Thaut, M.; Francisco, G.; Hoemberg, V. Editorial: The Clinical Neuroscience of Music: Evidence Based Approaches and Neurologic Music Therapy. Front. Neurosci. 2021, 15, 740329.
- Bradt, J.; Dileo, C. Music therapy for end-of-life care. Cochrane Database Syst. Rev. 2010, 1, CD007169.
- Gutgsell, K.J.; Schluchter, M.; Margevicius, S.; DeGolia, P.A.; McLaughlin, B.; Harris, M.; Mecklenburg, J.; Wiencek, C. Music therapy reduces pain in palliative care patients: A randomized controlled trial. J. Pain Symptom Manag. 2013, 45, 822–831.
- Horne-Thompson, A.; Grocke, D. The effect of music therapy on anxiety in patients who are terminally ill. J. Palliat. Med. 2008, 11, 582–590.
- Köhler, F.; Martin, Z.S.; Hertrampf, R.S.; Gäbel, C.; Kessler, J.; Ditzen, B.; Warth, M. Music Therapy in the Psychosocial Treatment of Adult Cancer Patients: A Systematic Review and Meta-Analysis. Front. Psychol. 2020, 11, 651.
- Lee, J.H. The Effects of Music on Pain: A Meta-Analysis. J. Music Ther. 2016, 53, 430–477.
- Schmid, W.; Rosland, J.H.; von Hofacker, S.; Hunskår, I.; Bruvik, F. Patient’s and health care provider’s perspectives on music therapy in palliative care—An integrative review. BMC Palliat. Care 2018, 17, 32.
- Clements-Cortés, A.; Yip, J. (Eds.) Relationship Completion in Palliative Care Music Therapy; Barcelona: Gilsum, NH, USA, 2021.
- Clements-Cortés A: The use of music in facilitating emotional expression in the terminally ill. Am. J. Hosp. Palliat. Med. 2004, 21, 255–260.
- McConnell, T.; Porter, S. The experience of providing end of life care at a children’s hospice: A qualitative study. BMC Palliat. Care 2017, 16, 15.
- Clements-Cortés, A. The effect of live music vs. taped music on pain and comfort in palliative care. Korean J. Music Ther. 2011, 13, 105–121.
- Clements-Cortes, A. Music therapy in end-of-life care: A review of the literature. In Voices of the Dying and Bereaved: Music Therapy Narratives; Clements-Cortes, A., Varvas Klinck, S., Eds.; Barcelona Publishers: Gilsum, NH, USA, 2016; pp. 5–34.
- Vesel, T.; Dave, S.; Soham, D. Music therapy and palliative care: Systematic review. J. Pain Symptom Manag. 2018, 56, e74.
- Gallagher, L.M.; Lagman, R.; Walsh, D.; Davis, M.P.; LeGrand, S.B. The clinical effects of music therapy in palliative medicine. Support. Care Cancer 2006, 14, 859–866.
- Reidy, J.; MacDonald, M.C. Use of palliative care music therapy in a hospital setting during COVID-19. J. Palliat. Med. 2021, 24, 1603–1605.
- College of Registered Psychotherapists of Ontario. Supervision. 2024. Available online: https://www.crpo.ca/supervision/#supervision_requirements (accessed on 9 January 2024).
