Fulminant myocarditis (FM) constitutes a severe and life-threatening form of acute cardiac injury associated with cardiogenic shock. The condition is characterised by rapidly progressing myocardial inflammation, leading to significant impairment of cardiac function. Due to the acute and severe nature of the disease, affected patients require urgent medical attention to mitigate adverse outcomes. Besides symptom-oriented treatment in specialised intensive care units (ICUs), the necessity for temporary mechanical cardiac support (MCS) may arise. Numerous patients depend on these treatment methods as a bridge to recovery or heart transplantation, while, in certain situations, permanent MCS systems can also be utilised as a long-term treatment option.
- mechanical circulatory support
- MCS
- fulminant myocarditis
- ECMO
- VAD
1. Acute Myocarditis and Transition to Fulminant Forms
| Authors | Time Period | Patients (n) | Type of MCS | Median Age | Outcomes |
|---|---|---|---|---|---|
| Aoyama, N., et al. [7] | 1989–2000 | 52 | VA-ECMO | ~48 years | 57.7% survival and return to normal life |
| Asaumi, Y., et al. [8] | 1993–2001 | 14 | VA-ECMO | ~38 years | 71.4% were weaned and survived to discharge |
| Hsu, K.H., et al. [9] | 1994–2009 | 75 | VA-ECMO | ~30 years | 61% survival to discharge |
| Ting, M., et al. [10] | 1994–2014 | 93 | VA-ECMO | ~42 years | 50.1% transplant-free survival |
| Ishida, K., et al. [11] | 1995–2010 | 20 | VA-ECMO | ~45 years | 60% survival to discharge |
| Diddle, J.W., et al. [12] | 1995–2011 | 147 | mainly VA-ECMO | ~31 years | 61% survival to discharge (9 HTx) |
| Matsumoto, M., et al. [13] | 1995–2014 | 37 | VA-ECMO | ~43 years | 59% successfully weaned from VA-ECMO |
| Chang, J.J., et al. [4] | 1997–2011 | 294 | 99 IABP/195 VA-ECMO | ~45/41 years | 81%/61% survival to discharge |
| Mirabel, M., et al. [14] | 2002–2009 | 35 | VA-ECMO | ~38 years | 68.6% survival to discharge |
| Wu, M.Y., et al. [15] | 2003–2010 | 16 | VA-ECMO | N/A | 87.5% survival to discharge |
| Beurtheret, S., et al. [16] | 2005–2009 | 14 | VA-ECMO | N/A | 65% survival to discharge |
| Chou, H.W., et al. [17] | 2006–2018 | 88 | VA-ECMO | ~42 years | 46.6% successful weaning and discharge |
| Tadokoro, N., et al. [18] | 2006–2020 | 70 | VA-ECMO cent. 48/periph.22 | ~44/50 years | 62%/95% weaning from VA-ECMO (total cohort survival 5 years: 76%) |
| Mody, K.P., et al. [19] | 2007–2013 | 11 | 3 VA-ECMO/8 Bi-VAD | ~48 years | 73% survival to discharge (2 permanent VAD) |
| Lorusso, R., et al. [20] | 2008–2013 | 57 | VA-ECMO | ~38 years | 72% survival to discharge |
| Saito, S., et al. [21] | 2009–2015 | 25 | 23 VA-ECMO/2 t-VAD | ~39 years | 83.3% survival to discharge (6 permanent VAD) |
| Annamalai, S.K., et al. [22] | 2009–2016 | 34 | Impella (2.5, CP, 5.0, or RP) | ~42 years | 61.8% survival to discharge (15 weaned, 5 transferred, 1 HTx) |
| Nunez, J.I., et al. [23] | 2011–2020 | 850 | VA-ECMO | ~41 years | 65.1% survival to discharge |
| Danial, P., et al. [24] | 2015–2018 | 47 | VA-ECMO | ~46 years | 37.9% survival to discharge |
| Tonna, J.E., et al. [25] | 2020–2021 | 88 | VA-ECMO | ~48 years | 49% survival to discharge (FM + COVID-19) |
| Ammirati, E., et al. [26] | 2020–2021 | 10 | IABP/VA-ECMO | ~38 years | 78.5% survival after 120 days (FM + COVID-19) |
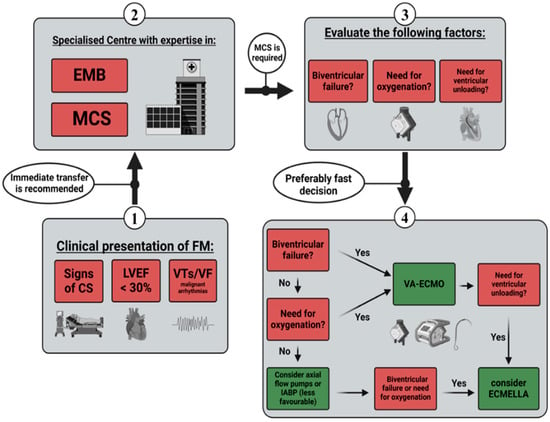
2. Indication and Timing of Short-Term MCS
3. Outcomes in Fulminant Myocarditis with Short-Term MCS
4. Ventricular Unloading in Short-Term MCS
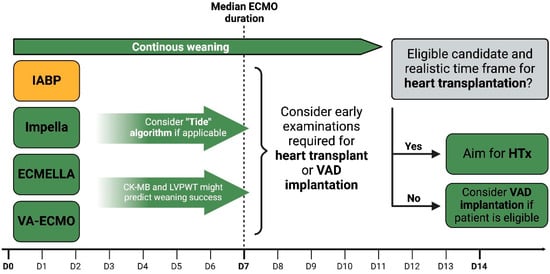
5. Weaning Strategies and Transition to Long-Term MCS
6. MCS and Additional Treatment in Lymphocytic Myocarditis
7. MCS and Additional Treatment in Giant Cell Myocarditis
8. MCS and Additional Treatment in Eosinophilic Myocarditis
This entry is adapted from the peer-reviewed paper 10.3390/jcm13051197
References
- Kociol, R.D.; Cooper, L.T.; Fang, J.C.; Moslehi, J.J.; Pang, P.S.; Sabe, M.A.; Shah, R.V.; Sims, D.B.; Thiene, G.; Vardeny, O. Recognition and Initial Management of Fulminant Myocarditis: A Scientific Statement from the American Heart Association. Circulation 2020, 141, e69–e92.
- Merlo, M.; Ammirati, E.; Gentile, P.; Artico, J.; Cannatà, A.; Finocchiaro, G.; Barbati, G.; Sormani, P.; Varrenti, M.; Perkan, A.; et al. Persistent left ventricular dysfunction after acute lymphocytic myocarditis: Frequency and predictors. PLoS ONE 2019, 14, e0214616.
- Ammirati, E.; Frigerio, M.; Adler, E.D.; Basso, C.; Birnie, D.H.; Brambatti, M.; Friedrich, M.G.; Klingel, K.; Lehtonen, J.; Moslehi, J.J.; et al. Management of Acute Myocarditis and Chronic Inflammatory Cardiomyopathy: An Expert Consensus Document. Circ. Heart Fail. 2020, 13, e007405.
- Chang, J.-J.; Lin, M.-S.; Chen, T.-H.; Chen, D.-Y.; Chen, S.-W.; Hsu, J.-T.; Wang, P.-C.; Lin, Y.-S. Heart Failure and Mortality of Adult Survivors from Acute Myocarditis Requiring Intensive Care Treatment—A Nationwide Cohort Study. Int. J. Med. Sci. 2017, 14, 1241–1250.
- Mensah, G.A.; Roth, G.A.; Fuster, V. The Global Burden of Cardiovascular Diseases and Risk Factors: 2020 and Beyond. J. Am. Coll. Cardiol. 2019, 74, 2529–2532.
- Ammirati, E.; Veronese, G.; Brambatti, M.; Merlo, M.; Cipriani, M.; Potena, L.; Sormani, P.; Aoki, T.; Sugimura, K.; Sawamura, A.; et al. Fulminant Versus Acute Nonfulminant Myocarditis in Patients with Left Ventricular Systolic Dysfunction. J. Am. Coll. Cardiol. 2019, 74, 299–311.
- Aoyama, N.; Izumi, T.; Hiramori, K.; Isobe, M.; Kawana, M.; Hiroe, M.; Hishida, H.; Kitaura, Y.; Imaizumi, T. National survey of fulminant myocarditis in Japan: Therapeutic guidelines and long-term prognosis of using percutaneous cardiopulmonary support for fulminant myocarditis (special report from a scientific committee). Circ. J. 2002, 66, 133–144.
- Asaumi, Y.; Yasuda, S.; Morii, I.; Kakuchi, H.; Otsuka, Y.; Kawamura, A.; Sasako, Y.; Nakatani, T.; Nonogi, H.; Miyazaki, S. Favourable clinical outcome in patients with cardiogenic shock due to fulminant myocarditis supported by percutaneous extracorporeal membrane oxygenation. Eur. Heart J. 2005, 26, 2185–2192.
- Hsu, K.H.; Chi, N.H.; Yu, H.Y.; Wang, C.H.; Huang, S.C.; Wang, S.S.; Ko, W.J.; Chen, Y.S. Extracorporeal membranous oxygenation support for acute fulminant myocarditis: Analysis of a single center’s experience. Eur. J. Cardiothorac. Surg. 2011, 40, 682–688.
- Ting, M.; Wang, C.H.; Tsao, C.I.; Huang, S.C.; Chi, N.H.; Chou, N.K.; Chen, Y.S.; Wang, S.S. Heart Transplantation Under Mechanical Circulatory Support for Acute Fulminant Myocarditis with Cardiogenic Shock: 10 Years’ Experience of a Single Center. Transpl. Transplant. Proc. 2016, 48, 951–955.
- Ishida, K.; Wada, H.; Sakakura, K.; Kubo, N.; Ikeda, N.; Sugawara, Y.; Ako, J.; Momomura, S.-I. Long-term follow-up on cardiac function following fulminant myocarditis requiring percutaneous extracorporeal cardiopulmonary support. Heart Vessels 2013, 28, 86–90.
- Diddle, J.W.; Almodovar, M.C.; Rajagopal, S.K.; Rycus, P.T.; Thiagarajan, R.R. Extracorporeal membrane oxygenation for the support of adults with acute myocarditis. Crit. Care Med. 2015, 43, 1016–1025.
- Matsumoto, M.; Asaumi, Y.; Nakamura, Y.; Nakatani, T.; Nagai, T.; Kanaya, T.; Kawakami, S.; Honda, S.; Kataoka, Y.; Nakajima, S.; et al. Clinical determinants of successful weaning from extracorporeal membrane oxygenation in patients with fulminant myocarditis. ESC Heart Fail. 2018, 5, 675–684.
- Mirabel, M.; Luyt, C.-E.; Leprince, P.; Trouillet, J.-L.; Léger, P.; Pavie, A.; Chastre, J.; Combes, A. Outcomes, long-term quality of life, and psychologic assessment of fulminant myocarditis patients rescued by mechanical circulatory support. Crit. Care Med. 2011, 39, 1029–1035.
- Wu, M.-Y.; Lee, M.-Y.; Lin, C.-C.; Chang, Y.-S.; Tsai, F.-C.; Lin, P.-J. Resuscitation of non-postcardiotomy cardiogenic shock or cardiac arrest with extracorporeal life support: The role of bridging to intervention. Resuscitation 2012, 83, 976–981.
- Beurtheret, S.; Mordant, P.; Paoletti, X.; Marijon, E.; Celermajer, D.S.; Léger, P.; Pavie, A.; Combes, A.; Leprince, P. Emergency circulatory support in refractory cardiogenic shock patients in remote institutions: A pilot study (the cardiac-RESCUE program). Eur. Heart J. 2013, 34, 112–120.
- Chou, H.-W.; Wang, C.-H.; Lin, L.-Y.; Chi, N.-H.; Chou, N.-K.; Yu, H.-Y.; Chen, Y.-S. Prognostic factors for heart recovery in adult patients with acute fulminant myocarditis and cardiogenic shock supported with extracorporeal membrane oxygenation. J. Crit. Care 2020, 57, 214–219.
- Tadokoro, N.; Fukushima, S.; Minami, K.; Taguchi, T.; Saito, T.; Kawamoto, N.; Kakuta, T.; Seguchi, O.; Watanabe, T.; Doi, S.N.; et al. Efficacy of central extracorporeal life support for patients with fulminant myocarditis and cardiogenic shock. Eur. J. Cardio-Thorac. Surg. 2021, 60, 1184–1192.
- Mody, K.P.; Takayama, H.; Landes, E.; Yuzefpolskaya, M.; Colombo, P.C.; Naka, Y.; Jorde, U.P.; Uriel, N. Acute mechanical circulatory support for fulminant myocarditis complicated by cardiogenic shock. J. Cardiovasc. Transl. Res. 2014, 7, 156–164.
- Lorusso, R.; Centofanti, P.; Gelsomino, S.; Barili, F.; Di Mauro, M.; Orlando, P.; Botta, L.; Milazzo, F.; Dato, G.A.; Casabona, R.; et al. Venoarterial Extracorporeal Membrane Oxygenation for Acute Fulminant Myocarditis in Adult Patients: A 5-Year Multi-Institutional Experience. Ann. Thorac. Surg. 2016, 101, 919–926.
- Saito, S.; Toda, K.; Miyagawa, S.; Yoshikawa, Y.; Hata, H.; Yoshioka, D.; Domae, K.; Tsukamoto, Y.; Sakata, Y.; Sawa, Y. Diagnosis, medical treatment, and stepwise mechanical circulatory support for fulminat myocarditis. J. Artif. Organs 2018, 21, 172–179.
- Annamalai, S.K.; Esposito, M.L.; Jorde, L.; Schreiber, T.; Hall, S.A.; O’Neill, W.W.; Kapur, N.K. The Impella Microaxial Flow Catheter Is Safe and Effective for Treatment of Myocarditis Complicated by Cardiogenic Shock: An Analysis from the Global cVAD Registry. J. Card. Fail. 2018, 24, 706–710.
- Nunez, J.I.; Grandin, E.W.; Reyes-Castro, T.; Sabe, M.; Quintero, P.; Motiwala, S.; Fleming, L.M.; Sriwattanakomen, R.; Ho, J.E.; Kennedy, K.; et al. Outcomes with Peripheral Venoarterial Extracorporeal Membrane Oxygenation for Suspected Acute Myocarditis: 10-Year Experience From the Extracorporeal Life Support Organization Registry. Circ. Heart Fail. 2023, 16, e010152.
- Danial, P.; Olivier, M.-E.; Bréchot, N.; Ponnaiah, M.; Schoell, T.; D’Alessandro, C.; Demondion, P.; Clément, M.; Juvin, C.; Carillion, A.; et al. Association Between Shock Etiology and 5-Year Outcomes After Venoarterial Extracorporeal Membrane Oxygenation. J. Am. Coll. Cardiol. 2023, 81, 897–909.
- Tonna, J.E.; Tan, C.S.; Hryniewicz, K.; Barbaro, R.P.; Brodie, D.; MacLaren, G. Outcomes after extracorporeal life support for COVID-19 myocarditis: An analysis of the Extracorporeal Life Support Organization Registry. Crit. Care 2022, 26, 235.
- Ammirati, E.; Lupi, L.; Palazzini, M.; Hendren, N.S.; Grodin, J.L.; Cannistraci, C.V.; Schmidt, M.; Hekimian, G.; Peretto, G.; Bochaton, T.; et al. Prevalence, Characteristics, and Outcomes of COVID-19-Associated Acute Myocarditis. Circulation 2022, 145, 1123–1139.
- Caforio, A.L.P.; Pankuweit, S.; Arbustini, E.; Basso, C.; Gimeno-Blanes, J.; Felix, S.B.; Fu, M.; Heliö, T.; Heymans, S.; Jahns, R.; et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur. Heart J. 2013, 34, 2636–2648.
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Rev. Esp. Cardiol. (Engl. Ed.) 2022, 75, 523.
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2024, 44, 3627–3639.
- Crespo-Leiro, M.G.; Metra, M.; Lund, L.H.; Milicic, D.; Costanzo, M.R.; Filippatos, G.; Gustafsson, F.; Tsui, S.; Barge-Caballero, E.; De Jonge, N.; et al. Advanced heart failure: A position statement of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018, 20, 1505–1535.
- Tehrani, B.N.; Truesdell, A.G.; Sherwood, M.; Desai, S.; Tran, H.A.; Epps, K.C.; Singh, R.; Psotka, M.; Shah, P.; Cooper, L.B.; et al. Standardized Team-Based Care for Cardiogenic Shock. J. Am. Coll. Cardiol. 2019, 73, 1659–1669.
- Basir, M.B.; Kapur, N.K.; Patel, K.; Salam, M.A.; Schreiber, T.; Kaki, A.; Hanson, I.; Almany, S.; Timmis, S.; Dixon, S.; et al. Improved Outcomes Associated with the use of Shock Protocols: Updates from the National Cardiogenic Shock Initiative. Catheter. Cardiovasc. Interv. 2019, 93, 1173–1183.
- Thiele, H.; Zeymer, U.; Neumann, F.-J.; Ferenc, M.; Olbrich, H.-G.; Hausleiter, J.; Richardt, G.; Hennersdorf, M.; Empen, K.; Fuernau, G.; et al. Intraaortic balloon support for myocardial infarction with cardiogenic shock. N. Engl. J. Med. 2012, 367, 1287–1296.
- Combes, A.; Price, S.; Slutsky, A.S.; Brodie, D. Temporary circulatory support for cardiogenic shock. Lancet 2020, 396, 199–212.
- Thiele, H.; Zeymer, U.; Akin, I.; Behnes, M.; Rassaf, T.; Mahabadi, A.A.; Lehmann, R.; Eitel, I.; Graf, T.; Seidler, T.; et al. Extracorporeal Life Support in Infarct-Related Cardiogenic Shock. N. Engl. J. Med. 2023, 389, 1286–1297.
- Pahuja, M.; Adegbala, O.; Mishra, T.; Akintoye, E.; Chehab, O.; Mony, S.; Singh, M.; Ando, T.; Abubaker, H.; Yassin, A.; et al. Trends in the Incidence of In-Hospital Mortality, Cardiogenic Shock, and Utilization of Mechanical Circulatory Support Devices in Myocarditis (Analysis of National Inpatient Sample Data, 2005–2014). J. Card. Fail. 2019, 25, 457–467.
- Lee, H.-H.; Kim, H.C.; Ahn, C.-M.; Lee, S.-J.; Hong, S.-J.; Yang, J.H.; Kim, J.-S.; Kim, B.-K.; Ko, Y.-G.; Choi, D.; et al. Association Between Timing of Extracorporeal Membrane Oxygenation and Clinical Outcomes in Refractory Cardiogenic Shock. JACC Cardiovasc. Interv. 2021, 14, 1109–1119.
- Sheu, J.-J.; Tsai, T.-H.; Lee, F.-Y.; Fang, H.-Y.; Sun, C.-K.; Leu, S.; Yang, C.-H.; Chen, S.-M.; Hang, C.-L.; Hsieh, Y.-K.; et al. Early extracorporeal membrane oxygenator-assisted primary percutaneous coronary intervention improved 30-day clinical outcomes in patients with ST-segment elevation myocardial infarction complicated with profound cardiogenic shock. Crit. Care Med. 2010, 38, 1810–1817.
- Wang, J.; Han, J.; Jia, Y.; Zeng, W.; Shi, J.; Hou, X.; Meng, X. Early and intermediate results of rescue extracorporeal membrane oxygenation in adult cardiogenic shock. Ann. Thorac. Surg. 2009, 88, 1897–1903.
- Tschöpe, C.; Van Linthout, S.; Klein, O.; Mairinger, T.; Krackhardt, F.; Potapov, E.V.; Schmidt, G.; Burkhoff, D.; Pieske, B.; Spillmann, F. Mechanical Unloading by Fulminant Myocarditis: LV-IMPELLA, ECMELLA, BI-PELLA, and PROPELLA Concepts. J. Cardiovasc. Transl. Res. 2019, 12, 116–123.
- Van Linthout, S.; Tschöpe, C. Inflammation—Cause or Consequence of Heart Failure or Both? Curr. Heart Fail. Rep. 2017, 14, 251–265.
- Saegusa, H.; Komatsu, J.; Sugane, H.; Hosoda, H.; Imai, R.-I.; Nakaoka, Y.; Nishida, K.; Seki, S.-I.; Kubokawa, S.-I.; Kawai, K.; et al. Fulminant lymphocytic myocarditis: Prediction of successful weaning from Impella support for cardiogenic shock. J. Cardiol. Cases 2022, 25, 159–162.
- Andrade, J.G.; Al-Saloos, H.; Jeewa, A.; Sandor, G.G.; Cheung, A. Facilitated cardiac recovery in fulminant myocarditis: Pediatric use of the Impella LP 5.0 pump. J. Heart Lung Transpl. 2010, 29, 96–97.
- Fox, H.; Farr, M.; Horstkotte, D.; Flottmann, C. Fulminant Myocarditis Managed by Extracorporeal Life Support (Impella(R) CP): A Rare Case. Case Rep. Cardiol. 2017, 2017, 9231959.
- Lamarche, Y.; Cheung, A.; Ignaszewski, A.; Higgins, J.; Kaan, A.; Griesdale, D.E.; Moss, R. Comparative outcomes in cardiogenic shock patients managed with Impella microaxial pump or extracorporeal life support. J. Thorac. Cardiovasc. Surg. 2011, 142, 60–65.
- Cameli, M.; Pastore, M.C.; Campora, A.; Lisi, M.; Mandoli, G.E. Donor shortage in heart transplantation: How can we overcome this challenge? Front. Cardiovasc. Med. 2022, 9, 1001002.
- Den Uil, C.A.; Akin, S.; Jewbali, L.S.; dos Reis Miranda, D.; Brugts, J.J.; Constantinescu, A.A.; Kappetein, A.P.; Caliskan, K. Short-term mechanical circulatory support as a bridge to durable left ventricular assist device implantation in refractory cardiogenic shock: A systematic review and meta-analysis. Eur. J. Cardiothorac. Surg. 2017, 52, 14–25.
- Lee, E.-P.; Chu, S.-C.; Huang, W.-Y.; Hsia, S.-H.; Chan, O.-W.; Lin, C.-Y.; Su, Y.-T.; Chang, Y.-S.; Chung, H.-T.; Wu, H.-P.; et al. Factors Associated with In-hospital Mortality of Children with Acute Fulminant Myocarditis on Extracorporeal Membrane Oxygenation. Front. Pediatr. 2020, 8, 488.
- Huang, Y.-F.; Hsu, P.-S.; Tsai, C.-S.; Tsai, Y.-T.; Lin, C.-Y.; Ke, H.-Y.; Lin, Y.-C.; Yang, H.-Y. Levitronix bilateral ventricular assist device, a bridge to recovery in a patient with acute fulminant myocarditis and concomitant cerebellar infarction. Cardiovasc. J. Afr. 2018, 29, e1–e4.
- Jaroszewski, D.E.; Marranca, M.C.; Pierce, C.N.; Wong, R.K.; Steidley, E.D.; Scott, R.L.; DeValeria, P.A.; Arabia, F. Successive circulatory support stages: A triple bridge to recovery from fulminant myocarditis. J. Heart Lung Transplant. 2009, 28, 984–986.
- Lam, L.; Sathirareuangchai, S.; Oyama, J.; Devendra, G.; Hong, R. Lymphocytic Myocarditis and Cardiogenic Shock in Hawai’i: A Case Series. Hawaii J. Health Soc. Welf. 2019, 78, 223–229.
- Olinde, K.D.; O’Connell, J.B. Inflammatory heart disease: Pathogenesis, clinical manifestations, and treatment of myocarditis. Annu. Rev. Med. 1994, 45, 481–490.
- Cooper, L.T., Jr. Myocarditis. N. Engl. J. Med. 2009, 360, 1526–1538.
- Massilamany, C.; Huber, S.A.; Cunningham, M.W.; Reddy, J. Relevance of molecular mimicry in the mediation of infectious myocarditis. J. Cardiovasc. Transl. Res. 2014, 7, 165–171.
- Atluri, P.; Ullery, B.W.; MacArthur, J.W.; Goldstone, A.B.; Fairman, A.S.; Hiesinger, W.; Acker, M.A.; Woo, Y.J. Rapid onset of fulminant myocarditis portends a favourable prognosis and the ability to bridge mechanical circulatory support to recovery. Eur. J. Cardio-Thorac. Surg. 2013, 43, 379–382.
- Mason, J.W.; O’Connell, J.B.; Herskowitz, A.; Rose, N.R.; McManus, B.M.; Billingham, M.E.; Moon, T.E. A clinical trial of immunosuppressive therapy for myocarditis. The Myocarditis Treatment Trial Investigators. N. Engl. J. Med. 1995, 333, 269–275.
- Blauwet, L.A.; Cooper, L.T. Idiopathic giant cell myocarditis and cardiac sarcoidosis. Heart Fail. Rev. 2013, 18, 733–746.
- Cooper, L.T.; Berry, G.J.; Shabetai, R. Idiopathic giant-cell myocarditis—Natural history and treatment. Multicenter Giant Cell Myocarditis Study Group Investigators. N. Engl. J. Med. 1997, 336, 1860–1866.
- Okura, Y.; Dec, G.; Hare, J.M.; Kodama, M.; Berry, G.J.; Tazelaar, H.D.; Bailey, K.R.; Cooper, L.T. A clinical and histopathologic comparison of cardiac sarcoidosis and idiopathic giant cell myocarditis. J. Am. Coll. Cardiol. 2003, 41, 322–329.
- Kandolin, R.; Lehtonen, J.; Salmenkivi, K.; Räisänen-Sokolowski, A.; Lommi, J.; Kupari, M. Diagnosis, treatment, and outcome of giant-cell myocarditis in the era of combined immunosuppression. Circ. Heart Fail. 2013, 6, 15–22.
- Brilakis, E.S.; Olson, L.J.; Berry, G.J.; Daly, R.C.; Loisance, D.; Zucker, M.; Cooper, L.T. Survival outcomes of patients with giant cell myocarditis bridged by ventricular assist devices. ASAIO J. 2000, 46, 569–572.
- Elamm, C.A.; Al-Kindi, S.G.; Bianco, C.M.; Dhakal, B.P.; Oliveira, G.H. Heart Transplantation in Giant Cell Myocarditis: Analysis of the United Network for Organ Sharing Registry. J. Card. Fail. 2017, 23, 566–569.
- Davies, R.A.; Veinot, J.P.; Smith, S.; Struthers, C.; Hendry, P.; Masters, R. Giant cell myocarditis: Clinical presentation, bridge to transplantation with mechanical circulatory support, and long-term outcome. J. Heart Lung Transplant. 2002, 21, 674–679.
- Cooper, L.T.; Hare, J.M.; Tazelaar, H.D.; Edwards, W.D.; Starling, R.C.; Deng, M.C.; Menon, S.; Mullen, G.M.; Jaski, B.; Bailey, K.R.; et al. Usefulness of Immunosuppression for Giant Cell Myocarditis. Am. J. Cardiol. 2008, 102, 1535–1539.
- Ekström, K.; Lehtonen, J.; Kandolin, R.; Räisänen-Sokolowski, A.; Salmenkivi, K.; Kupari, M. Long-term outcome and its predictors in giant cell myocarditis. Eur. J. Heart Fail. 2016, 18, 1452–1458.
- Patel, P.M.; Saxena, A.; Wood, C.T.; O’malley, T.J.; Maynes, E.J.; Entwistle, J.W.C.; Massey, H.T.; Pirlamarla, P.R.; Alvarez, R.J.; Cooper, L.T.; et al. Outcomes of Mechanical Circulatory Support for Giant Cell Myocarditis: A Systematic Review. J. Clin. Med. 2020, 9, 3905.
- Ashikaga, K.; Kida, K.; Akashi, Y.J. A case of fully recovered giant cell myocarditis treated with immunosuppression therapy. Int. J. Cardiol. 2013, 167, e149–e151.
- Löffler, W. Scientific raisins from 125 years SMW (Swiaa Medical Weekly). 2nd international medical week dedicated in Switzerland. Luzern, 31 August-5 September 1936. Fibroplastic parietal endocarditis with eosinophilia. An unusual disease. 1936. Schweiz. Med. Wochenschr. 1995, 125, 1837–1840.
- Pieroni, M.; Cavallaro, R.; Chimenti, C.; Smeraldi, E.; Frustaci, A. Clozapine-induced hypersensitivity myocarditis. Chest 2004, 126, 1703–1705.
- Ammirati, E.; Cipriani, M.; Musca, F.; Bonacina, E.; Pedrotti, P.; Roghi, A.; Astaneh, A.; Schroeder, J.W.; Nonini, S.; Russo, C.F.; et al. A life-threatening presentation of eosinophilic granulomatosis with polyangiitis. J. Cardiovasc. Med. 2016, 17 (Suppl. S2), e109–e111.
- Roehrl, M.H.A.; Alexander, M.P.; Hammond, S.B.; Ruzinova, M.; Wang, J.Y.; O’Hara, C.J. Eosinophilic myocarditis in hypereosinophilic syndrome. Am. J. Hematol. 2011, 86, 607–608.
- Enko, K.; Tada, T.; Ohgo, K.O.; Nagase, S.; Nakamura, K.; Ohta, K.; Ichiba, S.; Ujike, Y.; Nawa, Y.; Maruyama, H.; et al. Fulminant eosinophilic myocarditis associated with visceral larva migrans caused by Toxocara canis infection. Circ. J. 2009, 73, 1344–1348.
- Ammirati, E.; Stucchi, M.; Brambatti, M.; Spanò, F.; Bonacina, E.; Recalcati, F.; Cerea, G.; Vanzulli, A.; Frigerio, M.; Oliva, F. Eosinophilic myocarditis: A paraneoplastic event. Lancet 2015, 385, 2546.
- Brambatti, M.; Matassini, M.V.; Adler, E.D.; Klingel, K.; Camici, P.G.; Ammirati, E. Eosinophilic Myocarditis: Characteristics, Treatment, and Outcomes. J. Am. Coll. Cardiol. 2017, 70, 2363–2375.
- Al Ali, A.M.; Straatman, L.P.; Allard, M.F.; Ignaszewski, A.P. Eosinophilic myocarditis: Case series and review of literature. Can. J. Cardiol. 2006, 22, 1233–1237.
- Kontani, M.; Takashima, S.-I.; Okura, K.; Takemori, H.; Maeno, K.; Tanaka, N.; Ohashi, H.; Noriki, S. Survival after acute necrotizing eosinophilic myocarditis complicating a massive left ventricular mural thrombus: A case report. J. Cardiol. 2007, 50, 127–133.
- Allderdice, C.; Marcu, C.; Kabirdas, D. Intracardiac Thrombus in Leukemia: Role of Cardiac Magnetic Resonance Imaging in Eosinophilic Myocarditis. CASE 2018, 2, 114–117.
- Callan, P.D.; Baltabaeva, A.; Kamal, M.; Wong, J.; Lane, R.; Robertus, J.L.; Banner, N.R. Acute fulminant necrotizing eosinophilic myocarditis: Early diagnosis and treatment. ESC Heart Fail. 2017, 4, 660–664.
- Yonenaga, A.; Hasumi, E.; Fujiu, K.; Ushiku, A.; Hatano, M.; Ando, J.; Morita, H.; Watanabe, M.; Komuro, I. Prognostic Improvement of Acute Necrotizing Eosinophilic Myocarditis (ANEM) Through a Rapid Pathological Diagnosis and Appropriate Therapy. Int. Heart J. 2018, 59, 641–646.
- Cooper, L.T.; Zehr, K.J. Biventricular assist device placement and immunosuppression as therapy for necrotizing eosinophilic myocarditis. Nat. Clin. Pract. Cardiovasc. Med. 2005, 2, 544–548.
- Koehler, U.; Ghahremann, M.; Jerrentrup, A.; Just, M.; Löwer, R.; Moll, R.; Portig, I.; von Wichert, P. Eosinophilic myocarditis in Churg-Strauss syndrome. A rare cause of left heart decompensation with lung edema. Dtsch. Med. Wochenschr. 2000, 125, 1323–1327.
- Howell, E.; Paivanas, N.; Stern, J.; Vidula, H. Treatment of Acute Necrotizing Eosinophilic Myocarditis with Immunosuppression and Mechanical Circulatory Support. Circ. Heart Fail. 2016, 9, e003665.
