In the context of clinical practice, situational awareness refers to conscious awareness (knowledge), which is a mental model of a given clinical situation in terms of its elements and the significance of their interrelation. Situational awareness (SA) facilitates clinical reasoning, diagnostic accuracy, and appropriate goal-directed performance, and it enables clinicians to immediately adapt treatment strategies in response to changes in clinical situational actualities and to modify the course of goal-directed activities accordingly. It also helps clinicians prepare future operational plans and procedures based on the projection of situational developments. SA, therefore, is an important prerequisite for safe clinical procedures.
1. Introduction
Situational awareness (SA), domain-specific clinical knowledge and technical skills, and non-technical skills, such as teamwork, communication, cognition, and self-control, are some of the most important factors contributing to the efficient and effective processes of clinical judgment, decision making, and subsequently, synchronized goal-directed activities [
1,
2]. SA is a dynamic state of conscious awareness [
2,
3] that is brought about by complex interactions between multiple cognitive factors, including attention, working memory, long-term memory, cognitive flexibility, and rule acquisition [
2,
4] and by drawing from pre-determined mental models that have been developed via repeated relevant situational experiences and clinical training [
4].
SA can be viewed as one’s knowledge about a given situation's elements and circumstances [
5,
6,
7], and this conscious awareness plays an important role in a decision maker’s ability to manage complex and dynamic external tasks through adaptive goal-directed actions [
3]. It facilitates the process of decision making in the face of rapidly changing situational actualities and enables decision makers to anticipate and subsequently manage unplanned task descriptions and goal-directed demands under uncertain operational circumstances [
4].
A complex clinical situation generates multiple internal representations, some of which may be contradictory, and each such internal representation may require a different goal-directed action to solve the clinical problem, thus contributing to the uncertain nature of clinical decision making [
8]. The integration of successive new pieces of relevant situational information and the identification and resolution of conflicting perceptions are essential for developing and maintaining high-level SA and enable clinicians to form and support an accurate, comprehensive mental model of a situation [
6,
9,
10].
In the context of clinical practice, SA—that is, the integrated representation of a clinical problem—is essential for the processes of clinical reasoning, judgment, decision making, and performance [
6,
11,
12], and it enables the anticipation of evolving changes in current situational actualities and task descriptions based on similarities with past clinical situations.
Many factors may contribute to the faulty detection, capturing, and processing of situational clinical data and information, which may lead to the construction of an inaccurate SA with subsequent diagnostic errors and unfavorable treatment outcomes. These factors include mental exhaustion resulting from excessive cognitive demands associated with data and information processing and from a decrease in resources of mental energy; exposure to work overload and to work-related stressors, task saturation, fatigue, burnout, and negative emotional stimuli; and cognitive activities that divert attention away from goal-directed tasks [
6,
7,
9,
13,
14]. O
2. The Situational Awareness Construct
The framework of situational awareness (SA) refers to SA as an evolving state of knowledge about the dynamically interacting elements of a given situation [
7,
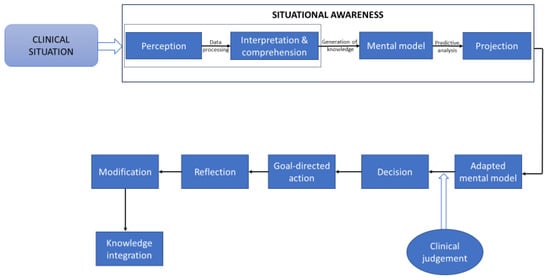
9]. According to this framework, all situational knowledge is generated by sequential cognitive steps that promote information processing, and it enables predictions of the immediate future state of an evolving situation (
Figure 1) [
7,
20]. SA can be viewed as a comprehensive and coherent internal representation of any current situational actualities; it is continuously assessed and updated in accordance with the dynamic state of the situation [
10,
21] and is imprinted in the consciousness of the decision maker [
3,
20].
Figure 1. A simplified diagram showing the cognitive information processing pathway that is used in the development of situational awareness, decision making, and clinical operations. The ‘perception’ component of this pathway captures the situational characteristics obtained from the patient’s history, physical examinations, and diagnostic test results. The interpretation and comprehension of the perceived information are determined by using pattern recognition processes, by using the clinician’s cognitive skills, memory capacity, and domain-specific competence, and by considering expert and second opinions. All of these factors are essential for constructing situational mental models, and comprehensive knowledge of the situational constraints enables the formulation of differential and working diagnoses, as well as the performance of adaptive goal-oriented activities [
6]. The ‘projection’ component deals with situational predictive analyses and with the search for additional situation-related and relevant scientific information, with the consideration of alternative treatment options, and with forecasting treatment outcomes and ongoing changes in situational eventualities [
6]. Based on the acquired situational awareness and adapted ‘mental model’, a decision is made, and it is followed by the execution of the planned goal-directed tasks. Subsequently, the process of reflection in relation to the operational plans and tasks is conducted. Finally, the newly acquired knowledge is integrated within pre-determined mental models [
7,
9,
15,
22].
Thus, SA should be regarded only as a description or label of an internal representation of a given situation and not as a cognitive mechanism or process in itself [
9,
21,
23]. The cognitive mechanisms that play active roles in developing a meaningful conscious awareness about a given situation include long-term memory, short-term memory, attention, and other executive functions, but not SA itself [
7]. Situational awareness is not an empirical reality but an abstract construct; a failure of a clinical operation associated with deficient SA cannot be attributed to an ‘impaired’ SA but rather to the imperfect functional activity of the psychological mechanism that generated it [
24].
3. Information-Processing Procedures in Relation to Situational Awareness
Reasoning is a cognitive activity that uses information-processing procedures to drive rational processes in order to solve problems; the dynamic and interconnected relationships between data, information, and knowledge are a fundamental prerequisite for clinical reasoning. Data are a collection of unorganized or uncontextualized objective facts, while information is contextualized data that convey values, meanings, and purposes.
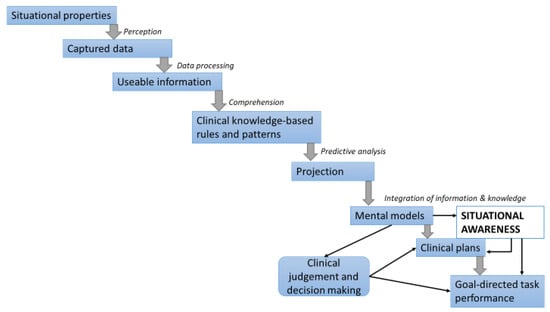
There is a hierarchal bidirectional relationship among data, information, and knowledge, and this comprises a bottom-up and a top-down direction. In the bottom-up hierarchy, cognitive information-processing activities include capturing situational data and gathering basic informative elements (perception stage), processing data into usable information that is then transformed into clinical-knowledge-based rules and patterns that support clinical judgments and decision making (comprehensive or understanding stage), and predictive analysis (projection stage), all of which enable the execution of goal-directed clinical tasks (
Figure 2) [
28,
29].
Figure 2. Bottom-up information processing pathway that enables clinical judgments, decision making, choices, and adaptive goal-directed clinical operation [
28,
29].
In the top-down hierarchy, the relevant predetermined knowledge, past experience, putative plans and goals, and established expectations are prerequisites for the selection, analysis, and interpretation of the collected data and for how the information-processing operation is performed [
28]. Thus, depending on the given clinical situational actualities and on the clinician’s operative goals, the information-processing operations that bring about SA will be top-down (goal-directed), bottom-up (data-directed), or a combination of both.
Three information-processing cognitive modes, namely, skill-, rule-, and knowledge-based modes, which differ in relation to the degree of the conscious control employed for their operations, are used to develop SA and clinical reasoning. Skill-based activities are highly automated and are performed with minimal conscious awareness; rule-based activities use a higher level of conscious control and are driven by predetermined mental models, standardized subordinates, and stored rules and guidelines that have been developed in association with similar previously managed clinical situations; knowledge-based activities employ the highest level of conscious control, which necessitates the de novo generation of plans and goal-directed decisions and of mental modes on an ad hoc basis through deliberate, time-consuming, analytical, and cognitively effortful processes [
19,
30,
31].
The use of clinical decision support systems and electronic health records provides clinicians with important patient-related information and with computer-generated clinical knowledge that includes risk assessments, risk reduction factors, clinical-knowledge-based rules and patterns, and predictive analyses of probable post-intervention clinical outcomes. This information and knowledge are generated from the patient’s medical history and through data mining, machine learning techniques, and statistical modeling [
29].
4. Clinical Judgments and Decision Making in Relation to Situational Awareness
The cognitive processes that are required to develop an accurate clinical SA force clinicians to focus their attention and to allocate resources of mental energy to the given situational elements and then to analyze and interpret the captured data and perceived information in the context of the situational constraints and of the performance of the goal-directed tasks. Goal-directed tasks may be pre-determined, and in such cases, the clinician’s role is to identify situational cues that are necessary for the efficient and effective execution of the prescribed plan (top-down); or, in the case of goal-directed activities that still need to be constructed, the clinician has to recognize situational cues that will enable the categorization and conceptualization of the current situation in accordance with previous similar mental situational models. This pattern recognition process facilitates clinical judgments, decision making, and the planning of appropriate goal-directed activities (bottom-up) [
21] (Flach, 1995) [
19].
The cognitive pathways involved in information processing in relation to solving clinical problems comprise a non-conscious, automatic, intuitive, and fast reasoning pathway (system 1), as well as a conscious, deliberate, analytical, effortful, and time-consuming reasoning pathway (system 2) [
22,
32,
33].
In the context of clinical practice, a given clinical problem may be typical, atypical, or complex, and it may display elements of uncertainty and/or ambiguity [
16,
22,
34]. Depending on the nature of the clinical situation and on the cognitive functions required for driving the decision-making process, system 1 and system 2 may either operate sequentially with system 1 being the first in action, followed by the analytical and deliberate system 2, which monitors and, if necessary, corrects the intuitive judgments and decisions constructed by system 1, or they may operate concurrently or interchangeably [
16,
22,
32,
34].
The intuitive reasoning pathway (system 1) that is used to formulate clinical judgments and decisions is based on the experience and expertise of the clinician, on heuristics, and on pre-determined mental models. The mental representations of a given current clinical situation’s elements and circumstances are matched with previous patterns and knowledge of clinical situations stored in the memory by using a pattern recognition process, and each identified match contributes to the understanding of the current clinical situation; the pre-determined mental models are revised and then adapted to accommodate the given current clinical situation.
However, in the face of deficiencies in prior knowledge and mental models, as is the case with novices and inexperienced clinicians, intuitive reasoning and heuristics may be ineffective in solving clinical problems [
11,
34]. In such circumstances, or when a clinical problem is compound or atypical, the clinician has to employ the deliberate and analytical reasoning pathway of system 2, which is characterized by its time-consuming and complex information-processing operations that require the use of critical thinking, statistical concepts, deductive logic, scientific methods, and focused attention [
33].
5. Emotions as They Relate to Situational Awareness
Emotions may either support or hinder cognitive functioning [
38,
39], and it appears that the emotional state of a clinician may influence whether the gathered situational information will be processed intuitively or analytically [
40]. While a positive affect may support information processing, clinical judgments, and decision making, a negative affect may interfere with sound reasoning, with assessments of the risks of clinical practices, and with weighting the relative clinical importance of situational elements, thus distorting the mental image in SA [
16,
38,
40].
Situational uncertainties and complexities, uncertainty intolerance, worries about inflicting harm to patients, concerns about possible malpractice liability claims, worries about managing a patient’s unrealistic expectations, and a lack of confidence in one’s operational competence are some contextual stressors in clinical practice that may bring about negative emotional responses, such as frustration, anger, agitation, and fear.
Fatigue, financial crisis, poor personal health, and intrinsic or substance-induced negative feelings and moods are some non-contextual stressors that may have a negative impact on SA and clinical practice, and they are not dissimilar to the effects described above with regard to contextual stressors [
14,
16,
38]. Some of these non-contextual negative emotions are incidentally induced, typically persist without conscious awareness (‘carryover incidental emotions’), and may affect subsequent clinical judgments and decision-making processes [
38].
Mental energy is an abstract construct with dynamic properties; it can be viewed as an intrapsychic resource that powers psychological mechanisms including cognition, emotions, motivation, willpower, and executive functioning, all of which are essential for performing goal-directed tasks.
6. Interventions That May Boost the Development of SA
Managing SA errors in clinical practice and reducing their occurrence should not be considered the sole responsibility of clinicians. Both clinician- and organization-directed measures are required to improve clinicians’ ability to develop accurate SA and reduce the risk of SA errors [
14]. Healthcare organizations should introduce, and clinicians should use, health information technology that enables easy access to relevant and up-to-date information, expert second opinions, digital images, clinical guidelines, and algorithms [
16]. The successful integration of bioinformatics, clinical data, and information into relevant knowledge and the effective use of clinical decision support systems and electronic health records may simplify the weighing of diagnostic probabilities and their primacy, and they may bring about essential knowledge that is directly applicable to patient-specific clinical situations [
44].
To boost SA acquisition and avoid SA errors, clinicians should have adequate domain-specific structural knowledge and clinical expertise, and they should master both intuitive and analytical cognitive operations that, in turn, support information processing and clinical reasoning, as well as the identification of common cognitive biases that have a negative impact on the development of accurate clinical SA [
16].
In the context of SA, meditation, mindfulness, and metacognition may enable clinicians to increase their critical awareness and understanding of the complexities of a given clinical situation and to monitor and evaluate their clinical judgments and rational reasoning so that decision making and goal-directed activities can be modified according to the situational dynamics.
7. Conclusions
Situational awareness plays an essential role in the complex and dynamic process of decision making and operational activities in clinical practice. It facilitates the dynamic adaptation of goal-directed plans in response to changing eventualities, and it enables the anticipation of future situational dynamics. Domain-specific experience and expertise and cognitive acuity are essential for developing high-level clinical SA. Situational awareness is susceptible to information overload, cognitive bias, and rapidly changing situational actualities; adequate resources of mental energy are required for its effective development [
5]. In order to acquire the skills necessary to develop accurate SA, clinician trainees have to be repeatedly exposed to simulations of complex and dynamic high-fidelity real-life clinical situations.
This entry is adapted from the peer-reviewed paper 10.3390/healthcare11233098