Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Syncope is a highly prevalent clinical condition characterized by a rapid, complete, and brief loss of consciousness, followed by full recovery caused by cerebral hypoperfusion. This symptom carries significance, as its potential underlying causes may involve the heart, blood pressure, or brain, leading to a spectrum of consequences, from sudden death to compromised quality of life. Various factors contribute to syncope, and adhering to a precise diagnostic pathway can enhance diagnostic accuracy and treatment effectiveness.
- syncope
- transient loss of consciousness
- vasovagal syncope
1. Introduction
The treatment of syncope aims to reduce syncopal recurrences; however, no treatment is completely effective in eliminating syncope episodes in the long term [1]. The underlying physiological mechanism of syncope influences the choice of treatment. For example, bradycardia is the most common cause of cardiac syncope, and it is treated with PM implantation. Nevertheless, the coexistence of hypotension reduces pacing efficacy [1][2]. On the other hand, the management of reflex or orthostatic syncope is more complex since specific therapies are less effective [3]. However, syncopal recurrences often spontaneously resolve after medical evaluation, even without any specific therapy [4].
Syncope tends to recur in less than 50% of patients within 1–2 years, particularly in cases of reflex and orthostatic hypotension syncope [4]. The underlying reason for this decrease is unknown. This implies that treatment may be delayed in low-risk conditions, and caution is warranted when interpreting the effectiveness of interventions in preventing syncope, as observational studies lacking a control group may be biased [4].
2. Treatment of Reflex Syncope
The goal of treating reflex syncope is to enhance the quality of life. Non-pharmacological approaches involve providing reassurance about the benign nature of syncope and encouraging behavioral measures to eliminate or reduce triggers. These measures include avoiding prolonged standing or sitting, rapid changes in position, hot or crowded environments, and engaging in moderate physical activity if tolerated, along with staying hydrated and consuming salted foods. Recognizing prodromes and adopting safe positions or physical counter-pressure maneuvers can significantly reduce syncope recurrence [5].
For cases of recurrent or disabling syncope, therapeutic strategies generally depend on age (younger than 40 years or older than 60 years). Treatment options include adjusting or withdrawing antihypertensive therapy, physical counter-pressure maneuvers (Figure 1, and tilt training [4][5]. Isometric muscle contractions increase cardiac outflow and BP and can potentially delay or prevent syncope events (Figure 1). Tilt training involves gradually increasing periods of orthostatism and may be effective in young, motivated patients with orthostatic stress-induced prodromes, although clear efficacy in clinical studies is not well-established [4][5].
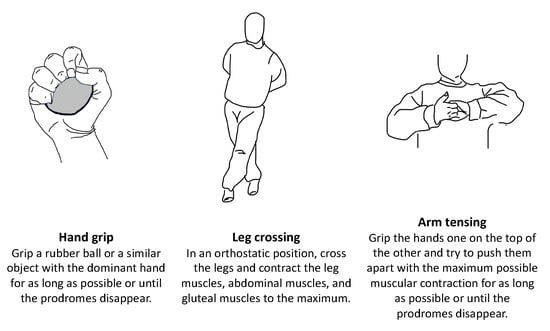
Figure 1. Physical counter-pressure maneuvers.
Pharmacological measures are rarely employed [5][6]. Fludrocortisone increases renal sodium absorption, counteracting the physiological cascade triggering vasovagal reflex syncope. It is recommended at doses of 0.05–0.2 mg/day for young patients without comorbidities and consistently low BP values [4][5]. According to a recent meta-analysis, midodrine, an alpha-agonist acting as a vasoconstrictor, showed a reduction in the recurrence of vasovagal syncope (relative risk (RR) 0.55; 95% CI 0.35–0.85) [6]. Midodrine may be considered at doses of 2.5–10 mg three times a day for young patients with the low BP phenotype experiencing orthostatic-induced reflex vasovagal syncope [4][5].
In the case of a dominating cardioinhibitory response, the implantation of a dual-chamber PM should be considered. PM implantation is indicated in patients over 40 years old. One indication is the evidence on the internal loop recorder of symptomatic asystolic pauses >3 s or asymptomatic pauses >6 s due to sinus arrest or AV block. However, the presence of a concomitant reflex vasodilatory response compromises the efficacy of pacing, resulting in a higher probability of syncopal recurrence. Another indication is a positive tilt test for a cardioinhibitory response and recurrent syncope, although the evidence is controversial. The clinical presentation of syncope itself, along with the absence of concomitant vasodilation and hypotension, is crucial in selecting patients for implantation. Additional tests, such as an internal loop recorder (ILR), are necessary to document the exact mechanism of reflex syncope and determine the appropriateness of pacing. The tilt test, especially when assessing hypotensive susceptibility, is critical for identifying patients who may not effectively respond to pacing, as a positive tilt for hypotensive susceptibility is a strong predictor of PM ineffectiveness [4][7].
Cardioneuroablation (CNA) is gaining recognition for its effectiveness in treating vasovagal syncope. CNA refers to the process of precisely targeting and cauterizing the intrinsic epicardial ganglia within the heart. This results in a partial parasympathetic denervation, decreasing vagal tone on the cardiac fibers, reducing the incidence of bradyarrhythmia [8]. A meta-analysis by Vandenberk et al. on 465 patients aged 18–60 years affected by severely symptomatic recurrent reflex syncope with spontaneous or orthostatic challenge-induced asystole and without sinus node or AV node dysfunction was performed, involving 14 studies [9]. According to their results, the freedom-from-syncope (FFS) after CNA was 91.9% (95% confidence interval (CI) 88.1–94.6%; p = 0.376), with higher rates of FFS for left atrial ablation (94.0%; 95% CI 88.6–96.9%) and biatrial ablation (92.7%; 95% CI 86.8–96.1%) than right atrial ablation (81.5%; 95% CI 51.9–94.7%; p < 0.0001) [9]. A recent study conducted on 48 patients with recurrent syncope showed lower recurrence rates of syncope in the CNA group compared to the non-CNA group [10]. However, despite the promising results, multiple issues arose regarding the selection of potential patients, ideal ablation site, verification of the ablation effect, and long-term durability of the procedure [11][12]. For this reason, further clinical trials and real-world studies encompassing a substantial number of participants with a suitably long follow-up duration are needed.
3. Treatment of Orthostatic Hypotension and Orthostatic Intolerance
The management of orthostatic intolerance syndromes involves reassuring patients about the benign nature of syncope and adopting behavioral measures. Additionally, reducing antihypertensive therapy to achieve a target SBP of 140–150 mmHg is recommended [3][4]. Angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and calcium channel blockers are preferred over beta-blockers and thiazide diuretics. If symptoms persist, further interventions, such as physical counter-pressure maneuvers, elastic stockings, head-up tilt (sleeping with a pillow to prevent nocturnal polyuria, improve fluid distribution, and address nocturnal hypertension), and the use of midodrine and fludrocortisone should be considered [3][4]. Droxidopa, a central and peripheral alpha and beta agonist, was recently approved by the Food and Drugs Administration for the treatment of symptomatic neurogenic OH [13][14]. The main concerns, however, remain for the durability of its benefits [15][16]. Hauser et al. conducted a 12-week open-label study using droxidopa. The study found a notable improvement in the symptoms of neurogenic OH and daily activities compared to the baseline evaluation [17].
4. Treatment of Cardiac Syncope
In sick sinus syndrome, a documented correlation between an ECG and syncope warrants consideration for PM implantation. This recommendation extends to patients experiencing syncope with relief of asymptomatic pauses. PM implantation is also indicated for second- and third-degree AV blocks, bifascicular blocks with a positive EPS, or evidence on the ILR of a paroxysmal AV block. Notably, the guidelines emphasize the importance of an EPS and ILR, as a bifascicular block alone suggests a complete block in less than half of patients, with one-third receiving a final diagnosis of reflex syncope and another third remaining unexplained [4][18].
For patients with paroxysmal supraventricular tachycardia (nodal reentrant tachycardia, AV reentrant tachycardia, atrial flutter, and ectopic tachycardia) and syncope, catheter ablation is recommended as a first-line therapy. The role of antiarrhythmic therapy is limited to the bridging period before ablation or in cases of ablation failure [4][18].
ICD implantation is indicated for syncope due to ventricular tachycardia with an EF < 35% and for syncope in the presence of ischemic heart disease with induced ventricular tachycardia during electrophysiological study. It may be considered in patients with an EF > 35% and recurrent ventricular tachycardia syncope when catheter ablation or medical therapy proves unsuccessful or is not feasible [4][18].
ICD implantation is always recommended in patients with unexplained syncope and dilated cardiomyopathy with an EF < 35%. Consideration for ICD implantation should be provided to patients with unexplained long QT (LQT) syndrome and recurrent syncope (not meeting diagnostic criteria) despite beta-blocker therapy, particularly in LQT2 and LQT3 syndromes, as well as patients with a Brugada type 1 ECG pattern and unexplained syncope [4][18].
In individuals with HCM, the decision for ICD implantation depends on the identification of a high risk of sudden cardiac death using the European Society of Cardiology (ESC) HCM Risk-SCD score. For those at low risk, the implantation of an ILR should be considered instead of an ICD. Lastly, for patients with syncope related to structural heart disease, addressing the underlying cause is essential [4][18].
This entry is adapted from the peer-reviewed paper 10.3390/jcm13030727
References
- Palmisano, P.; Dell’Era, G.; Pellegrino, P.L.; Ammendola, E.; Ziacchi, M.; Guerra, F.; Aspromonte, V.; Laffi, M.; Pimpini, L.; Santoro, F.; et al. Causes of syncopal recurrences in patients treated with permanent pacing for bradyarrhythmic syncope: Findings from the SYNCOPACED registry. Heart Rhythm. 2021, 18, 770–777.
- Van Dijk, J.G.; van Rossum, I.A.; van Houwelingen, M.; Ghariq, M.; Saal, D.P.; de Lange, F.J.; Thijs, R.D.; Sutton, R.; Benditt, D.G. Influence of Age on Magnitude and Timing of Vasodepression and Cardioinhibition in Tilt-Induced Vasovagal Syncope. JACC Clin. Electrophysiol. 2022, 8, 997–1009.
- Fedorowski, A.; Ricci, F.; Hamrefors, V.; Sandau, K.E.; Hwan Chung, T.; Muldowney, J.A.S.; Gopinathannair, R.; Olshansky, B. Orthostatic Hypotension: Management of a Complex, But Common, Medical Problem. Circ. Arrhythm. Electrophysiol. 2022, 15, e010573.
- Brignole, M.; Moya, A.; de Lange, F.J.; Deharo, J.C.; Elliott, P.M.; Fanciulli, A.; Fedorowski, A.; Furlan, R.; Kenny, R.A.; Martin, A.; et al. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur. Heart J. 2018, 39, 1883–1948.
- Aydin, M.A.; Salukhe, T.V.; Wilke, I.; Willems, S. Management and therapy of vasovagal syncope: A review. World J. Cardiol. 2010, 2, 308–315.
- Behnoush, A.H.; Yazdani, K.; Khalaji, A.; Tavolinejad, H.; Aminorroaya, A.; Jalali, A.; Tajdini, M. Pharmacologic prevention of recurrent vasovagal syncope: A systematic review and network meta-analysis of randomized controlled trials. Heart Rhythm. 2023, 20, 448–460.
- Sutton, R.; de Jong, J.S.Y.; Stewart, J.M.; Fedorowski, A.; de Lange, F.J. Pacing in vasovagal syncope: Physiology, pacemaker sensors, and recent clinical trials-Precise patient selection and measurable benefit. Heart Rhythm. 2020, 17, 821–828.
- Pachon, J.C.; Pachon, E.I.; Pachon, J.C.; Lobo, T.J.; Pachon, M.Z.; Vargas, R.N.; Jatene, A.D. “Cardioneuroablation”--new treatment for neurocardiogenic syncope, functional AV block and sinus dysfunction using catheter RF-ablation. Europace 2005, 7, 1–13.
- Vandenberk, B.; Lei, L.Y.; Ballantyne, B.; Vickers, D.; Liang, Z.; Sheldon, R.S.; Chew, D.S.; Aksu, T.; Raj, S.R.; Morillo, C.A. Cardioneuroablation for vasovagal syncope: A systematic review and meta-analysis. Heart Rhythm. 2022, 19, 1804–1812.
- Pachon, M.J.; Pachon, M.E.; Pachon, C.T.C.; Santillana, P.T.; Lobo, T.J.; Pachon, M.J.; Higuti, C.; Zerpa, A.J.; Pachon, M.Z.C.; Ortencio, F.A.; et al. Long-term outcomes of cardioneuroablation with and without extra-cardiac vagal stimulation confirmation in severe cardioinhibitory neurocardiogenic syncope. J. Cardiovasc. Electrophysiol. 2024, 42, 821–829.
- Brignole, M.; Aksu, T.; Calo, L.; Debruyne, P.; Deharo, J.C.; Fanciulli, A.; Fedorowski, A.; Kulakowski, P.; Morillo, C.; Moya, A.; et al. Clinical controversy: Methodology and indications of cardioneuroablation for reflex syncope. Europace 2023, 25, euad033.
- Sheldon, R.S.; Raj, S.R. Cardioneuroablation for vasovagal syncope: Sober second thoughts. Heart Rhythm. 2023.
- Elgebaly, A.; Abdelazeim, B.; Mattar, O.; Gadelkarim, M.; Salah, R.; Negida, A. Meta-analysis of the safety and efficacy of droxidopa for neurogenic orthostatic hypotension. Clin. Auton. Res. 2016, 26, 171–180.
- Kaufmann, H.; Norcliffe-Kaufmann, L.; Palma, J.A. Droxidopa in neurogenic orthostatic hypotension. Expert. Rev. Cardiovasc. Ther. 2015, 13, 875–891.
- Biaggioni, I.; Arthur Hewitt, L.; Rowse, G.J.; Kaufmann, H. Integrated analysis of droxidopa trials for neurogenic orthostatic hypotension. BMC Neurol. 2017, 17, 90.
- Amjad, F.; Polenchar, B.; Favit, A. Droxidopa Persistence in Neurogenic Orthostatic Hypotension May Be Affected by Titration Approach. Int. J. Gen. Med. 2021, 14, 4485–4490.
- Hauser, R.A.; Favit, A.; Hewitt, L.A.; Lindsten, A.; Gorny, S.; Kymes, S.; Isaacson, S.H. Durability of the Clinical Benefit of Droxidopa for Neurogenic Orthostatic Hypotension During 12 Weeks of Open-Label Treatment. Neurol. Ther. 2022, 11, 459–469.
- Francisco Pascual, J.; Jordan Marchite, P.; Rodriguez Silva, J.; Rivas Gandara, N. Arrhythmic syncope: From diagnosis to management. World J. Cardiol. 2023, 15, 119–141.
This entry is offline, you can click here to edit this entry!
