Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Dentistry, Oral Surgery & Medicine
The speed of progress in the evolution of digital dental manufacturing has become truly remarkable. Subtractive methods have achieved remarkable levels of both efficiency and precision in achieving accurate fits, while additive techniques such as 3D printing are gaining prominence at an escalating rate.
- 3D printing
- prosthodontics
- additive manufacturing
- polymers
- digital
- prosthetic restorations
1. Introduction
The advent of industrial-scale additive manufacturing, more commonly known as 3D printing, saw its initial appearance on the market during the early 1980s [1]. Visionaries in the realm of 3D printing include notable figures like Charles W. Hull (the visionary behind 3D Systems), S. Scott Crump (the mind behind Stratasys), and the pioneering duo of Hans J. Langer and Hans Steinbichler (the founders of EOS). It was Charles W. Hull who obtained the patent for the first 3D printer in 1986 [2]. In their nascent phase, these 3D printers primarily found their utility in the domain of rapid prototyping [3,4].
Nevertheless, the evolution of this technology surged forward with remarkable speed in the subsequent years [5]. Notably, the expiry of the patent for the fused deposition modeling (FDM) process in 2009 propelled 3D printers into the realm of consumers, catalyzing a significant penetration into this sector [6,7]. This transformative momentum extended its influence into the realm of dentistry as well [8]. The dimensions of printing units shrank while costs diminished, resulting in an altered landscape of applicability [9,10]. Simultaneously, the gamut of printable materials broadened to encompass a diverse array, ranging from plastics and metals to ceramics and even biological tissues [11]. These rapid prototyping methods can be classified based on the specific types of materials employed, such as plastics, metals, or powders [12,13].
Additive manufacturing (AM) procedures involve the step-by-step creation of items according to three-dimensional models [3]. The phrase commonly employed interchangeably with all additive techniques is 3D printing. As per the EN ISO/ASTM 52900:2021 standard for terminology, an AM process is defined as the “procedure of combining materials to construct objects using 3D model data, typically layer by layer, in contrast to subtractive manufacturing techniques” [9].
The speed of progress in the evolution of digital dental manufacturing has become truly remarkable [14]. Subtractive methods have achieved remarkable levels of both efficiency and precision in achieving accurate fits, while additive techniques such as 3D printing are gaining prominence at an escalating rate [15]. The merging of various manufacturing approaches, such as the pairing of laser sintering with CNC machining, or the integration of digital design and 3D printing alongside traditional analog pressing, vividly showcases the immense possibilities that lie ahead [16,17].
Societal shifts are exerting transformative influences on the field of dental technology, much like they do in other sectors [18]. One of these profound changes pertains to a scarcity of a proficient workforce. Notably, there is an ongoing decline in the number of individuals pursuing training in dental technology [19], even as the demand for dental prostheses continues to surge due to shifting demographics [8]. Furthermore, patients are increasingly constrained by time limitations prompted by heightened expectations in their professional spheres, curtailing their capacity to undergo dental procedures [20].
In the face of these challenges, the digital revolution emerges as a potential solution, as digital procedures often stand out for their efficiency [21]. Within the dental laboratory, the integration of digital processes offers advantages like heightened precision and reproducibility, alongside enhanced material characteristics and user convenience [22]. This technological transition holds the potential to address these challenges by harnessing the inherent efficiencies of digital methodologies [23,24].
The intriguing fusion of a digitalized work environment and a hands-on artisanal craft renders dental technology a compelling choice for young individuals seeking a diverse and multifaceted professional journey [25]. Numerous dental laboratories have adeptly embraced the delicate equilibrium between preserving age-old craftsmanship and embracing the digital realm, finding harmony between tradition and disruption, and reconciling established values with the need for necessary changes [26,27]. Within this unfolding narrative, the role of 3D printing as a digital manufacturing process takes center stage, illuminating a pivotal facet of this evolution [28]. To put it in simplified terms, the workflow involves a dental technician generating a digital dataset on a computer and creating a three-dimensional entity through computer-aided design (CAD) [29]. This digital blueprint is then transmitted to a 3D printer, where it metamorphoses into a tangible object [30].
An inherent advantage of additive manufacturing techniques lies in their capacity to visualize and actualize three-dimensional concepts on a screen, enabling the realization of a virtually boundless array of forms and intricacies [31]. An intriguing facet often overlooked is that the mechanical and aesthetic attributes of the fabricated item can be subtly tailored during the 3D construction process [32]. This distinct capability is absent in subtractive manufacturing, wherein the material characteristics are predetermined by the supplier of the prefabricated material [33,34]. The confluence of customization opportunities and the expeditious availability of digitally conceived items, often at reduced costs, positions additive manufacturing as a pivotal cornerstone within the realm of digital dentistry [35,36].
Polymeric materials play a significant role in the realm of dentistry, offering a wide array of applications stemming from their distinct surface qualities, mechanical and biological attributes, simplified processing, and cost-effectiveness [4]. Among the frequently employed polymers in dental applications are polymethyl methacrylate (PMMA), polyurethane (PU), polyethylene (PE), polycarbonate (PC), polyetheretherketone (PEEK), polyethylene glycol (PEG), polydimethylsiloxane (PDMS), polylactic acid (PLA), poly(e-caprolactone) (PCL), acrylonitrile butadiene styrene (ABS), and polypropylene (PP) [2].
While their mechanical traits are linked to the inherent properties of the bulk material, their interaction with oral tissues heavily relies on surface characteristics. This justifies the utilization of polymer coatings to enhance their biocompatibility [7]. The applications of these polymers span nearly all sectors of dentistry, encompassing direct restorative procedures, prosthodontics, orthodontics, and even implantology. Notably, synthetic PEEK has emerged as a potential implant material [15]. Leveraging 3D printing, intricately detailed custom facial prostheses made from polymers can be readily produced [26]. Furthermore, polymers have been instrumental in crafting scaffolds that contribute to bone structure regeneration, along with the development of tissues resembling dentin and pulp. They also find utility in producing membranes for guided tissue regeneration and as carriers for drug delivery in the treatment of various oral and periodontal conditions [21].
2. General Techniques for 3D Printing in Prosthetic Dentistry
Among the various dental specialties, prosthodontics appears to have reaped substantial benefits from the advancements in 3D-printing technology. This is particularly evident in both fixed and removable denture fabrication, which can now be seamlessly executed through a fully digital workflow, resulting in precise and well-fitting prostheses. Polymers have proven to be well-suited for additive manufacturing processes involved in creating temporary crowns, denture bases, and artificial teeth. There have even been efforts to explore the 3D printing of polymeric permanent crowns and bridges. The range of applications of 3D-printed polymers in prosthodontics extends to crafting custom trays, patterns, try-ins, dental bite registrations, and various types of models. Several frequently employed polymers in the field of prosthetic dentistry include polymethylmethacrylate (PMMA), polylactic acid (PLA), polyetheretherketone (PEEK), and acrylonitrile butadiene styrene (ABS). Their molecular structures and general applications in the prosthodontic field are presented in Figure 2 and Figure 3.
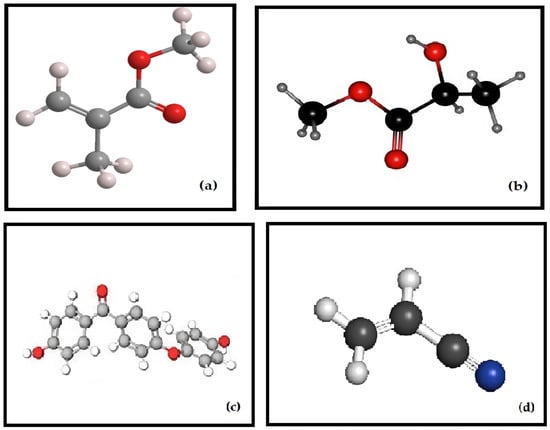
Figure 2. Molecular structures of the polymers for 3D Printing in Prosthodontics—(a) PMMA; (b) PLA; (c) PEEK; (d) ABS.
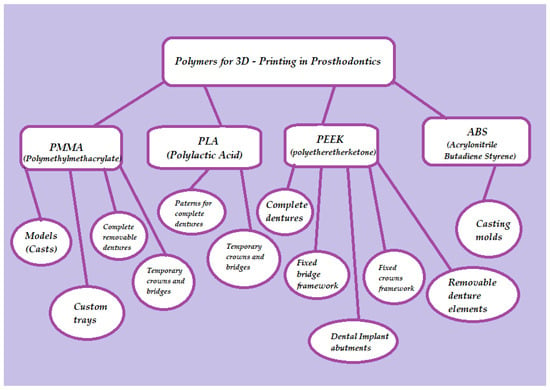
Figure 3. Three-dimensional-printed polymers used in prosthetic dentistry and their application.
Multiple 3D printing methods are available for the additive fabrication of prosthetic restorations (Figure 3, Figure 4 and Figure 5).
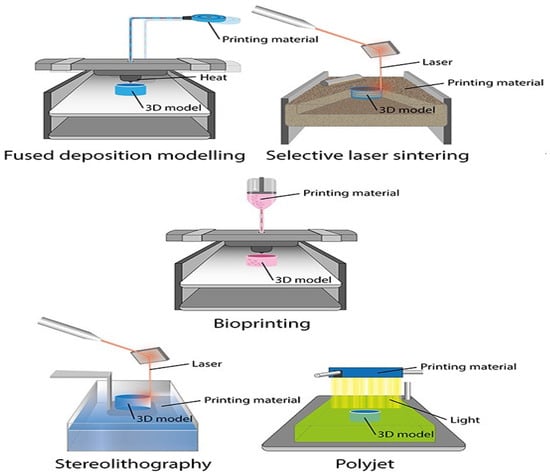
Figure 4. Application of 3D printers in dentistry.
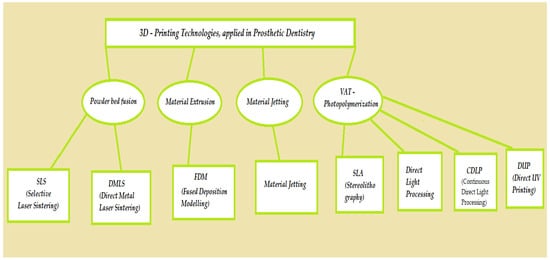
Figure 5. Three-dimensional-printing technologies, applied in prosthetic dentistry.
When these methods are juxtaposed, they reveal distinct attributes, encompassing speed, precision, scale, and procedural stability, contingent upon the underlying technology employed [37,38]. At present, within the domain of prosthetic dentistry, stereolithographic techniques emerge as the prevailing choice [39]. These encompass conventional stereolithography, laser-based solidification (stereolithography, SLA), and mask exposure methods (digital light processing, DLP). In both these methodologies, the object is solidified within a reservoir of photopolymer through the influence of light [40,41].
Starting in 2018, an array of 3D printers has entered the market that utilizes economical liquid crystal displays (LCD) [42]. This technology is termed direct ultraviolet printing (DUP) and exploits the LCD screens for precise pixel-wise exposure of the construction platform [43]. The typical choice for illumination is UV LEDs within a wavelength range of 395 to 405 nm. Moreover, direct 3D printing processes, also known as material jetting (MJT), have found application within dental contexts. Notably, there is a noteworthy technique known as multi-material 3D printing by Stratasys, which enables the simultaneous processing of diverse colors and materials with varying properties in a single build [5,44].
However, within the dental field, material extrusion (MEX) processes, including techniques such as fused-filament fabrication (FFF) or fused deposition modeling (FDM), currently face drawbacks as indicated by recent findings [45]. This is attributed to the extended printing times and challenges in attaining higher resolutions associated with these processes [46]. Among the diverse technologies mentioned within the realm of plastics, it is apparent that SLA, DLP, and MJT stand out as particularly compelling from both a technical and economic perspective [47,48]. Table 1 presents the most commonly used polymer materials in prosthodontics, organized according to their processing and their properties (Table 1).
Table 1. Three-dimensional-printed polymers, systemized by processing method and characteristics.
| Type of Polymer | Processing Method | Characteristics |
|---|---|---|
| Methacrylic Acid (Formlabs: Dental SG) | Stereolithography | Elastic Modulus: 1670 MPa; Orientations of 0° to 90°. |
| Polylactic acid (PLA) | Fused deposition modeling | Tensile Strength: 28–56 Mpa; Elastic Modulus: 2000 Mpa; Orientations of 0° to 90° |
| Polyether ether ketone (PEEK) | Fused deposition modeling | Tensile Strength: 58–85 Mpa Elastic Modulus: 3000–4100 Mpa; |
| Acrylonitrile butadiene styrene (ABS) | Fused deposition modeling | Tensile Strength: 27–31 Mpa; Layer height: 0.05–0.14 mm; Processed at 210–240 °C. data |
The pioneering 3D printing systems to enter the market were stereolithographic setups that employ laser beams to solidify liquid substances [49]. Charles Hull, as early as the 1980s, filed a patent application for the initial stereolithography printer [50]. In their initial iterations, these devices were notably extensive and came with a high price tag [51]. In contrast, the latest wave of stereolithographic printers has become significantly more cost-effective. For the past five years, Formlabs (Sommerville, MA, USA) has provided a 3D printer tailored for dental applications [52]. This budget-friendly system serves as an excellent point of entry into 3D-printing technology, although it should be noted that the printing process might take longer compared to DLP printers [53,54].
In conjunction with stereolithography, digital light processing (DLP) stands out as one of the most widely adopted additive manufacturing methods within the current dental domain [55]. The configuration of a DLP printer closely resembles that of an SLA printer, with the primary distinction being the source of illumination utilized [56,57]. Unlike the SLA printer that employs a laser beam for curing the photopolymer, DLP printers employ projection technology developed by Texas Instruments [58]. In this method, short-wavelength light (currently operating at wavelengths of 380 nm and 405 nm) is directed through a central digital micromirror device (DMD), which constitutes the core of DLP technology [59,60]. This setup employs micro mirrors with an approximate edge length of 16 µm that can be individually tilted under the influence of electrostatic forces, enabling the light to be optically directed onto the build platform [61]. This platform is situated within a translucent reservoir of photopolymer (also known as a photopolymer bath), or onto an absorptive surface [62,63]. The light, channeled through the DMD, projects the exposure mask onto the build platform through an optical lens. This prompts the photopolymer to solidify in the exposed regions [64]. After each mask projection, the build platform ascends along the z-axis, allowing fresh material to flow into the area beneath the object, thereby preparing it for exposure with the next mask [65,66]. In the realm of DLP technology, the time required for fabrication is predominantly determined by the object’s dimension along the z-axis, rendering it relatively independent of the object’s overall complexity or geometry [67].
In DLP (digital light processing) printers, the process involves using tiny mirrors to create individual image points or pixels [68]. However, the number of these micromirrors on a DMD (digital micromirror device) is limited. This limitation becomes evident when enlarging the build platform, which consequently increases the lengths of the edges along the x and y axes [69,70]. This expansion results in reduced precision. Despite this challenge, there are three methods currently employed to achieve larger build platforms. Inexpensive DLP printers utilize DMD chips with lower resolutions, leading to a smaller physical size. By using high-resolution DMD chips (e.g., HD 1920 × 1080 pixels), greater object accuracy can be attained without increasing the printer’s footprint [71]. Even more impressive, the use of 4K DMD chips (3840 × 2160 pixels) enables the combination of high resolutions with a sizable build area, as seen in the Rapid Shape D70+ printer. However, the cost of 4K DMD chips remains a significant obstacle.
The approach of running two DLP projectors with HD resolution in parallel results in a seam or “joint” on the build platform due to the utilization of two light sources. This joint prevents the printing of objects that span the projection field. For instance, the Rapid Shape D40 II printer employs this method [72]. To enhance the capabilities of DLP printers, innovations are applied in detaching objects from the material vat during the build process (W2P Engineering, Vienna, Austria). This detachment occurs after each cycle of exposure when the build platform is raised along the z-axis [73]. Four distinct techniques are employed to achieve these fixed intervals. The build platform follows a predefined path within a specific timeframe after each exposure cycle. This approach maintains a consistent path-to-time ratio throughout the build process, even if fewer support structures could allow for earlier detachment. While straightforward, this method does not alter the overall duration of the building processes [74].
Force sensors are utilized to measure the detachment force required (Rapid Shape, Heimsheim, Germany). Smart control technology calculates an optimal path-to-time ratio, thus accelerating the building process. An important benefit is the precise and controlled separation process. The patented Force Feedback technology is exemplified in printers like the Rapid Shape D30 [75].
Vat Deflection Feedback System (VDFS; W2P, Vienna, Austria) employs an additional sensor to expedite the building process. By allowing the deformation of the material tray (FlexVat), the detachment force is minimized. This leads to heightened printing speed and quality [76].
Carbon3D (CDLP; Carbon3D, Redwood City, CA, USA) introduced the patented continuous liquid interface production (CLIP) technology, categorized as a CDLP process. Unlike the step-by-step object buildup in conventional DLP printers, CLIP employs a continuous build process that does not necessitate the usual detachment steps. This is achievable due to an oxygen-rich zone (“dead zone”) immediately above the build platform, where the photopolymer does not cure. Oxygen is introduced into this zone through an oxygen-permeable window [77]. As adhesion between the object and the build platform is absent, a continuous build process becomes feasible. The outcome is rapid build speeds, precise object formation, and uninterrupted object geometries along the z-axis. Examples of dental applications encompass digitally manufactured Lucitone Digital Print denture bases from Dentsply Sirona (York, PA, USA), as well as bite splints produced using Carbon3D printers like KeyPrint and KeySplint Soft Clear [78].
DLP projectors that move underneath the material vat can expose a larger area for printing. A key advantage of this approach is the absence of a joint line on the printed object. As a result, the entire build platform can be used at full resolution, leading to higher precision, increased printing accuracy, and optimal utilization of the printer’s capacity [79].
MovingLight (Prodways Group, Paris, France) is a technology based on the DLP process but stands out due to its dynamic projector movement. Unlike its competitors, the projector is not fixed in a single position within the printer; instead, it moves across the entire working area in multiple steps [80]. This innovative movement results in high resolutions (42 µm) and remarkable accuracy, even with a substantial build platform. Examples of printers utilizing this technology include Prodways’ ProMaker LD10 Dental Plus, LD10 Dental Models, LD20 Dental Plus, and LD20 Dental Models. The latter two models incorporate two movable projector heads, reducing printing times by an additional 40%. For instance, these printers can produce 55 dental arches in approximately 1 h [81,82].
Another approach is the material jetting technique, in which the material is deposited directly onto the build platform using a print head, resembling the process of 2D printing. Following this deposition, the material undergoes curing during an intermediate exposure step, gradually constructing the object layer by layer. The most prominent example of this approach is the Polyjet method, developed by Stratasys in Eden Prairie, MN, USA [83]. This method is characterized by its rapid building process and remarkable precision. Notably, it supports multi-material 3D printing, allowing for the creation of objects using up to five distinct materials in a palette of over 500,000 colors. Stratasys offers products like the J720 Dental and J750 Digital Anatomy printers, both capable of operating in multi-material and multicolor modes [84].
At present, polymers stand as the predominant choice for 3D printing within the dental field. They are employed to create both permanent and removable dentures, along with a diverse array of dental devices, dental implants, and tissue formations.
This entry is adapted from the peer-reviewed paper 10.3390/polym15234525
This entry is offline, you can click here to edit this entry!
