1. Epidemiology and Pathophysiology
KS is considered a relatively rare condition, and its true prevalence is not well established due to under-recognition and under-reporting [
6].
Recent reports suggest that KS has been observed across all races, age groups (from 2 to 90 years old), and geographic locations. It has mostly been reported in Southern Europe, particularly in Turkey, Greece, Italy, and Spain [
6]. This geographical variation may be attributable to physician awareness, climate, environmental conditions, overconsumption of medicines, or inadequate preventative measures. An example is the district of Achaia, Greece, where 52 cases were reported in the last 4 years, resulting in an estimated annual incidence of 4.33 cases per 100,000 inhabitants [
6].
In a prospective study lead by Akoz et al. [
8], it was found that out of 138.911 patients admitted to the emergency department in one year, 793 presented with allergy complaints. The incidence of KS among all admissions and allergy patients was 19.4 per 100,000 (27/138.911) and 3.4% (27/793), respectively.
Between 2010 and 2014, 51 cases of KS were reported to the International Pharmacovigilance Agency, with almost half occurring in 2014 [
9].
In a retrospective study lead in the Swiss Canton [
10], the incidence of anaphylaxis with circulatory symptoms was estimated over a 3-year period, revealing 246 episodes in 226 individuals, with an incidence of 7.9–9.6 per 100,000 inhabitants per year. The case–fatality rate was 0.0001%, with three reported deaths.
Various causes can trigger KS, such as foods, medications (i.e., antibiotics, nonsteroidal anti-inflammatory drugs, contrast media), and environmental factors, including insect bites [
6,
9,
10] (
Figure 1). It is also important to underline how some antiblastic drugs, such as those used for molecular target therapy and immune checkpoint inhibitors, are considered capable of inducing vasospastic angina too [
11].
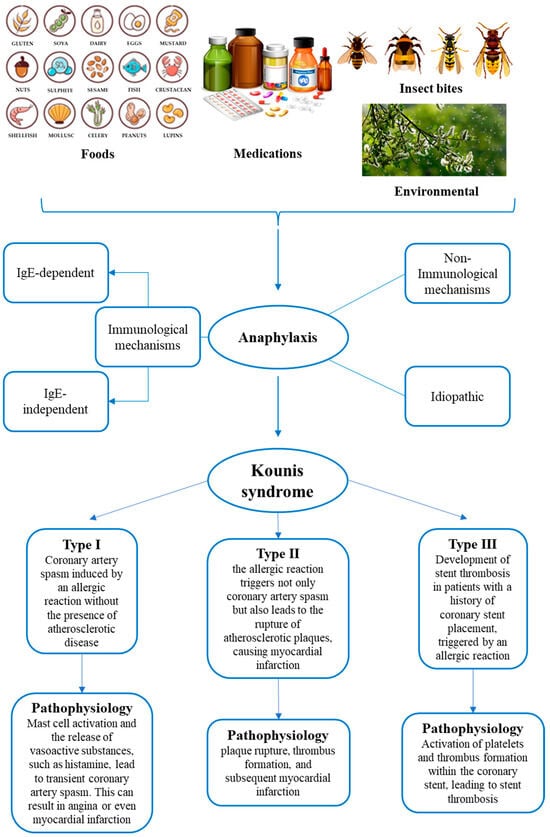
Figure 1. Summary of the main triggering factors of anaphylaxis, pathophysiological mechanisms of anaphylaxis, and types of Kounis syndrome.
The pathophysiology of KS involves a complex interplay between allergic or hypersensitivity reactions and the cardiovascular system. The pathophysiological mechanisms of anaphylaxis can be distinguished as immunological (IgE-dependent and IgE-independent, respectively), non-immunological, and idiopathic [
12]. The main molecular mechanism is the allergic IgE-mediated reaction, which involves mast cells and basophils, responsible for the release of inflammatory mediators in systemic circulation. The non-IgE-mediated reaction, called anaphylactoid, is based on IgG and IgM immune complexes activation. Then, there are cases in which a non-immunological mechanism is described, where a direct degranulation of mast cells and basophils occurs. Finally, in idiopathic anaphylaxis, no triggering causes can be identified.
The most reported pathophysiological mechanisms of KS consist of coronary vasospasm, platelet activation, aggregation, and platelet-dependent arterial smooth cell hyperplasia [
13], determined by allergic inflammatory mediators. Particularly, alterations in sympathetic and parasympathetic neural transmission, local arterial metabolic abnormalities, extensive responsiveness of the medium-sized arteries to circulatory vasoactive amines, or a combination of these factors have been described as potentially responsible for the onset of coronary spasm [
14]. Moreover, the presence of mast cells in the culprit lesion, especially if complicated by plaque erosion or rupture, can be identified in acute coronary syndrome due to allergic events [
15]. Mast cells activation is responsible for the degranulation of vasoactive mediators (i.e., histamine, chemokine, tryptase, chymase, cathepsin-D, heparin, proteoglycans, and cytokines), which are then released into local and peripheral circulation, determining vasoconstriction [
16]. Among these mediators, histamine induces both coronary vasoconstriction and platelet activation, with coronary thrombosis [
17].
KS can manifest in various ways, ranging from angina to acute myocardial infarction. The specific presentation may depend on factors such as the type and severity of the allergic reaction, individual patient characteristics, and the presence of pre-existing cardiovascular conditions [
6].
Understanding the pathophysiology of KS is crucial for appropriate diagnosis and management. Treatment often involves addressing the underlying allergic reaction, managing coronary artery spasm, and providing supportive care for cardiovascular events. To facilitate this, a classification system for KS has been provided [
4,
6]. Of the three existent types, each one presents different pathophysiology characteristics and clinical assessment, but there can be an overlap between the types, so individual cases may not fit into one specific category. It is important to note that these classifications provide a framework for understanding the different clinical scenarios associated with KS [
6,
20]. Type I variant, also known as vasospastic allergic angina or MINOCA (myocardial infarction with nonobstructive coronary arteries) type, usually develops in subjects with no atherosclerotic phenomena in coronary arteries and with no other risk factors, manifesting itself with endothelial dysfunction or microvascular angina: the releasing of the inflammatory mediators typical of anaphylaxis could cause coronary spasm with no cardiac enzyme alterations or myocardial infarction, leading to death in the most severe cases [
6,
20]. The type II variant is instead an allergic acute myocardial ischemia which develops in subjects suffering from coronary atherosclerosis: the release of inflammatory mediators can determine transient events characterized by coronary spasms with normal cardiac enzymes up to the rupture of plaques and death [
6,
20]. Lastly, the type III variant occurs in patients with coronary stents, at which occur thrombotic phenomena secondary to the onset of the anaphylactic phlogistic phenomena. There are two subtypes in the Type III variant, stent thrombosis (subtype IIIa) and/or stent restenosis (subtype IIIb). In these cases, it is possible to detect eosinophils and mast cells on histological examinations performed after autopsy [
6,
20]. The three main types are reported in
Figure 1. These classifications help in understanding the diverse ways in which the syndrome can manifest and, therefore, be treated.
2. Postmortem Assessment of Kounis Syndrome
The postmortem assessment of anaphylactic death is considered a challenge because the evidence emerging from autopsy and histology is not pathognomonic. The diagnosis should be based on the integration of circumstantial and anamnestic data, autopsies, histological findings, and biochemical and immunohistochemical data [
26,
27]. This approach has a pivotal role also in those cases where the occurrence of KS is suspected after analyzing the anaphylaxis effectors in the biological fluids and in common target tissues, together with heart and coronary arteries [
28].
Anaphylactic deaths are often related to a combination of factors, including upper airway obstruction from mucosal edema, asphyxia from bronchospasm, and shock due to massive fluid shifts [
26]. Thus, at postmortem evaluation, the main gross findings can be observed in the respiratory system, where the presence of laryngeal edema, tracheo-bronchial hypersecretion of mucus and mucosal edema with lumen obstruction, and pulmonary edema can support the occurrence of anaphylaxis [
27]. Histological analysis provides the confirmation of these macroscopic data and, also, can show other signs such as bronchospasm, emphysema, and acute pulmonary edema [
26]; then, an important finding, strongly related to anaphylaxis, is leukocyte infiltration, mostly mediated by basophils, eosinophils, and mast cells [
23].
In cases with KS occurrence suspicion, histological examination of the heart and coronary arteries is strongly recommended. For this purpose, the use of different histological stains can highlight the presence of different inflammatory cells involved in allergic reactions. In fact, eosinophils and mast cell infiltrates are identified using hematoxylin–eosin and Giemsa (or toluidine blue) staining, respectively [
29,
30].
In KS manifesting as coronary spasm, a high presence of mast cells has been found in the coronary arteries wall, including the area of the spasm, especially in the tunica adventitia [
29,
30,
31,
32,
33]. Furthermore, many studies report that the major count of mast cells is concentrated in atherosclerotic and hemorrhagic plaques [
28,
29]. Histologically, myocardial alterations caused by the ischemic insult related to the compromission of coronaries due to heart anaphylactic involvement can be observed. In fact, when death occurs within a short period of time from ischemia onset, it is possible to find signs such as myofiber eosinophilia, elongation of sarcomeres and nuclei, wavy fibers, interstitial oedema, and contraction band, suggesting the occurrence of a so-called early myocardial ischemia [
34,
35]. Kitulwatte et al., reported the presence of transmural contraction band necrosis together with consistent inflammatory cell infiltrates [
27].
However, since these findings cannot be considered pathognomonic, other analyses, such as biochemistry and immunohistochemistry, can contribute to performing the postmortem diagnosis of anaphylaxis and KS [
26].
Biochemical investigations are described in many studies as a useful tool for the postmortem assessment of anaphylaxis, with a particular attention paid to the measurement of serum tryptase and IgE. Serum tryptase is the most used biomarker of anaphylaxis and is a very stable enzyme, being detectable up to 6 days after death [
26,
28]. However, since postmortem degradation processes can lead to a reduction in the effective concentration of tryptase as the postmortem interval (PMI) increases, in case of suspected anaphylactic death, it is suggested that a blood sample is taken as soon as possible [
26]. Various cut-offs for serum tryptase levels from peripheral blood have been reported in the forensic literature. As reported by Kounis et al. [
28], a level of tryptase of 10 µg/L or greater has a sensitivity of 86% and specificity of 88% for the diagnosis of postmortem anaphylaxis. Tse et al. and Edston et al. [
36,
37] proposed a tryptase cut-off value ≥ 53.8 µg/L and 45 µg/L on femoral blood, respectively. The latter one can be considered to be a new limit value [
36,
37]. However, if blood is collected from central vessels, such as the aorta, the suggested threshold value is 110 µg/L [
38], which is higher than previous ones, since some factors, such as prolonged cardiac massage or defibrillation, are responsible for an increase in mast cell degranulation and in tryptase levels due to visceral trauma from chest compressions [
39]. Therefore, peripheral blood is preferable to central blood for postmortem tryptase determination [
40,
41]. However, even in the case of peripheral blood, in forensic practice, it is necessary to highlight that some factors can influence the tryptase concentration (i.e., hemolysis and duration of the agonal period). Furthermore, increased tryptase levels have also been described in non-anaphylactic deaths [
27,
28], such as sudden infant death syndrome, acute deaths after heroin injection, traumatic deaths, and asphyxia.
A total and specific IgE assay in postmortem serum can provide data on anaphylaxis occurrence, demonstrating atopic disposition and the degree of sensitization to a particular allergen [
26,
27]. Some studies argue that serum IgE measurement provides approximate data due to the short half-life and lack of a cut-off value for the differential diagnosis of anaphylaxis from other allergic diseases (i.e., asthma) [
42]. Nevertheless, integrating the results of these analyzes with serum tryptase levels can still provide useful information on the cause of death.
In suspicion of KS, the evaluation of these serum analytes should be performed and integrated thorough the analysis of others anaphylaxis-related substances (such as carboxypeptidase A and histamine) and specific IgE in the pericardial fluid. Specifically, an increased concentration of carboxypeptidase A, secreted by mast cells, has been found in both postmortem serum and the pericardial fluid of subjects who died from anaphylaxis [
28].
Moreover, since KS can cause coronary vasospasm or coronary thrombosis up to early myocardial ischemia or infarction, a further useful biochemical investigation consists of the measurement of serum troponin I levels to evaluate cardiac damage and to support its postmortem diagnosis [
43].
Immunohistochemistry is another useful investigation for a more effective postmortem diagnosis of anaphylaxis, although it is important to underline that the identification of mast cells in tissues cannot be considered sufficient to make a diagnosis of certainty. Indeed, an increased number of mast cells can be detected also in various biological processes (i.e., tissue remodeling, angiogenesis, fibrosis, and asphyxia) and in non-anaphylactic deaths. The main effectors of inflammation during anaphylaxis (i.e., eosinophils, basophils, but above all mast cells) have been found in tissues, as bronchial, respiratory, and intestinal mucosa, red pulp of the spleen, and connective tissue (i.e., cutaneous and perivascular) [
26,
30,
33].
A research group immunohistochemically analyzed eosinophil and basophil infiltrations using, respectively, major basic protein (MBP) and proMBP1 antibodies [
44]. These markers may also be used to detect specific cell infiltration in myocardial tissue to better define heart anaphylactic involvement and then to support KS occurrence.
Mast cells are the main effectors of anaphylaxis and are frequently immunohistochemically detectable in many tissues, such as respiratory and spleen, using anti-tryptase antibodies [
42]. These inflammatory cells are a very useful KS assessment, having been observed in myocardial tissue and coronary arteries [
28]. Increased numbers of mast cells in the three layers of the coronary arteries and myocardial cellular infiltrates of neutrophils with mast cells and eosinophils have been detected in patients who died because of coronary spasm. Therefore, during anaphylaxis, pericardial tissue may also be involved, in which histological examination has revealed perivascular areas of infiltration of lymphocytes, macrophages, neutrophils, and mast cells [
7,
28]. These findings suggest that, in KS, myocardial damage seems to be related to the effect of both mast cell degranulation and the release of inflammatory mediators that affect the cardiovascular system (i.e., coronary vasoconstriction induced by histamine). Thus, a diagnosis should be made mainly using the immunohistochemical evaluation of degranulated tryptase in coronary walls and myocardial tissue [
26,
38,
45,
46,
47,
48]. Moreover, some studies also reported the analysis of chymase, representing another marker for mast cells detection [
38,
48]. In particular, Del Duca et al., reported that in some samples, it is possible to identify anti-chymase positive mast cells in perivascular spaces [
49]. Therefore, these data could be useful for an even more correct identification of KS. A further diagnostic method is represented by anti-CD117, a specific indicator of the activation of the cKIT receptor tyrosine kinase, required for mast cell maturation. Therefore, anti-CD117 may be used to detect the activated tissue mast cells also in myocardial tissue and coronaries [
45,
46,
47].
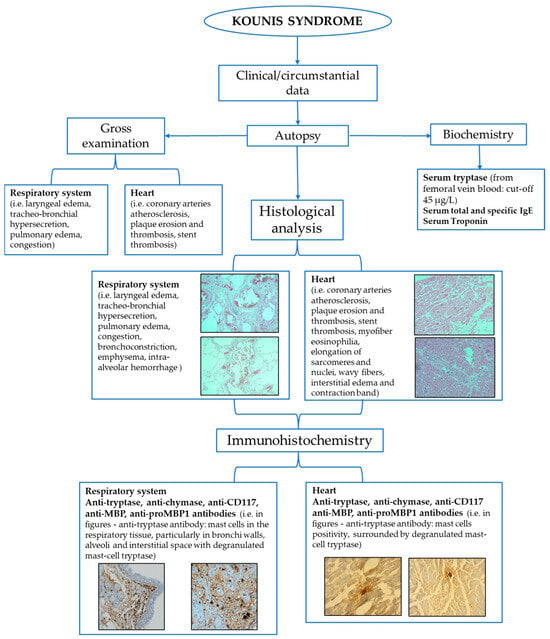
A schematic summary of the main investigations to reach the postmortem diagnosis of Kounis syndrome is reported in Figure 2.
Figure 2. Flow-chart of the main tools for postmortem assessment of Kounis syndrome.
This entry is adapted from the peer-reviewed paper 10.3390/life14010091