|
Trial/Reference
|
Design
|
Primary Endpoint
|
Number of Patients
|
Patients Enrolled
|
Response
|
Outcomes
|
Early Mortality
|
|
daunorubicin
+ cytarabine
+ venetoclax
(DAV)/[17]
|
phase II
|
composite complete remission rate
|
36
|
patients aged 18–60 years
|
CRc 6 rate: 91%
|
estimated 1-year OS 11: 97%
estimated 1-year EFS 12: 72%
|
30-day mortality: 0%
|
|
daunorubicin
+ cytarabine
+ venetoclax
(DAV 2 + 6)/[18]
|
phase II
|
overall response rate
|
42
|
patients aged 16–60 years
|
ORR 7: 92.9%;
87.9% of the CR 8 patients with undetectable MRD 9
|
estimated 12-month OS 11: 83.1%
estimated 12-month EFS 12: 82.7%
estimated 12-month DFS 13: 92%
|
30-day mortality: 2.4%
|
|
daunorubicin
+ cytarabine
+ venetoclax
(5 + 2 + VEN)/[19]
|
phase Ib
|
optimal dose schedule of venetoclax with
5 + 2
|
69
|
patients aged ≥65 years with de novo or s-AML 1 or t-AML 2
|
overall response (CR 8/Cri 10) rate: 73%
|
median OS 11: 15.4 months
|
30-day mortality: 6%
|
|
daunorubicin
+ cytarabine
+ venetoclax
(5 + 2 + VEN)/[20]
|
retrospective clinical trial
|
composite complete remission
|
12
|
patients aged ≥ 60 years
|
CR 8 rate: 91.7% All patients with poor-risk achieved CR 8
|
estimated 1-year EFS 12: 75%.
Estimated 1-year OS 11 rate: 100%
|
30-day mortality: 0%
|
|
cyclophosphamide
+ cytarabine
+ venetoclax
(VCA)/[22]
|
pilot study
|
complete remission rate
|
25
|
adult AML 3
|
CR 8/Cri 10: 92%; all these patients had undetectable MRD 9
|
Estimated 12-month
OS 11: 79.3%.
|
/
|
|
fludarabine
+ cytarabine
+ idarubicin
+ filgastrim
+ venetoclax
(FLAG-IDA + VEN)/[24]
|
phase Ib/II
|
overall response rate
|
45
|
patients aged ≥18 (including de novo, sAML 1, tAML 2, tsAML 4, or high-risk MDS 5)
|
ORR 7: 98%; among CR 8 patients, 93% MRD 9 negative
|
estimated 24-month EFS 12: 64%
estimated 24-month
OS 11: 76%,
|
30-day mortality: 0%
60-day mortality: 0%
|
|
fludarabine
+ cytarabine
+ idarubicin
+ venetoclax
(V-FLAI)/[28]
|
phase I/II trial
|
complete remission rate
|
57
|
European LeukemiaNet intermediate- or high-risk adult AML 3 (median age 54 years; 18–65)
|
CR 8 rate: 84%;
MRD 9 negative: 74%
|
probability of 12-month OS 11: 76%
|
30-day mortality: 1.8%
60-day mortality 5.3%
|
|
cladribine
+ cytarabine
+ idarubin
+ venetoclax
(CLIA + VEN)/[29]
|
phase II
|
complete response rate
|
67
|
patients aged ≤65 years with newly diagnosed AML 3 or high-risk MDS 5
|
CRc 7 rate: 96%; among CR 8 patients, 90% MRD 9 negative
|
estimated 12-month OS 11: 86.5%
estimated 24-month OS 11: 86.5%
estimated 12-month EFS 12: 71.8%
estimated 24-month EFS 12: 69.7%
|
30-day mortality: 2%
60-day mortality 3%
|
|
CPX-351
+ venetoclax
(CPX-351 + VEN)/[31]
|
phase Ib/II
|
the safe dose and schedule
|
5
|
patients aged ≥ 18 years
|
CR 8/CRi 10: 80%; 75% MRD 9 negative
|
1-year estimated OS 11: 75%
|
30-day mortality: 0%
60-day mortality: 0%
|
1 s-AML = secondary acute myeloid leukemia. 2 t-AML = therapy-related acute myeloid leukemia. 3 AML = acute myeloid leukemia. 4 ts-AML = treated secondary acute myeloid leukemia. 5 MDS = myelodysplastic syndrome. 6 CRc = composite complete remission. 7 ORR = overall response rate. 8 CR = complete remission. 9 MRD = minimal residual disease. 10 CRi = complete remission with incomplete bone marrow recovery. 11 OS = overall survival. 12 EFS = event-free survival. 13 DFS= disease-free survival.
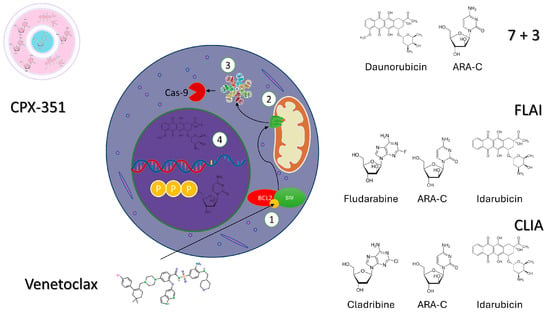
3. Venetoclax Plus Intensive Chemotherapy in Refractory/Resistant AML
The FLAG-IDA plus VEN regimen was investigated in an R/R-AML setting and showed encouraging preliminary results. After the starting 39 patients were treated [
23], a protocol amendment recommended reducing the VEN-treatment days from 21 to 14 days and the cytarabine dose from 2 to 1.5 g/m
2 (phase 2 cohort) due to the occurrence of severe grade 3 and grade 4 neutropenia-related infections in the initial phase Ib study. Therefore, further trials combining VEN plus IC regimens were designed with a shorter 7-day VEN regimen [
29]. Among the R/R AML patients included in the FLAG-IDA plus VEN trial phases Ib (
n = 16; median age, 51 years) and IIB (
n = 23; median age, 47 years) [
23], the CR + Cri rate was 67% (69% were MRD-negative), and 46% proceeded to consolidative HSCT. The estimated 1-year EFS and OS rates were 41% and 68%, respectively, which represent a significant outcome amelioration in comparison with historical results for R/R AML [
33,
34]. The rate of adverse events resembled that observed in de novo AML trials. Febrile neutropenia and bacteremia were observed in 51% and 46% of the patients, respectively, with an increased rate of sepsis documented in the phase 1b cohort compared with the phase 2 cohorts (50% versus 43%). The 30-day and 60-day mortality among this high-risk group was 0% and 4.4%, respectively.
The FLA-IDA plus VEN (FLAVIDA) regimen (VEN given at 100 mg daily for 7 days when posaconazole was co-administered) was investigated in 13 R/R-AML patients who were predominantly in first-salvage therapy (number of previous lines of treatment: 1–5) and who were classified as ELN intermediate- and high-risk (84.6%) AML [
36]. The ORR after induction was 69%, with a median time of CR/Cri maintenance of 7.3 months and an estimated 6-month EFS and OS of 52% and 76%, respectively. Afterward, a retrospective analysis of the same study analyzed the difference between 37 patients receiving FLAVIDA and a cohort of 81 patients treated with FLA-IDA but without VEN. The two cohorts were normalized according to age, genetic characteristics, R/R status, and previous HSCT [
37]. Patients treated with the FLAVIDA regimen showed a more significantly improved ORR (78% vs. 47%,
p = 0.001); however, no significant difference was observed in terms of the OS and bone-marrow recovery time post-therapy between the two groups.
An approach based on the combination of VEN with high-dose cytarabine and mitoxantrone (HAM) was investigated in the phase I/II Alliance Leukemia (SAL) Relax trial [
38]. Twelve patients (median age: 57 years) presenting with relapsed AML were included in this dose-finding phase study. The combination of VEN 400 mg daily (after a 3-day ramp-up) on days 3 to 14 and HAM proved secure and effective, leading 11 out of 12 patients to achieve remission.
Finally, the administration of VEN in an R/R setting has also been explored in combination with CPX-351. A phase 2 trial enrolled 26 R/R-AML patients; among them, 10 (42%) had a complex karyotype and 6 (23%) were TP53-mutated AML [
31]. The CR/Cri rate was 46%. Furthermore, 78% of CR/Cri patients achieved MRD negativity. Out of the 12 responding patients, 10 (83%) underwent HSCT. The 4- and 8-week mortality was 12% and 19%, respectively, with the most common grade 3 and grade 4 adverse events including infections, pneumonia, and febrile neutropenia. The 1-year estimated OS was 39%, while in responding patients, the median OS was 26.9 months.
Table 2 summarizes these trials, including the combination of VEN and chemotherapy in an R/R setting.
Table 2. Trials including a venetoclax and chemotherapy combination in relapsed/refractory AML.
1 CR = complete remission. 2 Cri = complete remission with incomplete bone marrow recovery. 3 MRD = minimal residual disease. 4 HSCT = hematopoietic stem cell transplantation. 5 CRc = composite complete remission. 6 ORR = overall response rate. 7 EFS = event-free survival. 8 OS = overall survival. 9 RFS = relapse-free survival.
4. Venetoclax Plus Intensive Chemotherapy in Pediatric AML
The first study combining VEN plus IC in a pediatric setting was conducted at the St. Jude Children’s Research Hospital. The trial enrolled 2- to-22-year-old R/R-AML patients, evaluating as the primary endpoint the safety and activity of VEN (240 or 360 mg/m
2/day orally for 28 days) in combination with cytarabine (100 mg/m
2 every 12 h for 20 doses or 1000 mg every 12 h for 8 doses) and with or without idarubicin (12 mg/m
2) as a single dose. Results of this phase 1 study also indicated the recommended phase 2 dose of VEN plus IC [
39]. In the following phase 2 trial, 38 patients were enrolled, and the recommended doses were 360 mg/m
2 for VEN and 1000 mg/m
2 (8 doses) for cytarabine. Overall responses were documented in 24 (69%) of 35 evaluable cases, comprising 16 CRs (11 MRD-negative). A large number (80%) of patients who reached CR/CRi, all of whom were MRD-negative after cycle 1, proceeded to a subsequent HSCT. The most frequent grade 3–4 toxicities resulted of febrile neutropenia (25 patients), bloodstream infections (6 patients), and invasive fungal infections (6 patients), with treatment-related death observed in one patient.
A recent retrospective analysis detailed the outcomes of pediatric patients with R/R AML who underwent VEN treatment before HSCT at St. Jude Children’s Research Hospital [
40]. Twenty-five pediatric patients (median age: 13.1 years) received VEN-based salvage therapy (VEN/cytarabine, 15; VEN/cytarabine/idarubicin, 5; VEN/cytarabine/azacytidine, 3; or VEN/decitabine, 2) prior to HSCT. Notably, 9 of the 25 patients had already undergone a prior HSCT. The last dose of VEN was administered at a median of 19 days prior to the start of the HSCT conditioning regimen. At the time of the HSCT, 14 patients were in MRD-negative CR, 9 patients were MRD+ (≥0.01%), and 2 patients had active disease (bone marrow blasts > 5%). At a median follow-up of 280 days from HSCT, the 1-year overall survival (OS) was 80% and leukemia-free survival was 74.5%. Unfortunately, six patients relapsed at a median of 143 days, and only one patient experienced non-relapse mortality.
An Italian multicenter retrospective analysis of pediatric patients (0–18 years) with R/R AML or advanced MDS arising after chemotherapy or radiation therapy who received VEN-based combination therapies was reported. Thirty-one patients (median age: 10.2 years) experiencing a median of three previous lines of therapy (31.2% relapsed after HSCT) were included in the analysis [
41]. The rates of CR, partial response, and no response were 66.7%, 11.1%, and 22.2% of cases, respectively. Of note, patients who received VEN with hypomethylating agents achieved CR, a partial response, no response, and treatment failure in 36.8%, 26.3%, 31.6%, and 5.3% of cases, respectively. Twenty patients (64%) were successfully bridged to HSCT by VEN therapy after a median time of 3.3 months from the start of the VEN treatment. The estimated 30-month OS after the start of VEN was 29.9% for the whole cohort and 74.4% for patients undergoing HSCT.
According to this data, the combination of VEN plus IC therapy demonstrates efficacy in the pediatric setting for AML, with a tolerability profile similar to that observed in adult AML. Nevertheless, additional data are needed to substantiate the actual benefits of this approach and to assess its potential role in frontline regimens.
5. Molecular Markers Predicting the Response to Venetoclax and Chemotherapy-Based Regimens
The combination of VEN plus IC demonstrates significant efficacy across various genetic subgroups in AML. In patients with ELN favorable-, intermediate-, or unfavorable-risk AML, frontline treatment with FLAG-IDA plus VEN yields composite CR rates of 88%, 89%, and 89%, respectively [
24]. Similarly, patients receiving CLIA plus VEN for ELN favorable-, moderate-, or high-risk AML exhibit 1-year survival rates of 78%, 93%, and 81%, respectively [
29]. The efficacy of the regimen including VEN plus “2 + 6” daunorubicin and cytarabine is evident across the ELN2022 risk groups. For the favorable-risk group, the estimated 12-month OS, EFS, and DFS rates are 87.5%, 88.9%, and 100%, respectively. The intermediate-risk patients show a rate of 100% for all three endpoints, while adverse-risk patients exhibit a rate of 70.7%, 70.3%, and 79.9%, respectively [
18]. The FLAG-IDA plus VEN regimen also showed efficacy in patients with extramedullary localization of the disease; indeed, among patients with extramedullary AML (three with de novo AML and one with R/R AML), all had durable responses, with three going on to HSCT [
24].
According to the CAVEAT trial, a seven-day VEN pre-phase before combining the “5 + 2” regimen resulted in a significant reduction in bone marrow blasts in patients with de novo AML, especially in those patients with
NPM1 (56% reduction),
IDH2 (55% reduction), or
SRSF2 (47% reduction) mutations. As a result, patients with these mutations showed an encouraging median OS (
NPM1: 13.2 months;
IDH2: not reached; and
SRSF2: 31.3 months) [
19]. In a subsequent analysis of the CAVEAT study evaluating the TFR duration in patients showing CR/Cri, 75% of patients with an
NPM1 or
IDH2 mutation at diagnosis were in TFR [
19]. Notably, R/R patients presenting with
NPM1, IDH1, and
IDH2 mutations also showed promising responses when they received an intensive combination treatment with VEN. Indeed, the FLAG-IDA plus VEN approach produced 100% composite CR in these molecular subgroups, thereby allowing 71% of the patients to undergo HSCT [
23]. Also,
KMT2A-rearranged patients showed a 100% composite CR rate (80% MRD-negativity by PCR for
KMT2A) after FLAG-IDA plus VEN, with a consequent 1-year OS of 80% [
23]. However, in a pediatric trial [
39], among 12 patients with
KMT2A rearrangements, 5 patients showed no response.
While FLAG-IDA plus VEN did not predict the outcome of patients presenting with signaling pathway gene mutations (
K/NRAS,
PTPN11,
FLT3,
CBL, and
KIT) in the frontline setting, R/R-AML patients with these mutations showed a lower median OS than patients with wild-type signaling genes. Similar findings were noted in R/R-AML patients, where tumor-suppressor gene mutations (
TP53,
WT1,
FBXW7, or
PHF6) were linked to a considerably lower rate of composite CR (38%) and a worse prognosis (median OS: 7 months) [
23].
In the CAVEAT trial, the lowest blast reductions after VEN pre-phase treatment were observed in patients with
TP53 and kinase-activating mutations (
FLT3-ITD,
FLT3-TKD,
RAS, and
PTPN11). Consequently, dismal OS outcomes were observed in patients with
TP53 (3.6 months) and
FLT3-ITD (5.5 months) mutations [
19]. In a CLIA plus VEN trial [
29], 15 patients had a
FLT3-ITD and/or -
TKD mutation, and 9 of these patients received a concomitant FLT3 inhibitor during induction and consolidation. Patients receiving a concomitant FLT3 inhibitor had a similar OS (
p = 0.38) and EFS (
p = 0.20) compared with those receiving VEN plus CLIA alone. In the FLAG-IDA plus VEN trial, 10 patients (3 with de novo AML and 7 with R/R AML) showed
TP53 mutations at baseline. The overall composite CR rate was 60%, with a median duration of response and OS of 3.4 and 9 months in de novo AML and 3.2 and 7 months in R/R AML, respectively [
23].
Recently, data from VIALE-A demonstrated that AML patients without specific genetic mutations (
FLT3-ITD,
K/RAS,
N/RAS, and
TP53 mutations) may derive a greater benefit from the combination of VEN and AZA [
42]. In this subgroup of patients, the median OS was reported to be 26 months, which represents a significant improvement compared with traditional treatment approaches. The identification of specific molecular profiles that predict a higher benefit from VEN plus IC treatments is an important goal in AML research. Indeed, the possibility of tailoring treatment based on a patient’s genetic and molecular characteristics can help to optimize outcomes and to minimize potential side effects.