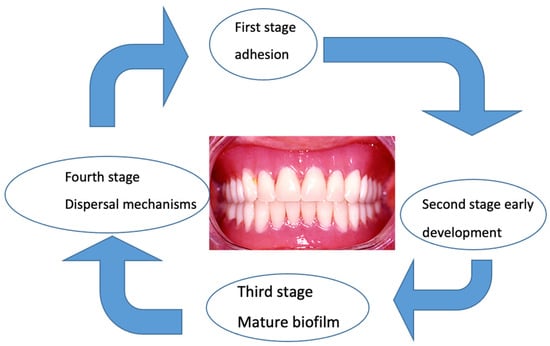
Whichever polymer is used in the composition of the prosthetic base (poly methyl methacrylate acrylic (PMMA), polyamide (PA), or polyether ether ketone (PEEK)), the simple presence of a removable prosthesis in the oral cavity can disturb the balance of the oral microbiota. This phenomenon is aggravated by poor oral hygiene, resulting in an increased microbial load coupled with the reduced salivation that is associated with older patients. In 15–70% of patients, this imbalance leads to the appearance of inflammation under the prosthesis (denture stomatitis, DS). DS is dependent on the equilibrium—as well as on the reciprocal, fragile, and constantly dynamic conditions—between the host and the microbiome in the oral cavity. Several local and general parameters contribute to this balance. Locally, the formation of microbial plaque on dentures (DMP) depends on the phenomena of adhesion, aggregation, and accumulation of microorganisms. To limit DMP, apart from oral and lifestyle hygiene, the prosthesis must be polished and regularly immersed in a disinfectant bath. It can also be covered with an insulating coating. In the long term, relining and maintenance of the prosthesis must also be established to control microbial proliferation. On the other hand, several general conditions specific to the host (aging; heredity; allergies; diseases such as diabetes mellitus or cardiovascular, respiratory, or digestive diseases; and immunodeficiencies) can make the management of DS difficult.
- Candida spp.
- dental plaque biofilm
- denture management
- denture hygiene
- denture stomatitis
- microbiome
- systemic
1. Introduction
2. Polymers in the Oral Environment
2.1. Polymer and Microbial Adhesion
2.2. PMMA and Adhesion
2.3. Polyamide and Adhesion
2.4. PEEK and Adhesion
2.5. Polymer and Accumulation of DMP
2.6. Polishing to Limit Microbial Adhesion
2.7. Denture Base Surface Coating to Limit Adhesion
2.8. Effects of Cleaning on Denture Materials
3. Denture Base Relining
4. General Conditions and Dentures
This entry is adapted from the peer-reviewed paper 10.3390/polym16010040
References
- Hao, Y.; Huang, X.; Zhou, X.; Li, M.; Ren, B.; Peng, X.; Cheng, L. Influence of dental prosthesis and restorative materials interface on oral biofilms. Int. J. Mol. Sci. 2018, 19, 3157.
- Sachdeo, A.; Haffajee, A.D.; Socransky, S.S. Biofilms in the edentulous oral cavity. J. Prosthodont. 2008, 17, 348–356.
- Sang, T.; Ye, Z.; Fischer, N.G.; Skoe, P.E.; Echeverría, C.; Wu, J.; Aparicio, C. Physical-chemical interactions between dental materials surface, salivary pellicle and Streptococcus gordonii. Colloids Surf. B 2020, 190, 110938.
- Mitchell, K.F.; Zarnowski, R.; Sanchez, H.; Edward, J.A.; Reinicke, E.L.; Nett, J.E.; Mitchell, A.P.; Andes, D.R. Community participation in biofilm matrix assembly and function. Proc. Natl. Acad. Sci. USA 2015, 112, 4092–4097.
- Ercalik-Yalcinkaya, S.; Ozcan, M. Association between oral mucosal lesions and hygiene habits in a population of removable prosthesis wearers. J. Prosthodont. 2015, 24, 271–278.
- Latib, Y.O.; Owen, C.P.; Patel, M. Viability of Candida albicans in denture base resin after disinfection: A preliminary study. Int. J. Prosthodont. 2018, 31, 436–439.
- Cruz, P.C.; Andrare, I.M.; Peracini, A.; Souza-Gugelmin, M.C.M.; Silva-Lovato, C.H.; de Souza, R.F.; Paranhos, H.d.F.O. The effectiveness of chemical denture cleansers and ultrasonic device in biofilm removal from complete dentures. J. Appl. Oral Sci. 2011, 19, 668–673.
- Axe, A.S.; Varghese, R.; Bosma, M.; Kitson, N.; Bradshaw, D.J. Dental health professional recommendation and consumer habits in denture cleansing. J. Prosthet. Dent. 2016, 115, 183–188.
- Abaci, Ö. Investigation of extracellular phospholipase and proteinase activities of Candida species isolated from individual’s denture wearers and genotypic distribution of Candida albicans strains. Curr. Microbiol. 2011, 62, 1308–1314.
- Zarnowski, R.; Westler, W.M.; Lacmbouh, G.A.; Marita, J.M.; Bothe, J.R.; Bernhardt, J.; Lounes-Hadj Sahraoui, A.; Fontaine, J.; Sanchez, H.; Hatfield, R.D.; et al. Novel entries in a fungal biofilm matrix encyclopedia. mBio 2014, 5, e01333-14.
- Kavanaugh, J.S.; Flack, C.E.; Lister, J.; Ricker, E.B.; Ibberson, C.B.; Jenul, C.; Moormeier, D.E.; Delmain, E.A.; Bayles, K.W.; Horswill, A.R. Identification of extracellular DNA-binding proteins in the biofilm matrix. mBio 2019, 10, e01137-19.
- Cahn, L.R. The Denture sore mouth. Ann. Dent. 1936, 3, 33–36.
- Koopmans, A.S.; Kippuw, N.; de Graaff, J. Bacterial involvement in denture-induced stomatitis. J. Dent. Res. 1988, 67, 1246–1250.
- Campos, M.S.; Marchini, L.; Bernardes, L.A.; Paulino, L.C.; Nobrega, F.G. Biofilm microbial communities of denture stomatitis. Oral Microbiol. Immunol. 2008, 23, 419–424.
- Salerno, C.; Pascale, M.; Contaldo, M.; Esposito, V.; Busciolano, M.; Milillo, L.; Guida, A.; Petruzzi, M.; Serpico, R. Candida-associated denture stomatitis. Med. Oral Patol. Oral Cir. Bucal 2011, 16, e139–e143.
- Schaller, M.; Borelli, C.; Korting, H.C.; Hube, B. Hydrolytic enzymes as virulence factors of Candida albicans. Mycoses 2005, 48, 365–377.
- Cavalcanti, Y.W.; Wilson, M.; Lewis, M.; Williams, D.; Senna, P.M.; Del-Bel-Cury, A.A.; Silva, W.J. Salivary pellicles equalize surfaces’ charges and modulate the virulence of Candida albicans biofilm. Arch. Oral Biol. 2016, 6, 129–140.
- Rickard, A.H.; Gilbert, P.; High, N.J.; Kolenbrander, P.E.; Handley, P.S. Bacterial coaggregation: An integral process in the development of multi-species biofilms. Trends Microbiol. 2003, 11, 94–100.
- Ruhl, S.; Eidt, A.; Melzl, H.; Reischl, U.; Cisar, J.O. Probing of microbial biofilm communities for coadhesion partners. Appl. Environ. Microbiol. 2014, 80, 6583–6590.
- Fox, E.P.; Bui, C.K.; Nett, J.E.; Hartooni, N.; Mui, M.C.; Andes, D.R.; Nobile, C.J.; Johnson, A.D. An expanded regulatory network temporally controls Candida albicans biofilm formation. Mol. Microbiol. 2015, 96, 1226–1239.
- Li, P.; Seneviratne, C.J.; Alpi, E.; Vizcaino, J.A.; Jin, L. Delicate metabolic control and coordinated stress response critically determine antifungal tolerance of Candida albicans biofilm persisters. Antimicrob. Agents Chemother. 2015, 59, 6101–6112.
- Santana, I.L.; Gonçalves, L.M.; de Vasconcellos, A.A.; da Silva, W.J.; Cury, J.A.; Cury, A.A.D.B. Dietary carbohydrates modulate Candida albicans biofilm development on the denture surface. PLoS ONE 2013, 8, e64645.
- Arendorf, T.M.; Walker, D.M. The prevalence and intra-oral distribution of Candida albicans in man. Arch. Oral Biol. 1980, 25, 1–10.
- Morse, D.J.; Smith, A.; Wilson, M.J.; Marsh, L.; White, L.; Posso, R.; Bradshaw, D.J.; Wei, X.; Lewis, M.A.O.; Williams, D.W. Molecular community profiling of the bacterial microbiota associated with denture-related stomatitis. Sci. Rep. 2019, 9, 10228.
- O’Donnell, L.E.; Robertson, D.; Nile, C.J.; Cross, L.J.; Riggio, M.; Sherriff, A.; Bradshaw, D.; Lambert, M.; Malcolm, J.; Buijs, M.J.; et al. The oral microbiome of denture wearers is influenced by levels of natural dentition. PLoS ONE 2015, 10, e0137717.
- Teles, F.R.; Teles, R.P.; Sachdeo, A.; Uzel, N.G.; Song, X.Q.; Torresyap, G.; Singh, M.; Papas, A.; Haffajee, A.; Socransky, S. Comparison of microbial changes in early redeveloping biofilms on natural teeth and dentures. J. Periodontol. 2012, 83, 1139–1148.
- Murugesan, S.; Al Ahmad, S.F.; Singh, P.; Saadaoui, M.; Kumar, M.; Al Khodor, S. Profiling the salivary microbiome of the Qatari population. J. Transl. Med. 2020, 18, 127.
- Perić, M.; Živković, R.; Milić Lemić, A.; Radunović, M.; Miličić, B.; Arsenijević, V.A. The severity of denture stomatitis as related to risk factors and different Candida spp. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 126, 41–47.
- Vila, T.; Sultan, A.S.; Montelongo-Jauregui, D.; Jabra-Rizk, M.A. Oral Candidiasis: A disease of opportunity. J. Fungi 2020, 6, 15.
- Steele, J.G.; Treasure, E.T.; Fuller, E.; Morgan, M.Z. Complexity and maintenance—A report from the Adult Dental Health Survey. In Adult Dental Health Survey 2009—Northern Ireland Key Findings; O’Sullivan, I., Ed.; The Health and Social Care Information Centre: London, UK, 2011; pp. 7–9.
- Theilade, E.; Budtz-Jørgensen, E.; Theilade, J. Predominant cultivable microflora of plaque on removable dentures in patients with healthy oral mucosa. Arch. Oral Biol. 1983, 28, 675–680.
- Shi, B.; Wu, T.; McLean, J.; Edlund, A.; Young, Y.; He, X.; Lv, H.; Zhou, X.; Shi, W.; Li, H.; et al. The denture-associated oral microbiome in health and stomatitis. mSphere 2016, 1, e00215–e00216.
- Lof, M.; Janus, M.; Krom, B. Metabolic interactions between bacteria and fungi in commensal oral biofilms. J. Fungi 2017, 3, 40.
- Senpuku, H.; Sogame, A.; Inoshita, E.; Tsuha, Y.; Miyazaki, H.; Hanada, N. Systemic diseases in association with microbial species in oral biofilm from elderly requiring care. Gerontology 2003, 49, 301–309.
- Yildirim-Bicer, A.Z.; Peker, I.; Akca, G.; Celik, I. In vitro antifungal evaluation of seven different disinfectants on acrylic resins. Biomed Res. Int. 2014, 2014, 519098.
- Ardizzoni, A.; Pericolini, E.; Paulone, S.; Orsi, C.F.; Castagnoli, A.; Oliva, I.; Strozzi, E.; Blasi, E. In vitro effects of commercial mouthwashes on several virulence traits of Candida albicans, viridans streptococci and Enterococcus faecalis colonizing the oral cavity. PLoS ONE 2018, 13, e0207262.
- Radford, D.R.; Challacombe, S.; Walter, J.D. Denture plaque and adherence of candida albicans to denture-base materials in vivo and in vitro. Crit. Rev. Oral Biol. Med. 1999, 10, 99–116.
- Zheng, W.; Tsompana, M.; Ruscitto, A.; Sharma, A.; Genco, R.; Sun, Y.; Buck, M.J. An accurate and efficient experimental approach for characterization of the complex oral microbiota. Microbiome 2015, 3, 48.
- Fujinami, W.; Nishikawa, K.; Ozawa, S.; Hasegawa, Y.; Takebe, J. Correlation between the relative abundance of oral bacteria and Candida albicans in denture and dental plaques. J. Oral Biosci. 2021, 63, 175–183.
- Delaney, C.; O’Donnell, L.E.; Kean, R.; Sherry, L.; Brown, J.L.; Calvert, G.; Nile, C.J.; Cross, L.; Bradshaw, D.J.; Brandt, B.W.; et al. Interkingdom interactions on the denture surface: Implications for oral hygiene. Biofilm 2019, 1, 100002.
- Kostic, M.; Pejcic, A.; Igic, M.; Gligorijević, N. Adverse reactions to denture resin materials. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 5298–5305.
- Figueiral, M.H.; Azul, A.; Pinto, E.; Fonseca, P.A.; Branco, F.M.; Scully, C. Denture-related stomatitis: Identification of aetiological and predisposing factors? A large cohort. J. Oral Rehabil. 2007, 34, 448–455.
- Coulthwaite, L.; Verran, J. Development of an in vitro denture plaque biofilm to model denture malodour. J. Breath Res. 2008, 2, 017004.
- Yitzhaki, S.; Reshef, L.; Gophna, U.; Rosenberg, M.; Sterer, N. Microbiome associated with denture malodour. J. Breath Res. 2018, 12, 027103.
- Garg, R.; Garg, R.K. Denture hygiene, different strategies. Webmed Cent. Dent. 2010, 10, WMC00932.
- Rüttermann, S.; Trellenkamp, T.; Bergmann, N.; Raab, W.H.R.; Ritter, H.; Janda, R. A new approach to influence contact angle and surface free energy of resin-based dental restorative materials. Acta Biomater. 2011, 7, 1160–1165.
- Liber-Knéc, A.; Łagan, S. Surface Testing of Dental Biomaterial Determination of Contact Angle and Surface Free Energy. Materials 2021, 14, 2716.
- Helal, M.A.; Fadl-Alah, A.; Baraka, Y.M.; Gad, M.M.; Emam, A.-N.M. In-vitro comparative evaluation for the surface properties and impact strength of CAD/CAM milled, 3D printed, and polyamide denture base resins. J. Int. Soc. Prev. Community Dent. 2022, 12, 126–131.
- Pereira-Cenci, T.; Cury, A.A.D.B.; Cenci, M.S.; Rodrigues-Garcia, R.C.M. In vitro candida colonization on acrylic resins and denture liners: Influence of surface free energy, roughness, saliva, and adhering bacteria. Int. J. Prosthodont. 2007, 20, 308–310.
- Olms, C.; Yahiaoui-Doktor, M.; Remmerbach, T.; Stingu, C. Bacterial colonization and tissue compatibility of denture base resins. Dent. J. 2018, 6, 20.
- Mukai, Y.; Torii, M.; Urushibara, Y.; Kawai, T.; Takahashi, Y.; Maeda, N.; Ohkubo, C.; Ohshima, T. Analysis of plaque microbiota and salivary proteins adhering to dental materials. J. Oral Biosci. 2020, 62, 182–188.
- de Foggi, C.C.; Machado, A.L.; Zamperini, C.A.; Fernandes, D.; Wady, A.F.; Vergani, C.E. Effect of surface roughness on the hydrophobicity of a denture-base acrylic resin and Candida albicans colonization. J. Investig. Clin. Dent. 2016, 7, 141–148.
- Vila, T.; Rizk, A.M.; Sultan, A.S.; Jabra-Rizk, M.A. The power of saliva: Antimicrobial and beyond. PLoS Pathog. 2019, 15, 1008058.
- Queiroz, J.R.C.; Fissmer, S.F.; Koga-Ito, C.Y.; Salvia, A.C.R.D.; Massi, M.; Sobrinho, A.S.d.S.; Júnior, L.N. Effect of diamond-like carbon thin film coated acrylic resin on candida albicans biofilm formation: Effect of dlc film on biofilm formation. J. Prosthodont. 2013, 22, 451–455.
- Bajunaid, S.O.; Baras, B.H.; Weir, M.D.; Xu, H.H.K. Denture acrylic resin material with antibacterial and protein-repelling properties for the prevention of denture stomatitis. Polymers 2022, 14, 230.
- Sarkar, A.; Kuehl, M.N.; Alman, A.C.; Burkhardt, B.R. Linking the oral microbiome and salivary cytokine abundance to circadian oscillations. Sci. Rep. 2021, 11, 2658.
- Gad, M.M.; Abualsaud, R.; Khan, S.Q. Hydrophobicity of denture base resins: A systematic review and meta-analysis. J. Int. Soc. Prev. Community Dent. 2022, 12, 139–159.
- Choi, S.Y.; Habimana, O.; Flood, P.; Reynaud, E.G.; Rodriguez, B.J.; Zhang, N.; Casey, E.; Gilchrist, M.D. Material-and feature-dependent effects on cell adhesion to micro injection moulded medical polymers. Colloids Surf. B Biointerfaces 2016, 145, 46–54.
- Sipahi, C.; Anil, N.; Bayramli, E. The effect of acquired salivary pellicle on the surface free energy and wettability of different denture base materials. J. Dent. 2001, 29, 197–204.
- Moslehifard, E.; Ghaffari, T.; Abolghasemi, H.; Maleki Dizaj, S. Comparison of conventional pressure-packed and injection molding processing methods for an acrylic resin denture based on microhardness, surface roughness, and water sorption. Int. J. Dent. 2022, 2022, 7069507.
- de Freitas Fernandes, F.S.; Pereira-Cenci, T.; da Silva, W.J.; Filho, A.P.R.; Straioto, F.G.; Del Bel Cury, A.A. Efficacy of denture cleansers on candida spp. biofilm formed on polyamide and polymethyl methacrylate resins. J. Prosthet. Dent. 2011, 105, 51–58.
- Vojdani, M.; Giti, R. Polyamide as a denture base material: A literature review. J. Dent. 2015, 16, 1–9.
- Sultana, N.; Ahmed, S.; Nandini, V.V.; Lathief, J.; Boruah, S. An in vitro comparison of microbial adhesion on three different denture base materials and its relation to surface roughness. Cureus 2023, 15, e37085.
- Chuchulska, B.; Hristov, I.; Dochev, B.; Raychev, R. Changes in the surface texture of thermoplastic (monomer-free) dental materials due to some minor alterations in the laboratory protocol—Preliminary study. Materials 2022, 15, 6633.
- da Rocha, L.G.D.O.; Ribeiro, V.S.T.; de Andrade, A.P.; Gonçalves, G.A.; Kraft, L.; Cieslinski, J.; Suss, P.H.; Tuon, F.F. Evaluation of staphylococcus aureus and candida albicans biofilms adherence to peek and titanium-alloy prosthetic spine devices. Eur. J. Orthop. Surg. Traumatol. 2022, 32, 981–989.
- Hahnel, S.; Wieser, A.; Lang, R.; Rosentritt, M. Biofilm formation on the surface of modern implant abutment materials. Clin. Oral Impl Res. 2015, 26, 1297–1301.
- Skirbutis, G.; Dzingutė, A.; Masiliūnaitė, V.; Šulcaitė, G.; Žilinskas, J. A review of peek polymer’s properties and its use in prosthodontics. Stomatologija 2017, 19, 19–23.
- Neugebauer, J.; Adler, S.; Kisttler, F.; Kistler, S.; Bayer, G. The use of plastics in fixed prosthetic implant restoration. Zwr-Ger. Dent. J. 2013, 122, 242–245.
- Gad, M.M.; Abu-Rashid, K.; Alkhaldi, A.; Alshehri, O.; Khan, S.Q. Evaluation of the effectiveness of bioactive glass fillers against candida albicans adhesion to PMMA denture base materials: An in vitro study. Saudi Dent. J. 2022, 34, 730–737.
- Vulović, S.; Todorović, A.; Stančić, I.; Popovac, A.; Stašić, J.N.; Vencl, A.; Milić-Lemić, A. Study on the surface properties of different commercially available cad/cam materials for implant-supported restorations. J. Esthet. Restor. Dent. 2022, 34, 1132–1141.
- Khattar, A.; Alghafli, J.A.; Muheef, M.A.; Alsalem, A.M.; Al-Dubays, M.A.; AlHussain, H.M.; AlShoalah, H.M.; Khan, S.Q.; AlEraky, D.M.; Gad, M.M. Antibiofilm activity of 3D-printed nanocomposite resin: Impact of ZrO2 nanoparticles. Nanomaterials 2023, 13, 591.
- Sawada, T.; Sawada, T.; Kumasaka, T.; Hamada, N.; Shibata, T.; Nonami, T.; Kimoto, K. Self-cleaning effects of acrylic resin containing fluoridated apatite-coated titanium dioxide. Gerodontology 2014, 31, 68–75.
- Lazarin, A.A.; Machado, A.L.; Zamperini, C.A.; Wady, A.F.; Spolidorio, D.M.P.; Vergani, C.E. Effect of experimental photopolymerized coatings on the hydrophobicity of a denture base acrylic resin and on Candida albicans adhesion. Arch. Oral Biol. 2013, 58, 1–9.
- Qian, K.; Pan, H.; Li, Y.; Wang, G.; Zhang, J.; Pan, J. Time-related surface modification of denture base acrylic resin treated by atmospheric pressure cold plasma. Dent. Mater. J. 2016, 35, 97–103.
- Yildirim, M.S.; Hasanreisoglu, U.; Hasirci, N.; Sultan, N. Adherence of candida albicans to glow-discharge modified acrylic denture base polymers. J. Oral Rehabil. 2005, 32, 518–525.
- Liu, T.; Xu, C.; Hong, L.; Garcia-Godoy, F.; Hottel, T.; Babu, J.; Yu, Q. Effects of trimethylsilane plasma coating on the hydrophobicity of denture base resin and adhesion of Candida albicans on resin sur-faces. J. Prosthet. Dent. 2017, 118, 765–770.
- Darwish, G.; Huang, S.; Knoernschild, K.; Sukotjo, C.; Campbell, S.; Bishal, A.K.; Barão, V.A.; Wu, C.D.; Taukodis, C.G.; Yang, B. Improving polymethyl methacrylate resin using a novel titanium dioxide coating. J. Prosthodont. 2019, 28, 1011–1017.
- Zamperini, C.A.; Machado, A.L.; Vergani, C.E.; Pavarina, A.C.; Giampaolo, E.T.; da Cruz, N.C. Adherence in vitro of candida albicans to plasma treated acrylic resin. Effect of plasma parameters, surface roughness and salivary pellicle. Arch. Oral Biol. 2010, 55, 763–770.
- Heimer, S.; Schmidlin, P.R.; Roos, M.; Stawarczyk, B. Surface properties of polyetheretherketone after different laboratory and chairside polishing protocols. J. Prosthet. Dent. 2017, 117, 419–425.
- Heimer, S.; Schmidlin, P.R.; Stawarczyk, B. Discoloration of pmma, composite, and peek. Clin. Oral Investig. 2017, 21, 1191–1200.
- Nishi, Y.; Seto, K.; Murakami, M.; Harada, K.; Ishii, M.; Kamashita, Y.; Kawamoto, S.; Hamano, T.; Yoshimura, T.; Kurono, A.; et al. Effects of denture cleaning regimens on the quantity of Candida on dentures: A cross-sectional survey on nursing home residents. Int. J. Environ. Res. Public. Health. 2022, 19, 15805.
- Duyck, J.; Vandamme, K.; Krausch-Hofmann, S.; Boon, L.; De Keersmaecker, K.; Jalon, E.; Teughels, W. Impact of denture cleaning method and overnight storage condition on denture biofilm mass and composition: A cross-over randomized clinical trial. PLoS ONE 2016, 11, e0145837.
- Sun, J.; Wang, L.; Wang, J.; Li, Y.; Zhou, X.; Guo, X.; Zhang, T.; Guo, H. Characterization and evaluation of a novel silver nanoparticles-loaded polymethyl methacrylate denture base: In vitro and in vivo animal study. Dent. Mater. J. 2021, 40, 1100–1108.
- Garcia, A.A.M.N.; Sugio, C.Y.C.; de Azevedo-Silva, L.J.; Gomes, A.C.G.; Batista, A.U.D.; Porto, V.C.; Soares, S.; Neppelenbroek, K.H. Nanoparticle-modified PMMA to prevent denture stomatitis: A systematic review. Arch. Microbiol. 2022, 204, 75.
- Apip, C.; Martínez, A.; Meléndrez, M.; Domínguez, M.; Marzialetti, T.; Báez, R.; Sánchez-Sanhueza, G.; Jaramillo, A.; Catalán, A. An in vitro study on the inhibition and ultrastructural alterations of candida albicans biofilm by zinc oxide nanowires in a PMMA matrix. Saudi Dent. J. 2021, 33, 944–953.
- Young, B.; Jose, A.; Cameron, D.; McCord, F.; Murray, C.; Bagg, J.; Ramage, G. Attachment of candida albicans to denture base acrylic resin processed by three different methods. Int. J. Prosthodont. 2009, 22, 488–489.
- Meirowitz, A.; Rahmanov, A.; Shlomo, E.; Zelikman, H.; Dolev, E.; Sterer, N. Effect of denture base fabrication technique on Candida albicans adhesion in vitro. Materials 2021, 14, 221.
- Mondelli, R.; Garrido, L.M.; Soares, A.; Rodriguez-Medina, A.; Mondelli, J.; de Lucena, F.; Furuse, A. Effect of simulated brushing on surface roughness and wear of bis-acryl-based materials submitted to different polishing protocols. J. Clin. Exp. Dent. 2022, 14, e168–e176.
- Alammari, M.R. The influence of polishing techniques on pre-polymerized cad/cam acrylic resin denture bases. Electron. Physician 2017, 9, 5452–5458.
- Al-Fouzan, A.F.; Al-mejrad, L.A.; Albarrag, A.M. Adherence of candida to complete denture surfaces in vitro: A comparison of conventional and CAD/CAM complete dentures. J. Adv. Prosthodont. 2017, 9, 402.
- Quezada, M.M.; Salgado, H.; Correia, A.; Fernandes, C.; Fonseca, P. Investigation of the effect of the same polishing protocol on the surface roughness of denture base acrylic resins. Biomedicines 2022, 10, 1971.
- Corsalini, M.; Boccaccio, A.; Lamberti, L.; Pappalettere, C.; Catapano, S.; Carossa, S. Analysis of the performance of a standardized method for the polishing of methacrylic resins. Open Dent. J. 2009, 3, 233–240.
- Sahin, O.; Koroglu, A.; Dede, D.Ö.; Yilmaz, B. Effect of surface sealant agents on the surface roughness and color stability of denture base materials. J. Prosthet. Dent. 2016, 116, 610–616.
- Liebermann, A.; Wimmer, T.; Schmidlin, P.R.; Scherer, H.; Löffler, P.; Roos, M.; Stawarczyk, B. Physicomechanical characterization of polyetheretherketone and current esthetic dental cad/cam polymers after aging in different storage media. J. Prosthet. Dent. 2016, 115, 321–328.
- Kurahashi, K.; Matsuda, T.; Ishida, Y.; Ichikawa, T. Effect of polishing protocols on the surface roughness of polyetheretherketone. J. Oral Sci. 2020, 62, 40–42.
- Liu, Y.; Fang, M.; Zhao, R.; Liu, H.; Li, K.; Tian, M.; Niu, L.; Xie, R.; Bai, S. Clinical applications of polyetheretherketone in removable dental prostheses: Accuracy characteristics, and performance. Polymers 2022, 14, 4615.
- Choi, J.J.E.; Uy, C.E.; Plaksina, P.; Ramani, R.S.; Ganjigatti, R.; Waddell, J.N. Bond strength of denture teeth to heat cured, cad/cam and 3d printed denture acrylics. J. Prosthodont. 2020, 29, 415–421.
- Behr, M.; Rosentritt, M.; Lang, R.; Handel, G. Glass fiber-reinforced abutments for dental implants. a pilot study: Glass fiber-reinforced abutments for dental implants. A pilot study. Clin. Oral Implant. Res. 2001, 12, 174–178.
- Pan, H.; Wang, G.; Pan, J.; Ye, G.; Sun, K.; Zhang, J.; Wang, J. Cold plasma-induced surface modification of heat-polymerized acrylic resin and prevention of early adherence of candida albicans. Dent. Mater. J. 2015, 34, 529–536.
- Gül, E.B.; Atala, M.H.; Eşer, B.; Polat, N.T.; Asiltürk, M.; Gültek, A. Effects of coating with different ceromers on the impact strength, transverse strength and elastic modulus of polymethyl methacrylate. Dent. Mater. J. 2015, 34, 379–387.
- Güngör, A.; Kayaman-Apohan, N.; Mert, A.; Kahraman, M.V. Preparation and characterization of light curable hybrid coating: Its potential application for dental restorative material. J. Polym. Res. 2008, 15, 389–395.
- Mylonas, P.; Milward, P.; McAndrew, R. Denture cleanliness and hygiene: An overview. Br. Dent. J. 2022, 233, 20–26.
- Estrela, A.; Estrela, C.R.A.; Barbin, E.L.; Spano, J.C.E.; Marchesan, M.A.; Pecora, J.D. Mechanism of action of sodium hypochlorite. Braz. Dent. J. 2002, 13, 113–117.
- De Sousa Porta, S.R.; de Lucena-Ferreira, S.C.; da Silva, W.J.; Del Bel Cury, A.A. Evaluation of sodium hypochlorite as a denture cleanser: A clinical study. Gerodontology 2015, 32, 260–266.
- Milward, P.; Katechia, D.; Morgan, M.Z. Knowledge of removable partial denture wearers on denture hygiene. Br. Dent. J. 2013, 215, E20.
- Kumar, B.; Sandhu, P.K.; Kumar, A.N.; Patil, C.P. A comparative study for plaque removing efficacy between commonly used denture cleansers in India. J. Indian. Prosthodont. Soc. 2017, 17, 295–300.
- De Souza, R.F.; de Freitas Oliveira Paranhos, H.; Lovato da Silva, C.H.; Abu-Naba’a, L.; Fedorowicz, Z.; Gurgan, C.A. Interventions for cleaning dentures in adults. Cochrane Data-Base Syst. Rev. 2009, 4, CD007395.
- Tulbah, H.I. Anticandidal efficacy on polymide based denture resin using Photodynamic therapy, chemical and herbal disinfectants and their effect on surface roughness and hardness. Photodiagn. Photodyn. Ther. 2022, 39, 102874.
- Ramage, G.; O’Donnell, L.; Sherry, L.; Culshaw, S.; Bagg, J.; Czesnikiewicz-Guzik, M.; Brown, C.; McKenzie, D.; Cross, L.; MacInnes, A.; et al. Impact of frequency of denture cleaning on microbial and clinical parameters—A bench to chairside approach. J. Oral Microbiol. 2019, 11, 1538437.
- Costa, R.T.F.; Pellizzer, E.P.; Vasconcelos, B.C.d.E.; Gomes, J.M.L.; Lemos, C.A.A.; Moraes, S.L.D. Surface roughness of acrylic resins used for denture base after chemical disinfection: A systematic review and meta-analysis. Gerodontology 2021, 38, 242–251.
- Masetti, P.; Arbeláez, M.I.A.; Pavarina, A.C.; Sanitá, P.V.; Jorge, J.H. Cytotoxic potential of denture base and reline acrylic resins after immersion in disinfectant solutions. J. Prosthet. Dent. 2018, 120, 155.
- Gad, M.M.; Abualsaud, R.; Fouda, S.M.; Rahoma, A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Al-Harbi, F.A. Effects of denture cleansers on the flexural strength of PMMA denture base resin modified with ZrO2 nanoparticles. J. Prosthodont. 2021, 30, 2356244.
- Amaya, A.M.I.; Vergani, C.E.; Barbugli, P.A.; Pavarina, A.C.; Sanitá, P.V.; Jorge, J.H. Long-term effect of daily chemical disinfection on surface topography and Candida albicans biofilm formation on denture base and reline acrylic resins. Oral Health Prev. Dent. 2020, 18, 999–1010.
- Kiesow, A.; Sarembe, S.; Pizzey, R.L.; Axe, A.S.; Bradshaw, D.J. Material compatibility and antimicrobial activity of consumer products commonly used to clean dentures. J. Prosthet. Dent. 2016, 115, 189–198.
- Mert, D.; Kamnoedboon, P.; Al-Haj Husain, N.; Özcan, M.; Srinivasan, M. CAD-CAM complete denture resins: Effect of relining on the shear bond strength. J. Dent. 2023, 131, 104438.
- Yuan, S.P.; Lin, H.; Pan, S.; Lou, L.L.; Xu, Y.X. Effect of Polident denture cleansers on the properties of heat-polymerized denture base acrylic resin. Beijing Da Xue Xue Bao Yi Xue Ban 2012, 44, 946–949.
- Demirci, F.; Tanik, A. Comparison of the effect of denture cleansers on long-term water sorption and solubility of polyetheretherketone with other denture base materials. Clin. Exp. Health Sci. 2022, 12, 672–677.
- Sesma, N.; Rocha, A.L.; Lagana, D.C.; Costa, B.; Morimoto, S. Effectiveness of denture cleanser associated with microwave disinfection and brushing of complete dentures: In vivo study. Braz. Dent. J. 2013, 24, 357–361.
- Arun Kumar, P.; Iniyan, K.; Balasubramaniam, R.; Viswanathan, M.; Hines, P.J.; Monnica, V. The effect of surface treatments on the shear bond strength of acrylic resin denture base with different repair acrylic resin: An in vitro study. J. Pharm. Bioall Sci. 2019, 11, 380.
- Kreve, S.; Dos Reis, A.C. Denture liners: A systematic review relative to adhesion and mechanical properties. Sci. World J. 2019, 2019, 6913080.
- Ates, S.M.; Caglar, I.; Ozdogan, A.; Duymus, Z.Y. The effect of denture cleansers on surface roughness and bond strength of a denture base resin. J. Adhes. Sci. Technol. 2017, 31, 171–181.
- Kümbüloğlu, Ö.; Yildirim, B.; Al-Haj Husain, N.; Özcan, M. Adhesion potential of relining materials to polyamide and PMMA-based denture base materials: Effect of surface conditioning methods. J. Adhes. Sci. Technol. 2019, 33, 1939–1947.
- AlZaher, Z.A.; Almaskin, D.F.; Qaw, M.S.; Abu Showmi, T.H.; Abualsaud, R.; Akhtar, S.; Gad, M.M. Chemo-mechanical approach to improve repair bond strength of denture teeth. Int. J. Dent. 2020, 2020, 8870361.
- Choi, J.E.; Ng, T.E.; Leong, C.K.Y.; Kim, H.; Li, P.; Waddell, J.N. Adhesive evaluation of three types of resilient denture liners bonded to heat-polymerized, autopolymerized, or CAD-CAM acrylic resin denture bases. J. Prosthet. Dent. 2018, 120, 699–705.
- Takahashi, Y.; Chai, J. Shear bond strength of denture reline polymers to denture base polymers. Int. J. Prosthodont. 2001, 14, 271–275.
- Taghva, M.; Enteghad, S.; Jamali, A.; Mohaghegh, M. Comparison of shear bond strength of CAD/CAM and conventional heat-polymerized acrylic resin denture bases to auto-polymerized and heat-polymerized acrylic resins after aging. J. Clin. Exp. Dent. 2022, 14, 72–78.
- Choi, J.J.E.; Ramani, R.S.; Ganjigatti, R.; Uy, C.E.; Plaksina, P.; Waddell, J.N. Adhesion of denture characterizing composites to heat cured, CAD/CAM and 3D printed denture base resins. J. Prosthodont. 2021, 30, 83–90.
- Luo, C.; Liu, Y.; Peng, B.; Chen, M.; Liu, Z.; Li, Z.; Kuang, H.; Gong, B.; Li, Z.; Sun, H. PEEK for oral applications: Recent advances in mechanical and adhesive properties. Polymers 2023, 15, 386.
- Kim, J.H.; Choe, H.C.; Son, M.K. Evaluation of adhesion of reline resins to the thermoplastic denture base resin for non-metal clasp denture. Dent. Mater. J. 2014, 33, 32–38.
- Vuksic, J.; Pilipovic, A.; Poklepovic Pericic, T.; Kranjcic, J. Tensile bond strength between different denture base materials and soft denture liners. Materials 2023, 16, 4615.
- Müller, F. Oral hygiene reduces the mortality from aspiration pneumonia in frail elders. J. Dent. Res. 2015, 94, 14–16.
- Le Bars, P.; Kouadio, A.A.; Bandiaky, O.N.; Le Guéhennec, L.; de La Cochetière, M.F. Host’s immunity and Candida species associated with denture stomatitis: A narrative review. Microorganisms 2022, 10, 1437.
- Ruiz Núñez, M.d.R.; Raulino, M.; Goulart Castro, R.; Schaefer Ferreira de Mello, A.L. Dental plaque control strategies for the elderly population: A scoping review. Int. J. Dent. Hyg. 2022, 20, 167–181.
- Patil, S.; Rao, R.S.; Majumdar, B.; Anil, S. Clinical appearance of oral candida infection and therapeutic strategies. Front. Microbiol. 2015, 6, 1391.
- Chladek, G.; Nowak, M.; Pakieła, W.; Mertas, A. Effect of Candida Albicans Suspension on the Mechanical Properties of Denture Base Acrylic Resin. Materials 2022, 15, 3841.
- Dhiman, R.; Chowdhury, S.R. Midline fractures in single maxillary complete acrylic vs flexible dentures. Med. J. Armed Forces India 2009, 65, 141–145.
- Takahashi, Y.; Imazato, S.; Russell, R.R.B.; Noiri, Y.; Ebisu, S. Influence of Resin Monomers on Growth of Oral Streptococci. J. Dent. Res. 2004, 83, 302–306.
- Kostić, M.; Igić, M.; Gligorijević, N.; Nikolić, V.; Stošić, N.; Nikolić, L. The use of acrylate polymers in dentistry. Polymers 2022, 14, 4511.
- Yoshii, E. Cytotoxic effects of acrylates and methacrylates: Relationships of monomer structures and cytotoxicity. J. Biomed. Mater. Res. A 1997, 37, 517–524.
- Hinz, S.; Bensel, T.; Bömicke, W.; Boeckler, A.F. In Vitro analysis of the mechanical properties of hypoallergenic denture base resins. Materials 2022, 15, 3611.
- Pfeiffer, P.; An, N.; Schmage, P. Repair strength of hypoallergenic denture base materials. J. Prosthet. Dent. 2008, 100, 292–301.
- Hirasawa, M.; Tsutsumi-Arai, C.; Takakusaki, K.; Oya, T.; Fueki, K.; Wakabayashi, N. Superhydrophilic co-polymer coatings on denture surfaces reduce candida albicans adhesion—An in vitro study. Arch. Oral Biol. 2018, 87, 143–150.
