1. Inorganic Biomaterials
1.1. Hydroxyapatite (Hap)
Hydroxyapatite, the chemical formula of which is Ca
10(OH)
2(PO4)
6, is an inorganic compound that is a key constituent of the mineralized portion of bones [
45]. It is one of the most used and relevant ceramic biomaterials in the realm of 3D printing [
46,
47]. Although research reporting the use of 3D-printed hydroxyapatite using VPP is limited, certain studies have illustrated that the resulting product exhibits increased precision and enhanced sensitivity and accuracy compared to alternative 3D printing technologies [
48]. Hap 3D-printed constructs have excellent bioactive properties, including increased biocompatibility, osteoinductivity, osteoconductivity, excellent bioresorbability and biodegradation, and near-to-zero cytotoxicity [
49,
50,
51,
52,
53]. These qualities hold significant importance in medical applications such as tissue engineering for bone grafts [
49,
50,
51,
53], dental root implants [
52], and coatings for 3D-printed metallic implants [
54,
55,
56].
Good results have been obtained by employing Hap in the 3D printing of bone grafts for bone regeneration. It is known that the pore sizes and shapes of these builds are the main modulators for enhanced or diminished osteoconductive properties [
51,
53]. Research has demonstrated that larger pore sizes (exceeding 300 μm) enhance the osteogenesis process [
57,
58], although the challenge lies in achieving a balance between pore size and shape (with cubic pores being more efficient [
50]) while maintaining the required mechanical performance [
59].
Printed with the same technology are Hap dental roots. In oral surgery, 3D printing parts of teeth has gained popularity. The most used and studied biocompatible material in this particular field is currently zirconium [
33], but recent studies have shown some promising results using DLP 3D-printed hydroxyapatite [
52]. There are still challenges in finding the ideal alloys that can also enhance the bacteriostatic properties [
52].
Despite not being printed via VPP, hydroxyapatite coatings are representative of the compound’s bioactive properties [
54]. As most orthopedic implants are composed of biocompatible metals such as titanium due to their superior biomechanical properties [
60], there are still some challenges with the biointegration of the implants, which can be effectively addressed through Hap coatings or Hap-ion coatings [
55].
Hydroxyapatite is a material with untapped potential. Some studies propose its usage in building feasible, sophisticated, and complex scaffolds that maintain the requirements of an artificial bone scaffold, or even bioactive and biocompatible mixtures with extracellular matrix proteins that can promote cellular integration and responsiveness [
53]. Possible enhancements in strength have also been reported, but the architecture and the porosities of the builds require further study [
51]. Furthermore, the development of antimicrobial implants in the fields of orthopedics and neurosurgery is also currently being explored [
55].
1.2. Zirconia
Zirconia, a crystalline oxide of zirconium (ZrO
2), can be shaped into a monolithic form suitable for medical applications. It stands out in the realm of dental ceramics due to its exceptional mechanical properties, rendering it both the strongest and most aesthetically pleasing ceramic [
33,
61,
62]. DLP is one of the most advanced 3D printing techniques used in the fabrication of ceramics due to its high speed and increased precision and accuracy [
63], as well as the fact that zirconia can be employed as a material [
33].
Despite not being inherently bioactive, zirconia-based structures find extensive use in dentistry [
64] thanks to a multitude of crucial properties, including rheological behavior, curing characteristics, biocompatibility, and mechanical and tribological performance [
33,
65,
66]. Factors such as resistance to bacterial colonization, low toxicity, and enhanced fracture strength are essential for the use of zirconia in dental implants [
64,
67,
68]. Unalloyed zirconia is suitable for dental crowns, bridges, implants, and abutments, as well as for teeth repair, as it can resist compressive strengths as high as 2000 Mpa [
33,
69]. Despite other materials being used in the past for dental implants, zirconia or other dental resin-based materials have gained popularity in the field due to rises in patient quality of life because of their clinical performance and aesthetic quality [
66]. Zirconia does not cause adverse reactions when interacting with oral tissues. Additional advantages of dental applications include chemical stability over time and the capacity for rapid printing [
10].
Zirconia stabilized with yttrium oxide (yttria) is an outstanding ceramic material used in dentistry due to its high stability and enhanced fracture strength [
70]. Comparative studies involving zirconia stabilized with 3 mol% and 8 mol% of yttria have demonstrated improved stability and printability when compared to unstabilized zirconia. There were minimal differences in printability observed between these two yttria concentrations when employing DLP printing technology [
65]. Research showed that the addition of yttria-stabilized zirconia in 3D dental constructs leads to enhanced thermomechanical and biological properties [
66].
As previously mentioned, zirconia lacks bioactive properties. Consequently, it finds applications not only in dentistry but also in orthopedic implants [
71]. To achieve the desired osteoinductivity and osteoconductivity properties of the orthopedic implants, zirconia-based builds must be coated with bioactive materials [
72]. One extensively studied coating material is hydroxyapatite [
73]. Such combinations are frequently utilized due to the outstanding mechanical properties of zirconia and the great bioactivity of hydroxyapatite [
67].
Despite its suitability for applications demanding high mechanical and fracture strength, zirconia does come with certain drawbacks when adapting it for VPP. Notably, its high refractive index (2.1) [
74], while advantageous for dental implants in terms of aesthetics, poses challenges in DLP technology reliant on UV light [
33]. Furthermore, zirconia’s fragility can lead to crack formation in the build, unless it is combined with various slurries [
64]. Also to be considered are the different orientations of the prints, with studies showing that orientating the 3D model at 45 degrees exhibited the greatest resistance to indentation fracture [
75].
Zirconia was adapted for DLP 3D printing due to the technique’s increased speed and accuracy in fabricating patient-specific dental parts. Data in the literature allude to the possibility of adapting zirconia for suitability with DLP printers by dispersing zirconia particles using silane as a coupling agent. However, further investigations are required to assess its performance under different physical conditions and mechanical stress [
64].
1.3. Lithium Disilicate
Lithium disilicate (Li
2Si
2O
5) is categorized as a glass–ceramic material with a biphasic polycrystalline structure [
76]. Owing to its remarkable mechanical properties and aesthetic qualities, lithium disilicate has gained prominence in the field of dental restorations [
77]. Manipulating the material with traditional techniques such as conventional restoration waxing exhibited drawbacks related to precision, accuracy, and susceptibility to human error [
78]. However, due to the high precision and speed offered by DLP 3D printing, along with advancements in 3D printing techniques [
63], such as LCM-Lithography-based Ceramics (DLP in conjunction with highly filled ceramic suspensions of photocurable resins), 3D-printed dental components made from lithium disilicate have shown promise [
79].
Although limited research has been conducted on 3D-printed lithium disilicate, it was reported that lithium disilicate is suitable in dental restorations, as it meets both the aesthetic and functional requirements for the anterior and posterior regions of the oral cavity [
78]. Dental crowns and veneers are the primary structures widely employed in this context [
79,
80,
81,
82]. A recent study showed that lithium disilicate builds overcome the limitations of metal–ceramic restorations, which have long been considered the gold standard in dental restorations [
79,
81].
In veneers, studies comparing 3D-printed parts with the manual waxing technique reported that the 3D-printed build displayed no differences in the quality of the final product regarding the marginal and internal fit. Instead, it came only with advantages, such as the ability to rigorously replicate the dental part and the accuracy and the speeds of the builds [
82,
83]. Crucial to veneer fabrication are the mechanical properties of the material used (in this case, with reported values for fracture toughness of 3.3 ± 0.3 Mpa m
1/2 [
84] and flexural strength of 280 Mpa) [
85]. Additionally, LCM lithium disilicate veneers have shown satisfactory aesthetics and an acceptable marginal fit [
79].
Several studies have demonstrated that lithium disilicate glass ceramics stand out as an excellent option for dental rehabilitation, particularly for producing monolithic crowns [
86]. Similar to veneers, 3D printing a crown is an efficient and controlled process, with fewer errors and less materials being wasted compared with traditional waxing. It was also reported that VPP techniques are more efficient than other recent methods of producing crowns and veneers, such as the subtractive CAD/CAM technique [
78]. A few analyses revealed that the lithium disilicate dental parts are adequate for patients requiring restorations with a lifespan exceeding 5 to 9 years, considering that the complication rate is usually under 20% [
80,
81].
Alongside the previously mentioned advantages, we also need to mention the challenges that occur during 3D printing and post-processing. One notable drawback is the susceptibility of builds, particularly crowns, to fracture, with posterior and molar crowns being more prone to this issue [
80]. Furthermore, the incidence of fracture presumably increases after a certain time of clinical service and also increases with the forces developed in the mastication process [
80]. Another concern arises from post-processing methods that can prolong the average manufacturing time and also make it less attractive for clinical practice; however, studies show that this limitation can be overcome by using the adapted DLP technique known as LCM [
79]. Although 3D-printed lithium disilicate has not yet received approval for definitive restorations, there is potential for achieving this milestone in the future. Flexural and bonding strength needs to be enhanced to fully apply this material in all dental applications, and the reduction of micro-fractures is needed [
79]. Furthermore, the potential for multicolor dental part printing using lithium disilicate for aesthetic purposes is also a possibility [
79].
1.4. β-Tricalcium Phosphate (β-TCP)
Tricalcium phosphate (Ca
3(PO
4)
2) exists in four different forms, the β form being relevant for this review, due to its temperature stability (below 1120 °C) and printability [
87]. With a research history spanning five decades and an annual publication output exceeding 200 papers, β-tricalcium phosphate (β-TCP) has emerged as one of the most potent biocompatible materials for bone grafts [
88]. With the development of additive manufacturing processes, the adaptation of β-TCP for 3D printing was an inevitable step. The current focus on the use of β-TCP in 3D printing is its compatibility with VPP 3D printing technology due to all the advantages that this technology brings, especially for manufacturing porous and high-strength scaffolds [
89].
Owing to its chemical composition, β-TCP exhibits a spectrum of bioactive properties, including osteoconduction (promoting osteoblast adhesion, osteoblast proliferation, and the synthesis of new extracellular matrix components [
89]); gradual biodegradation (the gradual release of ions with a therapeutic effect [
90]); osteoinductivity [
88]; and minimal cytotoxicity [
91]. Studies have revealed that pure β-TCP scaffolds may not exhibit optimal mechanical properties due to rapid degradation in vivo, which hinders the maintenance of the build integrality before the full repair of the bone defect [
92].
A recent study mentioned that, despite the pure β-TCP scaffolds in the study having a compressive strength of up to 44.7 Mpa, which is higher than the values reported in he literature for similar bioceramic scaffolds, it is essential that the ceramic framework be coated or impregnated with different biocompatible materials for enhanced properties [
89]. Still, further research is required in order to facilitate compatibility between this type of mix and VPP 3D printers.
The in vivo properties of a scaffold printed via DLP technology and consisting of β-TCP mixed with pyritum (a traditional Chinese medicine composed of iron disulfide, magnesium, zinc, copper, and other compounds and elements) were recently reported in [
90]. When compared with a pure β-TCP scaffold, tricalcium phosphate mixed with a pyritum scaffold managed to overcome the structural drawback of this build. With enhanced mechanical strength (approximately four times higher), improved osteoinductive properties (due to the presence of the elements mentioned above), and a lower rate of biodegradability regarding the scaffolds, the TCP/pyritum build holds promise as a biomaterial for bone defect repair [
90].
Other studies have investigated the potential of carrying out bone defect repairs using β-TCP scaffolds doped with different quantities of magnesium oxide, ranging from 0 to 5%. In one study, it was revealed that Mg doping improves physicochemical functions such as mechanical strength and also slows down the degradation rate of scaffolds. Also, the biological functions were improved, and the Mg-doped DLP 3D-printed scaffolds promoted the osteogenic differentiation of bone marrow stem cells and angiogenic differentiation [
92]. The study also reported that the optimal doping with magnesium oxide was 3%.
1.5. Biphasic Calcium Phosphate (BCP)
Biphasic calcium phosphate is a bioceramic that consists of a mixture of hydroxyapatite and beta-tricalcium phosphate (β-TCP) in varying ratios, with each part having a pivotal role in determining the bioactive properties of constructs fabricated using this functional biomaterial [
93]. There is a scarcity of data regarding the use of BCP in VPP 3D printing with biocompatible and functional materials. Even though numerous studies concentrate on Robocasting, FDM, or SLS 3D printing technologies, there are a limited number of papers that have explored BCP builds produced through DLP 3D printing and showed that they exhibit higher precision, accuracy, and speed [
94,
95,
96,
97], although the eventual drawbacks of DLP 3D printing using BCP also need to be studied further.
As they are composed of Hap and beta-tricalcium phosphate, BCP builds offer several bioactive properties. The osteoconductive and osteoinductive properties of Hap are crucial features that promote processes like cell migration, vascularization, and, of course, osteogenesis [
98,
99]. Beta-tricalcium phosphate is biodegradable, and its role in this type of construction is to provide calcium and phosphate ions for bone formation [
100]. With its excellent cytocompatibility and minimal cytotoxicity, this biocompatible ceramic is well suited for manufacturing various patient-specific scaffolds in order to address bone defects [
101,
102] (
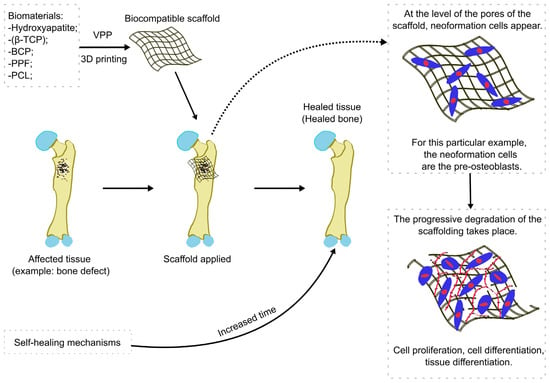
Figure 1).
Figure 1. The general process of a VPP 3D-printed biocompatible scaffold applied in bone regeneration. β-TCP = beta-tricalcium phosphate, BCP = biphasic calcium phosphate, PPF = poly(propylene fumarate, PCL = polycaprolactone.
In a recent comparative study aiming to assess how pore diameter influences bone formation in the regeneration of rabbit calvarial defects, it was determined that an optimal HA/β-TCP ratio of 60:40, along with pore diameters exceeding 300 µm enhanced vascularization and new bone formation [
98]. Another study comparing DLP 3D printing with 3D-milled PMMA (poly methyl methacrylate) showed that the DLP 3D-printed block displayed enhanced internal fit and demonstrated significantly greater contact with the defect surface. To elaborate, it had twice as much contact in flat defects and over 70% more contact in curved defects [
103].
Additionally, the morphology of the constructs can influence their bioactive properties. For instance, analyzing composite scaffolds with a gyroid structure led to the revelation that they have excellent biocompatibility, as well as enhanced cell proliferation and adhesion [
104]. The evolution of 3D additive manufacturing technology has facilitated the construction of more intricate and accurate builds, particularly in addressing patient-specific defects. Another study revealed that scaffolds incorporating oxygen-generating elements can efficiently increase oxygen levels, which is essential in preventing hypoxic cell death during the early stages of engraftment [
105]. As such, biphasic calcium phosphate coated with calcium peroxide showed great potential for promoting bone ingrowth and proliferation under a hypoxic environment [
105].
Despite the research on this topic being in its early stages, meaning that the disadvantages regarding DLP 3D printing with this material have yet to be revealed, biphasic calcium phosphate is not perfectly compatible with this type of technology and needs to be adapted. Similar to hydroxyapatite, mixing the bioceramics in a slurry made of acrylic monomers, dispersants, and photocatalysts is necessary; nevertheless, this might improve printing quality with DLP 3D technology, which, despite being a fast and precise method, can have drawbacks regarding the final form, the time of postprocessing, and the possible shrinkage of the build [
98,
102,
103,
104].
Further research is needed to investigate the in vivo effects of these structures and their biological behavior in order to expand their applications in the medical field [
101].
2. Organic Biomaterials
2.1. Poly(propylene fumarate)
Poly(propylene fumarate) (PPF) is a linear and unsaturated co-polyester characterized by its fumaric acid–base structure which has demonstrated a range of intriguing attributes in the medical field [
106]. Due to the research carried out in the past 10 years and the development of new technologies in 3D printing, the way for faster, more precise, and increasingly complex fabrications has been paved [
107]. Similar to the majority of the materials discussed in this review, slurries with various photocurable substances and minor structural adjustments are needed in order to 3D print PPF using VPP. Due to the presence of an unsaturated bond, PPF can be converted into a resin and undergo photo-crosslinking to form a VPP 3D-printable solution [
108].
Another hurdle that was overcome in the goal of adapting PPF for VPP-based 3D printing is its viscosity. The intrinsic viscosity of pure PPF at 40 °C is 120 times higher than the ideal viscosity of 200 cP in 3D printing resins [
109,
110,
111]. The lowering of the viscosity of PPF solutions was accomplished by mixing it with diethyl fumarate at various ratios, usually greater than 50% [
108,
111,
112,
113,
114,
115,
116,
117]. This ensured that the solution was printable but within the maximum limits of viscosity. Nevertheless, addressing potential defects that may arise from this approach remains an ongoing pursuit.
PPF, by itself, is not osteoinductive or osteoconductive and does not aid in bone tissue regeneration. Still, its advantageous properties, such as its great resorption, optimal degradability, low cytotoxicity, and mechanical behavior [
108,
113,
115], in combination with the feasibility of the DLP 3D printing technique, put the PPF builds at the top of the list of functional biomaterials [
116]. Studies have reported that PPF-based materials have great medical applications, including in cardiac tissue engineering, ophthalmology, and neural tissue engineering [
115], yet 3D-printed PPF-based materials are more suitable in orthopedics, specifically in bone tissue engineering [
113].
In one particular study wherein two DLP 3D-printed scaffolds made from PPF were used to repair murine cranial defects, it was observed that bone regeneration and material degradation depend on the molecular mass variation. It was stipulated that the PPF 1000 Da scaffold had the highest bone/interaction at 4 weeks due to the enhanced degradation of the polymer that facilitates a relative high inflammatory response [
108].
In order to expand PPF scaffolds to more medical applications, these builds should be enhanced with bioactive properties [
108]. However, mixing PPF with an excess of bioactive material increases the slurry viscosity and leads to printing incompatibility or defective printing. A study reported that mixing PPF with Bioglass in a range between 2.5% and 5% yielded great results in terms of surface availability and functionality, as well as cell attachment, proliferation, and osteogenic differentiation at the surface of the build [
116].
Despite being studied since 1994, the compatibility of PPF with 3D printers has not been extensively investigated [
112], particularly in regard to VPP. While the benefits of using PPF can be extrapolated from prior research, several challenges, including post-processing methods, the development of photoinitiators and solvents to create final, printable slurries [
115], and the management of defects and cracks, necessitate further investigations. Moreover, further in vivo and in vitro studies are needed to identify the optimal concentrations to fulfill the potential of PPF tissue engineering (tissue replacement/regeneration) [
115].
2.2. Polycaprolactone (PCL) Mixes and Polycaprolactone (PCL)-Based Materials
Polycaprolactone (PCL)—(C
6H
10O
2)
n—is a synthetic polymer that can be synthesized chemically by the ring-opening polymerization of ε-caprolactone. PCL presents great biocompatibility and has been approved by the United States Food and Drug Administration (FDA) for use in humans [
118,
119]. A highly used material in various 3D printing technologies such as Fused Deposition Modeling (FDM) [
120] and electrospinning [
121], there is growing interest in adapting different biocompatible materials with distinct physico-biological attributes for VPP 3D printing techniques. A prime illustration of this venture is the integration of polycaprolactone. Although few studies have reported the use of PCL in VPP 3D printing, some authors have unveiled innovative adaptations to harness PCL’s properties in conjunction with the speed and precision of VPP [
122,
123,
124,
125].
PCL is widely favored for biomedical applications due to its remarkable characteristics, which include its low degradation rate [
126], flexibility and hydrophilia [
126], anisotropic behavior [
127], antibacterial activity [
128], adequate mechanical strength and heightened extracellular matrix gene expression [
119], and biodegradability [
125]. To this day, there appears to be no studies reporting the exclusive use of pure PCL in printing using VPP techniques. Some researchers have adapted and successfully implemented the properties of PCL in DLP 3D-printed structures either by incorporating a small proportion of PCL or by using PCL-based materials [
122,
123,
124,
129].
GelMA is a biopolymer employed for the 3D fabrication of different biocompatible scaffolds; however, its mechanical drawbacks do not allow for a good printing resolution using SLA or DLP. One study showed that adding PCL in a ratio of 70/30 (GelMA-PCL) increased the resolution of printing with SLA and also stabilized the viscosity [
124]. To assess this novel resin blend and to challenge the 3D printer with the complexity of an anatomical structure, a human small intestine tissue scaffold was made. Furthermore, this material presented optimal cell adhesion, water swelling, softness, and precision, as well as reduced reabsorption, compared with the pure materials taken separately [
124].
As mentioned, PCL-based biocompatible materials have also been tested with VPP 3D printing machines. Some studies have reported the synthesis of PCL-based urethane acrylates for DLP 3D printers [
122,
123]. Following synthesis, the authors of one specific study reported that the PCL-based poly(urethane acrylates) (PUA) used for 3D-printed builds had been mixed with natural resins such as polyethylene glycol diacrylate (PEGDA) or polypropylene glycol (PPG) to obtain optimal viscosity and printability. It was determined that the optimal mix with low cytotoxicity and good printability for producing tissue engineering scaffolds is the PUA-PEGDA-PPG (70:30:0) [
122]. Moreover, in another study, waterborne polyurethanes produced from PCL in a ratio of 20% in the final mix were optimal for manufacturing bendable and flexible 3D architectures and devices via DLP 3D printing [
123].
Another study reported on the use of PCL in the realm of 4D printing, which denotes the fourth dimension as time and considers the evolving properties of the material [
129]. PCL was integrated into the scaffolds as a self-healing agent to confer this property to the system build (based on soft active materials). The study also reported drawbacks due to encountering irreparable damaged printed structures, which can lead to increased costs, but in the end, it was concluded that these types of builds have enhanced resolution, enhanced geometric complexity, and, most importantly, self-healing capabilities [
129].
In the future, PCL-based materials or mixes could be applied to cartilage scaffolds [
122]. Also, these resins may have great potential tissue engineering applications and, in the next decade, may become the base of artificial organs [
122,
123].
2.3. Poly(methyl methacrylate)
Poly(methyl methacrylate) is a widely used synthetic polymer of significant scientific interest in the field of medical technologies, with a research history spanning over eight decades. It has been acknowledged for its favorable attributes, including its ease of processing, repairability, polishability, and good biocompatibility [
130,
131,
132]. PMMA has found applications in various medical specialties, such as orthopedics (for bone cement and screw fixation in bone), ophthalmology (for contact and intraocular lens), neurosurgery (as filler for skull defects and for vertebrae stabilization), dental technologies, plastic surgery, and even keratoprosthesis [
130,
133]. With a great history regarding the methods used for manufacturing PMMA builds, from traditional ones such as pouring a fluid resin or mold-filling to more modern ones like milling blocks designed using computer-assisted design and manufacturing, the current direction is making PMMA compatible with the SLA and DLP printers [
132,
134].
Recent reports indicate that, for the moment, the mixes of PMMA compatible with VPP 3D printing techniques are for dental technologies and implants [
135,
136,
137], although a few studies have reported additional medical uses [
138]. The notable characteristics of PMMA-based constructs include their good aesthetics, physicochemical properties, low cost, excellent biocompatibility, low toxicity, reliability, and good mechanical strength [
130,
132,
133].
One approach that has been found to make PMMA compatible with VPP 3D printing techniques, namely SLA 3D printing, involves blending it with other acrylates such as ethylene glycol dimethacrylate (EGDMA) and methyl methacrylate (MMA), which also present great mechanical and biological properties [
134]. The study of Hata et al. aimed to find an optimal mixture for satisfactory printability and practicability following SLA 3D printing, and the authors concluded that the best mechanical, bonding, and physicochemical properties, as well as good cell viability, is given by a 30% PMMA, 56% EGDMA, 14% MMA mix [
134]. This particular PMMA-based resin exhibits excellent properties, suggesting its potential suitability for various dental applications, including in crowns, bridges, denture bases, and teeth [
134].
Mechanical properties are crucial in dental applications to ensure durability and resilience in patients. One study assessed the flexural strength of a DLP and SLA 3D-printed PMMA build and compared it to pieces built with a frequently used technique, namely FDM [
137]. Although DLP was the fastest method for printing PMMA, all of the produced specimens fractured into several fragments when their flexural strength was tested and compared with the other two groups. Also, the specimens based on vat polymerization exhibited increased flexural strengths but suffered from numerous cracks and fractures. As the speed and precision of DLP and SLA techniques are considerable, further studies are worth pursuing in order to improve the observed disadvantages [
135,
136,
137].
An innovative study using DLP-printed PMMA successfully built a tracheostomy tube which was later tested and functioned properly with no infections, allergies, or other reactions in rabbits [
138]. It was reported that the PMMA-resin scaffold exhibited no fiber structures, contaminations, or surface cracks and also that cell viability was higher than in the control groups. The key advantages include the precision and speed of the print, the enhanced mechanical behavior pre- and post-insertion, and the absence of cytotoxic effects and visible chemical changes in vivo [
138].
In summary, DLP-printed PMMA resins hold promise for advancing modern medical applications. However, they have been insufficiently studied, and not many future medical applications are in sight. Considering that compatibility with DLP and SLA 3D printers was just established, adequate in vivo testing is required, especially regarding cytotoxicity. Optimal mixes need to be identified in order to eliminate all the mechanical disadvantages that these materials currently present [
134,
136].
2.4. Poly(trimethylene carbonate)
Poly(trimethylene carbonate) (PTMC) is a biocompatible and biodegradable synthetic polymer that can be manufactured through the process of ring-opening polymerization (ROP) using trimethylene carbonate (TMC), a bio-derived monomer with the following chemical formula: C
4H
6O
3 [
139,
140,
141]. PTMC is categorized as an amphiphilic biocompatible copolymer that is akin to PEG, an attention-drawing compound due to its increased compatibility with the body fluids [
141]. With the development of VPP 3D printing techniques, it was concluded that PTMC is more suitable than its partner in the amphiphilic group due to superior mechanical properties and printability with DLP or SLA 3D printers [
139,
140].
Similarly to the previously mentioned materials adapted for VPP techniques, PTMC possesses noteworthy and distinctive properties, including flexibility, a low glass transition temperature of ≈ −20 °C, toughness, tear resistance, the absence of relevant cytotoxicity, softness, and great degradation activity suitable for building tissue engineering scaffolds [
139,
140,
142]. As a synthetic material, it does not present bioactivity, but some studies have revealed different ways of transforming pure PTMC into a DLP- or SLA-printable resin with bioactive and mechanical properties [
139,
142].
It was stipulated that materials prepared from macromers with molecular weights higher than 10 kg mol
−1 show enhanced mechanical properties such as high tensile strength, toughness, tear resistance, and suture retention strength [
143]. A group of researchers managed to build a PTMC DLP 3D-printed structure that exceeded the 10 kg mol
−1 molecular weight mark; specifically, it weighed 28.9 kg mol
−1 [
139]. This weight could open up new avenues in terms of the functionality of this material, mainly by making it more applicable to cases that require constructs to be subjected to great forces, such as the case with meniscus implants [
139].
Another biofunctional application is PTMC’s role in tissue engineering. In order to create a scaffold compatible with tissue engineering applications, the materials have to meet certain conditions, including being biocompatible, biodegradable, and porous while also having sufficient mechanical properties [
144]. In this case, pure PTMC is very hydrophobic, but due to its high potential in medical engineering applications, a method for adapting it to DLP printing was constructed [
142]. The reported solution was a mix between PTMC—a synthetic hydrophobic biopolymer—and gelatine (from porcine skin)—a natural hydrophilic biopolymer, in which a large quantity of solvent was added; the resulting mixed resin was manageable for tissue engineering applications and printable via VPP techniques [
142].
Very few studies have reported the use of PTMC in additive manufacturing, and even fewer have reported on using PTMC with DLP or SLA 3D printing techniques [
139,
140,
142]. As mentioned, the future of medical applications requires the printing of patient-specific builds quickly and with reduced costs. For now, DLP and SLA are the fastest methods, but they are limited by their incompatibilities with some biomaterials. Further research needs to identify new processes to adapt materials that show suitable properties for different biofunctional applications to these new, precise, and fast 3D printing technologies. Drug delivery and cell/stem cell therapy are also very promising fields for future research with this material or its mixes with various bioactive and biocompatible materials. Furthermore, thermogels have been reported as candidates in different potential laboratory applications [
139,
140].
This entry is adapted from the peer-reviewed paper 10.3390/jfb15010007