Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Vitamin D functions have been studied progressively, and along with their main role in regulating calcium homeostasis, the potential function in the nervous system and the link between different psychiatric disorders and vitamin D deficiency have been revealed. The discovery of vitamin D receptors in multiple brain structures, like the hippocampus, led to the hypothesis that vitamin D deficiency could be responsible for treatment resistance in psychiatric diseases.
- vitamin D deficiency
- mental health
- depression
1. Introduction
Since the discovery of vitamin D in 1921 and its active form, 1,25-dihydroxyvitamin D (1,25-(OH)2D) [1], in 1967, its role in bone health and calcium homeostasis has been well established. However, recent biochemical advances have increased interest in its non-skeletal function, given the prevalence of its deficit in more than 50% of commonly encountered patients in clinical practice [2].
Vitamin D can be found in two forms: ergocalciferol (Vitamin D2), created in plants such as mushrooms but also available in supplements; and cholecalciferol (Vitamin D3—the “sunshine” vitamin), obtained from skin sunlight radiation, exposure to ultraviolet B, oral supplements, and various foods (juices, milk, cereals, oily fish). After intestinal absorption, they are metabolized in the liver and kidneys, resulting in calcidiol (25-hydroxycholecalciferol), the body’s storage of vitamin D, and calcitriol (1,25-dihydroxyvitamin D), also known as the active metabolite. Thus, calcidiol is used for the measurement of total body vitamin D, with a normal range between 25 ng/mL and 80 ng/mL [3].
Vitamin D plays a pivotal role in regulating calcium and phosphorus levels within the body. Its functions are multifaceted, including the stimulation of calcium and phosphorus absorption in the intestines, mobilization of calcium from bones, and increased reabsorption of calcium in the distal tubule of the kidneys (Figure 1). Notably, these actions on bone and, to some extent, the kidneys are modulated by the parathyroid hormone [4]. One crucial aspect of the vitamin D endocrine system is its ability to establish a robust feedback mechanism. In this mechanism, 1,25(OH)2D3, an active form of vitamin D, acts to inhibit the expression of the CYP27B1 gene in the kidney. This, in turn, leads to a decrease in the production and secretion of parathyroid hormone (PTH) by the parathyroid gland and an increase in the expression of fibroblast growth factor 23 (FGF23) in the bone [5]. This intricate feedback loop is vital for maintaining the delicate balance of calcium and phosphorus in the body.
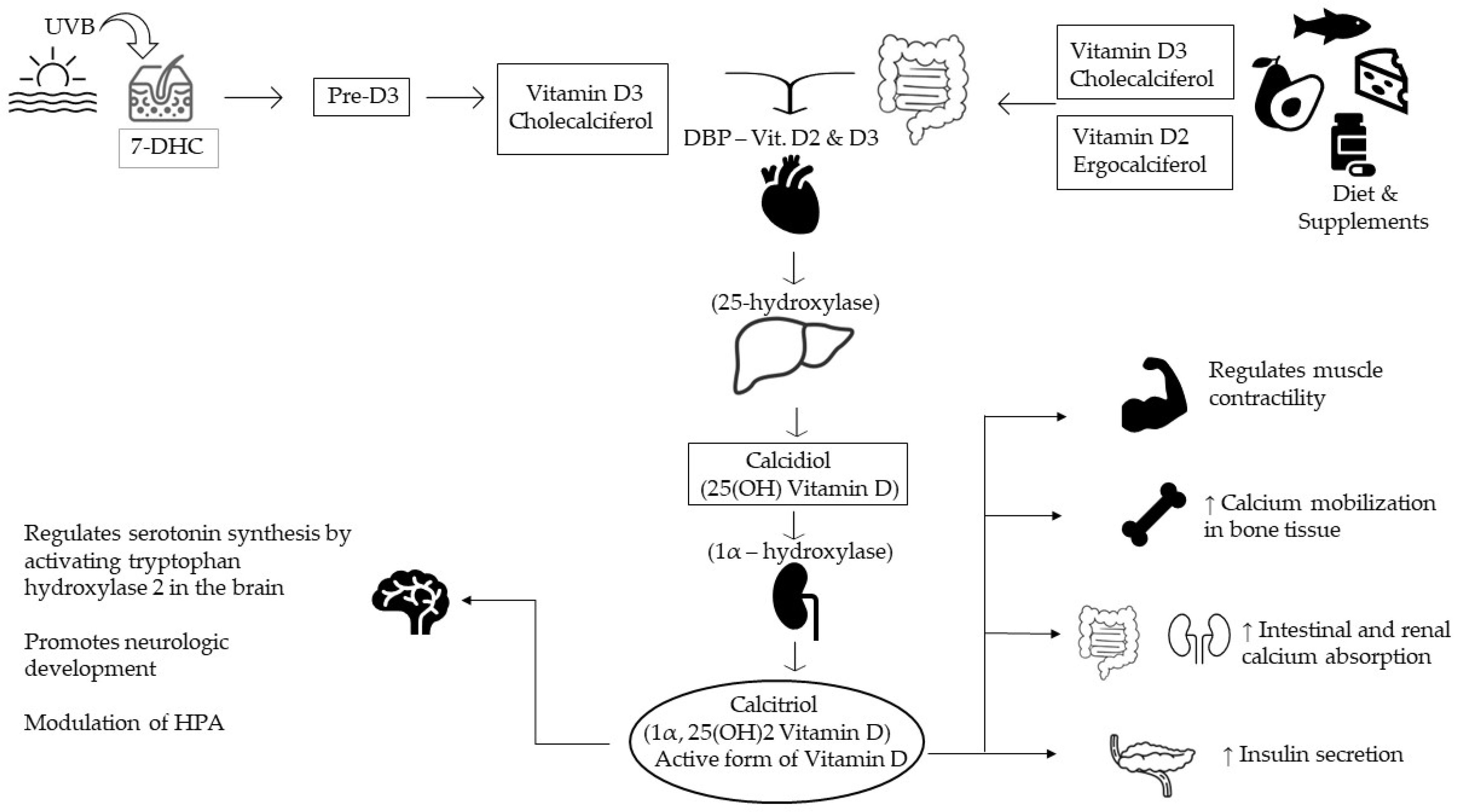
Figure 1. Vitamin D synthesis and its main functions. 7-DHC—7-dehydrocholesterol; DBP—vitamin D binding protein; HPA—hypothalamic-pituitary-adrenal axis.
In recent discoveries, vitamin D receptors have been found in the brain (hippocampus, substantia nigra, and cerebellum), which led to further explanations for their role in neurologic development, psychiatric conditions (anxiety, depression, psychoses), or behavior. An additional role could be the involvement in modulation of the hypothalamic-pituitary-adrenal axis (HPA), thus regulating the production of epinephrine, norepinephrine, and dopamine [6][7]. Thirdly, this hormone has neuroprotective effects through multiple mechanisms, such as the reduction of nitric oxide synthesis and calcium toxicity, protection of the neurons from induced cell death, antioxidant properties, and modulation of cytokine release [8]. The discovery of vitamin D receptors in the brain has prompted research into its potential role as a neuroactive steroid in regulating neurophysiological processes associated with depression [9]. Low levels of circulating vitamin D (25-hydroxyvitamin D3; 25(OH)D) have been linked to depression [10]. In the brain, vitamin D is biologically active (1,25-dihydroxyvitamin D3), and it interacts with the nuclear vitamin D receptor (VDR) and enzymes involved in its activation and metabolism. This suggests that vitamin D may have autocrine or paracrine effects on the brain [8]. It may counteract the hyperactivity of the hypothalamic-pituitary-adrenal (HPA) axis and cortisol overproduction, common in depression due to reduced glucocorticoid receptor sensitivity in the brain [11].
It has also been found that neonatal deficiencies of vitamin D in rats alter the shape and size of the brain, growth factor expression, cell proliferation, enlargement of the ventricles, and cortical thinning [7][8][9][10][11][12].
2. Psychiatric Diseases and Vitamin D
Vitamin D exhibits a remarkable ability to traverse the blood-brain barrier, activate vitamin D receptors within the central nervous system, and exert influence over human behavior regulation, as elucidated by studies such as Farhangi et al. (2017) [13]. Its role extends to the intricate modulation of neurotransmitter release and the synthesis of neurotrophic factors, pivotal mechanisms contributing to the improvement of mood and behavioral outcomes in individuals, as highlighted in the research conducted by Macova et al. (2017) [14]. This multifaceted influence can also be attributed to vitamin D’s neuroprotective properties, with evidence indicating its potential to reduce plasma C-reactive protein levels in psychiatric disorder patients and its capacity to modulate inflammation through the suppression of proinflammatory cytokines, as observed in studies like Jamilian et al. (2019) and Barker et al. (2013) [15]. These findings collectively underscore the pivotal role of vitamin D in neurological and psychiatric well-being, shedding light on its potential therapeutic implications.
After crossing the blood-brain barrier, vitamin D has implications for many processes: cell differentiation, neurotransmitter synthesis, neurotrophic production and release, calcium homeostasis, cognitive function, oxidative damage prevention, and neuronal structure-function. Therefore, it is not surprising that low vitamin levels have been associated with various psychiatric disorders (depression, schizophrenia, autism spectrum disorders, and Alzheimer’s disease [16].
Some data suggest that the psychiatric population has a higher rate of vitamin D deficiency than the general population [16][17][18][19][20][21][22][23][24][25]. Patients from a psychiatric ward in Serbia have been included in a cross-sectional design study, and a significant number of patients had a lower vitamin D level than expected [24]. Even in an equatorial nation, despite the geographic location and outdoor activities, levels of vitamin D were still low among psychiatric hospitalized subjects [23].
Vitamin D supplementation therapy in psychiatric patients had beneficial effects on depressive symptoms, biomarkers of inflammation, and even oxidative stress [26][27][28] C-reactive protein and total antioxidant levels have been improved [28].
Patients with alexithymia have been included in a study for measuring serum levels of vitamin D and genotyping vitamin D binding protein, and their results suggest that lower vitamin levels could be involved in the pathophysiology of the disease [29].
4. Neurodevelopmental Disorders
The majority of people with intellectual disabilities were reported to have deficient or insufficient vitamin D levels, with a higher prevalence in women [30]. The level of vitamin D deficiency in patients with intellectual disabilities was not correlated with seasonality, type of admission, or associated treatment [31]. Deficient levels of maternal vitamin D were not correlated with a higher risk of intellectual disability or autism spectrum disorders [32].
Deficient levels of vitamin D in newborns were not correlated with a higher risk of autism spectrum disorders [33]. Autistic children had a significantly lower level of vitamin D when compared to healthy children [34]. Vitamin D had a positive effect on irritability symptoms in autistic children [35].
Vitamin D levels were significantly lower in ADHD children and adolescents [36]. Vitamin D supplementation could improve mental health and behavioral symptoms in children with ADHD and low vitamin D levels [37]. Another study found that vitamin D supplementation in ADHD patients improved outcomes such as cognitive function, hyperactivity, and inattention.
5. Psychotic Spectrum Diseases
Epidemiologic evidence suggests that the etiology of schizophrenia includes genetic and environmental factors and common risk factors for vitamin D, including low prenatal vitamin D, children born in winter and early spring, high-altitude residents or urban residents, and dark-skinned migrants who move to cold climates [38]. Also, schizophrenia patients have poorer general health; they are less active, have a poor diet, and have an increased risk of medical conditions [39].
Recent studies have initiated vitamin D supplementation therapy as an augmented treatment to the standard regimen for schizophrenia [40][41][42]. Some of them found a negative, but not significant, association between vitamin D and different subscale scores (Positive and negative syndrome scale—PANSS), and other studies have reported improved cognition but not psychotic symptoms [40][41]. Later on, in 2021, the data obtained suggested that both antipsychotic medication and vitamin D treatment may improve positive and negative symptoms and also improve attention span [41].
6. Bipolar Disorders
Recent studies have shown that there might be a link between bipolar disorder and vitamin D deficiency [43]. There is little information concerning vitamin D levels and supplementation effects on the course of bipolar disorder; however, there has been a noted increase in 25OHD synthesis during BD decompensation [44]. Other studies have shown a lower level of vitamin D in people with bipolar disorders, but supplementation was not correlated with an improvement in depressive symptoms [45].
7. Depression
Antidepressants, as indicated by Cipriani et al. in 2018 [46], can indeed serve as a viable remedy for depression. Nevertheless, their effectiveness in addressing the condition may fall short in certain cases. Additionally, it’s not uncommon for individuals to experience a recurrence of symptoms during treatment, often necessitating multiple trials with different antidepressants before achieving a satisfactory response, as noted by Rush et al. in 2006 [47]. Therefore, it is imperative to explore supplementary treatment alternatives for individuals grappling with depression.
While the pathophysiology of depression is not yet fully understood, a deficit in vitamin D serum levels is linked to a higher likelihood of having depression, even after adjusting for confounding variables such as time of the year, socioeconomic status, and lifestyle [48]. Depression is also associated with low-grade inflammation, elevated cytokine levels, and stress-induced disruptions in lipid and glucose metabolism. Vitamin D has been proposed to act as a glucocorticoid antagonist, potentially protecting the hippocampus during HPA axis dysregulation [49]. Additionally, it may influence hippocampal neuron development, serotonin and dopamine release, and synaptic plasticity mechanisms through various pathways [50][51]. Furthermore, circulating 25(OH)D levels have been linked to the body’s immune responses [52].
The serum levels of vitamin D were correlated with the degree of depression as measured by scores such as the Hospital Anxiety and Depression Scale, with a stronger correlation in male patients as opposed to female patients [53][54]. While the correlation between vitamin D levels and depression has been studied more and more, depressive symptoms do not appear in all patients suffering from vitamin D deficiency, and not all patients with vitamin D deficiency suffer from depression, indicating a more complex pathophysiological pathway.
Vitamin D supplementation was correlated with a decrease in depressive symptoms in a variety of populations, such as elderly depressed people [55], patients with metastatic pulmonary cancer and comorbid depression [56], adolescent girls suffering from depression, and patients with acute stroke and comorbid depression [57]. Vitamin D supplementation was not correlated with a significant difference in neurotransmitters such as serotonin or oxytocin, indicating a different pathophysiological mechanism [55]. Several clinical trials have shown vitamin D supplementation to be an effective way of treating depression [58], even though when antidepressant treatment and psychotherapy are applied in an adequate scenario, the effect of vitamin D supplementation can be negligible [59][60] or at most moderate [61].
The outcomes of a comprehensive meta-analysis present compelling evidence pointing to a significant association between low circulating vitamin D levels and a notable three-fold increase in the susceptibility to post-stroke depression. Furthermore, the study underscores several other risk factors, including female gender, hyperlipidemia, and higher NIHSS scores, which were also identified as contributors to an augmented risk or occurrence of post-stroke depression. These findings illuminate the importance of considering routine screening for circulating vitamin D concentrations, not only in individuals recovering from stroke but also in other high-risk populations. Such proactive measures may aid in early identification and intervention, potentially improving mental health outcomes in these vulnerable groups, as documented in the study by Hung et al. (2023) [62].
8. Anxiety Disorder
Since epidemiological research has evidenced a relationship between vitamin D and depression, and given the usual association of depressive symptoms in patients suffering from anxiety, studies have aimed to research the therapeutic effect of vitamin D supplementation in such patients [38][63][64][65].
This current evidence shows several potential mechanisms for improvement after vitamin D supplementation, such as the role in calcium homeostasis or the interference in serotonin synthesis by expression of the serotonin synthesizing gene, therefore maintaining normal levels. Another function is the mediation of several pathways for insulin or serotonin, which are associated with mood disorders [66].
In an experiment conducted by Zhu, C. et al., approximately 160 Chinese individuals suffering from depression were subjected to supplementation with vitamin D for 6 months. There was no perceivable impact on depressive symptoms in these patients, but an improvement in anxiety symptoms [38].
In 2019, Eid, A. et al. investigated the effects of vitamin D supplementation on generalized anxiety disorder (GAD), clinically and biologically, on 30 diagnosed patients from Saudi Arabia. The individuals had serum vitamin D, serotonin, and neopterin (a mediator for cellular immunity and a biomarker of oxidative stress) measured and were divided into 2 groups (with or without vitamin D supplementation). The researchers found significant improvement in GAD patient scores in the vitamin D-treated group [63].
On the other hand, Casseb G.A.S. et al. and De Koning E.J. et al. have described ambiguous results on this matter with little association between vitamin D therapy and anxiety, independently from depression. The results showed an association between anxiety symptoms and serum vitamin D or depressive symptoms. However, the relationship between vitamin D levels and anxiety symptoms was explained by demographic and lifestyle factors such as sunlight, food, or supplements [64][65].
9. Obsessive-Compulsive Disorder
Recent investigations have shown an association between reduced vitamin D levels and obsessive-compulsive disorder (OCD) [67][68]. It is noteworthy that certain studies, despite not discerning significant differences in vitamin D levels between individuals diagnosed with OCD and healthy controls, have reported that even the healthy participants displayed vitamin D levels within the range considered a deficiency [69]. Although a pathophysiological connection between vitamin D deficiency and OCD has been posited, the precise mechanisms underlying this relationship remain elusive [70].
10. Trauma and Stress-Related Disorders
While the incidence rate for traumatic events during one’s lifetime varies between 25% and 80%, only a small group of trauma victims develop post-traumatic stress disorder (PTSD). This disease is associated with cardiovascular complications, depression, and anxiety [71]. Vitamin D may be implicated through three different mechanisms in this pathogenesis: Firstly, its neuro-inflammatory and neuro-immunological regulation may be involved with psychiatric disorders from PTSD [72]. Secondly, brain regions with altered activity in patients with PTSD express vitamin D receptors (prefrontal cortex, cingulate cortex, hypothalamus) [9]. Thirdly, vitamin D is implicated in the regulation of serotonin and catecholamine [73].
Another study investigated vitamin D supplementation during winter and the effect on biological markers of stress resilience (serotonin, cortisol, psychophysiological activity) in a randomized clinical trial. In this group, resilience to stress varied with seasonal changes in vitamin D levels (vitamin supplementation during the winter influenced resilience to stress in the spring) [74].
11. Eating Disorders
Patients suffering from eating disorders, such as anorexia nervosa (AD), have been found to present deficient levels of vitamin D [75], with some studies indicating that over half the patients have vitamin D deficiency [76]. While vitamin D deficiency is more of a result than a cause of AD, it has been suggested as a potential cause for the depressive symptoms seen in such patients [77], though this effect has been contested [78]. Vitamin D supplementation for eating disorders should be considered more on the grounds of the comorbid pathologies, such as osteoporosis, than for the eating disorder itself [79].
12. Elimination Disorders
The evaluation of urinary incontinence has led to an association between vitamin D and conditions that increase the risk for elimination disorders. Vitamin D receptors can be found in the bladder and pelvic floor muscles. Additionally, prostatic cells can express a hydroxylase that can synthesize the active form of vitamin D [80].
A recent study evaluated the relationship between vitamin D and urinary incontinence in a longitudinal observation of a cohort of older adults with a previous assessment of daily activities and cognitive and depression screening tests and found that more than half of the participants were deficient in vitamin D, and among them, 38% developed urinary incontinence. This study demonstrates the association between vitamin D and optimal pelvic floor function [81].
13. Sleep-Wake Disorders
Recent studies have shown that vitamin D levels play a role in regulating sleep patterns and, consequently, in sleep disorders [82]. Higher vitamin D levels were significantly associated with a shorter time required to fall asleep [83]. It is worth mentioning that differences in sleep patterns and duration related to vitamin D levels were only observed in daytime workers and not in nighttime workers [84]. Vitamin D deficiency has been associated with lower sleep duration and worse sleep quality in both adult and pediatric populations, with a subsequent increase in the time of sleep onset in pediatric populations, suggesting an effect of vitamin D on circadian rhythm regulation [85].
There appears to be an inverse relationship between excessive daytime sleepiness and vitamin D levels [86]. Lower levels of vitamin D have been reported in people suffering from narcolepsy with cataplexy [87]. Patients with chronic insomnia had significantly lower levels of vitamin D when compared to healthy controls [88]. Patients who were not responding to classical treatment had even lower levels of serum vitamin D when compared with treatment responders [88].
Vitamin D deficiency was present in a large proportion of patients with obstructive sleep apnea (OSA) [89]. Reduced vitamin D levels were found in pediatric patients with obstructive sleep apnea, with lower levels also observed in African American children and obese children, these factors having a cumulative effect [90]. Subjects with OSA have a higher risk of vitamin D deficiency, which is in turn independently correlated with insulin resistance in these patients [91]. Vitamin D levels are inversely correlated with OSA severity [92]. Continuous positive airway pressure (CPAP) treatment improved the clinical manifestations of OSA and vitamin D levels in obese patients [93].
14. Sexual Disorders
Among the organic causes of erectile dysfunction, vascular diseases are the most common (predominantly atherosclerosis). Low levels of vitamin D are associated with increased risk for atherosclerotic events through inflammation, endothelial dysfunction, atherosclerosis, and impaired glucose homeostasis [93].
Apart from the well-known calcium effects, several studies have conducted further analysis of the role of vitamin D levels and sexual function [94][95][96][97][98].
In a randomized, double-blind study with female participants diagnosed with sexual dysfunction and serum vitamin D deficiency, after intramuscular administration of vitamin D and evaluation of depressive symptoms, the results showed an improvement in sexual function. Furthermore, the effect of this treatment was independent of the effect on depression [95].
In comparison, another study aimed to investigate the effect of lower vitamin D levels and sexual function in men and concluded that, compared to the healthy participants, the subjects with low vitamin D obtained lower scores in erectile function, sexual desire, and orgasmic function, suggesting that low vitamin D impairs male sexual functioning, and also concluded that the degree of hypovitaminosis correlates with the severity of sexual dysfunction [96]. Canguven O. et al. conducted research with 102 male participants with vitamin D deficiency who received treatment for 12 months while being monitored. The results suggested that the treatment improved testosterone function, erectile function, and metabolic syndrome in middle-aged men [94]. Another large representative sample of U.S. men was included in a cross-sectional study where vitamin D deficiency has been associated with erectile dysfunction but is independent of atherosclerosis [97].
15. Neurocognitive Diseases
In the last 25 years, vitamin D has become a candidate for the development and function of the nervous system and a therapeutic tool [98]. Vitamin D receptors are found in the hippocampus and, therefore, play an important role in memory formation. Patients with vitamin D deficiency present with small hippocampal volumes. The active form of vitamin D supports neurotransmission, neuroprotection, and synaptic plasticity [99].
Studies have shown that patients with Alzheimer’s disease have lower concentrations of vitamin D [35][100][101][102][103][104][105]. Moreover, low serum levels of vitamin D are associated with a higher degree of cognitive impairment [106]. A 1 nmol/L decrease in serum vitamin D was associated with a 6% risk of Alzheimer’s disease [107].
Digging deeper and comparing visual with verbal memory, Kuzma E. et al. studied severe vitamin D deficiency in dementia patients and found an association with only visual memory decline [108]. In a case-control study with geriatric patients, serum vitamin D levels were tested, and a lower concentration was linked to delirium [109].
On the other hand, vitamin D has shown no protective effect on cognitive function in a 5-year follow-up study. Over the course of 5 years, 661 dementia-free patients were included in the study, and only 141 subjects developed dementia. The authors found that, among women, a 50% increase in vitamin D concentration was associated with a higher risk of dementia. In comparison, in a study with 180 patients with already-diagnosed mild cognitive impairment, a 12-month vitamin D supplementation improved cognition by reducing oxidative stress [107]. Another study showed that black participants benefited from vitamin supplementation and showed cognitive improvement in executive and attention scores [110].
This entry is adapted from the peer-reviewed paper 10.3390/medicina59122056
References
- Jones, G. 100 Years of Vitamin D: Historical aspects of vitamin D. Endocr. Connect. 2022, 11, e210594.
- Holick, M.F. Vitamin D Deficiency. N. Engl. J. Med. 2007, 357, 266–281.
- Kennel, K.A.; Drake, M.T.; Hurley, D.L. Vitamin D Deficiency in Adults: When to Test and How to Treat. Mayo Clin. Proc. 2010, 85, 752–758.
- DeLuca, H.F. The Metabolism and Functions of Vitamin D. In Steroid Hormone Resistance: Mechanisms and Clinical Aspects; Springer: Berlin/Heidelberg, Germany, 1986; pp. 361–375.
- Pike, J.W.; Christakos, S. Biology and Mechanisms of Action of the Vitamin D Hormone. Endocrinol. Metab. Clin. N. Am. 2017, 46, 815–843.
- Polak, M.; Houghton, L.; Reeder, A.; Harper, M.; Conner, T. Serum 25-Hydroxyvitamin D Concentrations and Depressive Symptoms among Young Adult Men and Women. Nutrients 2014, 6, 4720–4730.
- Yüksel, R.N.; Altunsoy, N.; Tikir, B.; Cingi Külük, M.; Unal, K.; Goka, S.; Aydemir, C.; Goka, E. Correlation between total vitamin D levels and psychotic psychopathology in patients with schizophrenia: Therapeutic implications for add-on vitamin D augmentation. Ther. Adv. Psychopharmacol. 2014, 4, 268–275.
- Kalueff, A.V.; Tuohimaa, P. Neurosteroid hormone vitamin D and its utility in clinical nutrition. Curr. Opin. Clin. Nutr. Metab. Care 2007, 10, 12–19.
- Eyles, D.W.; Smith, S.; Kinobe, R.; Hewison, M.; McGrath, J.J. Distribution of the Vitamin D receptor and 1α-hydroxylase in human brain. J. Chem. Neuroanat. 2005, 29, 21–30.
- Anglin, R.E.S.; Samaan, Z.; Walter, S.D.; McDonald, S.D. Vitamin D deficiency and depression in adults: Systematic review and meta-analysis. Br. J. Psychiatry 2013, 202, 100–107.
- Willner, P.; Scheel-Krüger, J.; Belzung, C. The neurobiology of depression and antidepressant action. Neurosci. Biobehav. Rev. 2013, 37, 2331–2371.
- Anastasiou, C.A.; Yannakoulia, M.; Scarmeas, N. Vitamin D and Cognition: An Update of the Current Evidence. J. Alzheimer’s Dis. 2014, 42, S71–S80.
- Farhangi, M.A.; Mesgari-Abbasi, M.; Nameni, G.; Hajiluian, G.; Shahabi, P. The effects of vitamin D administration on brain inflammatory markers in high fat diet induced obese rats. BMC Neurosci. 2017, 18, 81.
- Máčová, L.; Bičíková, M.; Ostatníková, D.; Hill, M.; Stárka, L. Vitamin D, Neurosteroids and Autism. Physiol. Res. 2017, 66 (Suppl. S3), S333–S340.
- Barker, T.; Martins, T.B.; Hill, H.R.; Kjeldsberg, C.R.; Dixon, B.M.; Schneider, E.D.; Henriksen, V.T.; Weaver, L.K. Circulating pro-inflammatory cytokines are elevated and peak power output correlates with 25-hydroxyvitamin D in vitamin D insufficient adults. Eur. J. Appl. Physiol. 2013, 113, 1523–1534.
- Mayne, P.E.; Burne, T.H.J. Vitamin D in Synaptic Plasticity, Cognitive Function, and Neuropsychiatric Illness. Trends Neurosci. 2019, 42, 293–306.
- Buscemi, S.; Buscemi, C.; Corleo, D.; De Pergola, G.; Caldarella, R.; Meli, F.; Randazzo, C.; Milazzo, S.; Barile, A.M.; Rosafio, G.; et al. Obesity and Circulating Levels of Vitamin D before and after Weight Loss Induced by a Very Low-Calorie Ketogenic Diet. Nutrients 2021, 13, 1829.
- Faivre, S.; Roche, N.; Lacerre, F.; Dealberto, M.-J. Vitamin D deficiency in a psychiatric population and correlation between vitamin D and CRP. Encephale 2019, 45, 376–383.
- Cuomo, A.; Maina, G.; Bolognesi, S.; Rosso, G.; Beccarini Crescenzi, B.; Zanobini, F.; Goracci, A.; Facchi, E.; Favaretto, E.; Baldini, I.; et al. Prevalence and Correlates of Vitamin D Deficiency in a Sample of 290 Inpatients with Mental Illness. Front. Psychiatry 2019, 10, 167.
- Ikonen, H.; Palaniswamy, S.; Nordström, T.; Järvelin, M.R.; Herzig, K.H.; Jääskeläinen, E.; Seppälä, J.; Miettunen, J.; Sebert, S. Vitamin D status and correlates of low vitamin D in schizophrenia, other psychoses and non-psychotic depression–The Northern Finland Birth Cohort 1966 study. Psychiatry Res. 2019, 279, 186–194.
- Jegede, O.; Gayam, V.; Gunasekara, R.; Tiongson, B.; Ishola, A.; Sidhu, J.; Virk, J.; Virk, I.; Ahmed, S.; Ojo, O.; et al. Patterns of Vitamin D Deficiency in a Community Outpatient Psychiatric Practice: A Real-World Evaluation of Treatment Gaps. Psychiatr. Q. 2020, 91, 561–570.
- Goluza, I.; Borchard, J.; Wijesinghe, N.; Wijesinghe, K.; Pai, N. To screen or not to screen? Vitamin D deficiency in chronic mental illness. Australas. Psychiatry 2018, 26, 56–59.
- Suri, T.; Suri, S.; Poremski, D.; Fang, T.; Su, A. Vitamin D deficiency in long-term hospitalization psychiatric wards in an equatorial nation. Asia-Pac. Psychiatry 2020, 12, e12390.
- Ristic, S. Vitamin D Status in Patients with Mental Disorders: A Cross-Sectional Analysis of Single Cohort from Routine Practice. Acta Endocrinol. 2017, 13, 40–46.
- Woodward, G.; Wan, J.C.M.; Viswanath, K.; Zaman, R. Serum Vitamin D and Magnesium levels in a psychiatric cohort. Psychiatr. Danub. 2019, 31 (Suppl. S3), 221–226.
- Silva, M.R.M.; Barros, W.M.A.; Silva, M.L.D.; Silva, J.M.L.D.; Souza, A.P.D.S.; Silva, A.B.J.D.; Fernandes, M.S.D.S.; Souza, S.L.D.; Souza, V.D.O.N. Relationship between vitamin D deficiency and psychophysiological variables: A systematic review of the literature. Clinics 2021, 76, e3155.
- Lerner, P.P.; Sharony, L.; Miodownik, C. Association between mental disorders, cognitive disturbances and vitamin D serum level: Current state. Clin. Nutr. ESPEN 2017, 23, 89–102.
- Jamilian, H.; Amirani, E.; Milajerdi, A.; Kolahdooz, F.; Mirzaei, H.; Zaroudi, M.; Ghaderi, A.; Asemi, Z. The effects of vitamin D supplementation on mental health, and biomarkers of inflammation and oxidative stress in patients with psychiatric disorders: A systematic review and meta-analysis of randomized controlled trials. Prog. Neuropsychopharmacol. Biol. Psychiatry 2019, 94, 109651.
- Terock, J.; Hannemann, A.; Van der Auwera, S.; Janowitz, D.; Spitzer, C.; Bonk, S.; Völzke, H.; Grabe, H.J. Posttraumatic stress disorder is associated with reduced vitamin D levels and functional polymorphisms of the vitamin D binding-protein in a population-based sample. Prog. Neuropsychopharmacol. Biol. Psychiatry 2020, 96, 109760.
- Chester, V.; Simmons, H.; Henriksen, M.; Alexander, R.T. Vitamin D deficiency in an inpatient forensic intellectual disability service. J. Intellect. Disabil. 2017, 21, 134–143.
- McKinnon, I.; Lewis, T.; Mehta, N.; Imrit, S.; Thorp, J.; Ince, C. Vitamin D in patients with intellectual and developmental disability in secure in-patient services in the North of England, UK. BJPsych Bull. 2018, 42, 24–29.
- Windham, G.C.; Pearl, M.; Poon, V.; Berger, K.; Soriano, J.W.; Eyles, D.; Lyall, K.; Kharrazi, M.; Croen, L.A. Maternal Vitamin D Levels During Pregnancy in Association With Autism Spectrum Disorders (ASD)or Intellectual Disability (ID) in Offspring; Exploring Non-linear Patterns and Demographic Sub-groups. Autism Res. 2020, 13, 2216–2229.
- Windham, G.C.; Pearl, M.; Anderson, M.C.; Poon, V.; Eyles, D.; Jones, K.L.; Lyall, K.; Kharrazi, M.; Croen, L.A. Newborn vitamin D levels in relation to autism spectrum disorders and intellectual disability: A case–control study in California. Autism Res. 2019, 12, 989–998.
- Chtourou, M.; Naifar, M.; Grayaa, S.; Hajkacem, I.; Touhemi, D.B.; Ayadi, F.; Moalla, Y. Vitamin d status in TUNISIAN children with autism spectrum disorders. Clin. Chim. Acta 2019, 493, S619–S620.
- Mazahery, H.; Conlon, C.A.; Beck, K.L.; Mugridge, O.; Kruger, M.C.; Stonehouse, W.; Camargo, C.A., Jr.; Meyer, B.J.; Jones, B.; von Hurst, P.R. A randomised controlled trial of vitamin D and omega-3 long chain polyunsaturated fatty acids in the treatment of irritability and hyperactivity among children with autism spectrum disorder. J. Steroid Biochem. Mol. Biol. 2019, 187, 9–16.
- Kotsi, E.; Kotsi, E.; Perrea, D.N. Vitamin D levels in children and adolescents with attention-deficit hyperactivity disorder (ADHD): A meta-analysis. ADHD Atten. Deficit Hyperact. Disord. 2019, 11, 221–232.
- Hemamy, M.; Pahlavani, N.; Amanollahi, A.; Islam, S.M.S.; McVicar, J.; Askari, G.; Malekahmadi, M. The effect of vitamin D and magnesium supplementation on the mental health status of attention-deficit hyperactive children: A randomized controlled trial. BMC Pediatr. 2021, 21, 178.
- Zhu, C.; Zhang, Y.; Wang, T.; Lin, Y.; Yu, J.; Xia, Q.; Zhu, P.; Zhu, D.-M. Vitamin D supplementation improves anxiety but not depression symptoms in patients with vitamin D deficiency. Brain Behav. 2020, 10, e1760.
- Cui, X.; McGrath, J.J.; Burne, T.H.J.; Eyles, D.W. Vitamin D and schizophrenia: 20 years on. Mol. Psychiatry 2021, 26, 2708–2720.
- Krivoy, A.; Onn, R.; Vilner, Y.; Hochman, E.; Weizman, S.; Paz, A.; Hess, S.; Sagy, R.; Kimhi-Nesher, S.; Kalter, E.; et al. Vitamin D Supplementation in Chronic Schizophrenia Patients Treated with Clozapine: A Randomized, Double-Blind, Placebo-controlled Clinical Trial. EBioMedicine 2017, 26, 138–145.
- Neriman, A.; Hakan, Y.; Ozge, U. The psychotropic effect of vitamin D supplementation on schizophrenia symptoms. BMC Psychiatry 2021, 21, 309.
- Sheikhmoonesi, F.; Zarghami, M.; Mamashli, S.; Yazdani Charati, J.; Hamzehpour, R.; Fattahi, S.; Azadbakht, R.; Kashi, Z.; Ala, S.; Moshayedi, M.; et al. Effectiveness of Vitamin D Supplement Therapy in Chronic Stable Schizophrenic Male Patients: A Randomized Controlled Trial. Iran. J. Pharm. Res. 2016, 15, 941–950.
- Altunsoy, N.; Yüksel, R.N.; Cingi Yirun, M.; Kılıçarslan, A.; Aydemir, Ç. Exploring the relationship between vitamin D and mania: Correlations between serum vitamin D levels and disease activity. Nord. J. Psychiatry 2018, 72, 221–225.
- Naifar, M.; Maalej Bouali, M.; Guidara, W.; Ellouze, A.S.; Jmal, K.; Omri, S.; Messedi, M.; Zouari, L.; Elleuch, A.; Maalej, M.; et al. Vulnérabilité au Trouble Bipolaire: La Piste de la Vitamine D. Can. J. Psychiatry 2020, 65, 184–192.
- Marsh, W.K.; Penny, J.L.; Rothschild, A.J. Vitamin D supplementation in bipolar depression: A double blind placebo controlled trial. J. Psychiatr. Res. 2017, 95, 48–53.
- Cipriani, A.; Furukawa, T.A.; Salanti, G.; Chaimani, A.; Atkinson, L.Z.; Ogawa, Y.; Leucht, S.; Ruhe, H.G.; Turner, E.H.; Higgins, J.P.T.; et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. Lancet 2018, 391, 1357–1366.
- Rush, A.J.; Trivedi, M.H.; Wisniewski, S.R.; Nierenberg, A.A.; Stewart, J.W.; Warden, D.; Niederehe, G.; Thase, M.E.; Lavori, P.W.; Lebowitz, B.D.; et al. Acute and Longer-Term Outcomes in Depressed Outpatients Requiring One or Several Treatment Steps: A STAR*D Report. Am. J. Psychiatry 2006, 163, 1905–1917.
- Köhnke, C.; Herrmann, M.; Berger, K. Associations of major depressive disorder and related clinical characteristics with 25-hydroxyvitamin D levels in middle-aged adults. Nutr. Neurosci. 2022, 25, 1209–1218.
- Obradovic, D.; Gronemeyer, H.; Lutz, B.; Rein, T. Cross-talk of vitamin D and glucocorticoids in hippocampal cells. J. Neurochem. 2006, 96, 500–509.
- Sabir, M.S.; Haussler, M.R.; Mallick, S.; Kaneko, I.; Lucas, D.A.; Haussler, C.A.; Whitfield, G.K.; Jurutka, P.W. Optimal vitamin D spurs serotonin: 1,25-dihydroxyvitamin D represses serotonin reuptake transport (SERT) and degradation (MAO-A) gene expression in cultured rat serotonergic neuronal cell lines. Genes. Nutr. 2018, 13, 19.
- Sedaghat, K.; Yousefian, Z.; Vafaei, A.A.; Rashidy-Pour, A.; Parsaei, H.; Khaleghian, A.; Choobdar, S. Mesolimbic dopamine system and its modulation by vitamin D in a chronic mild stress model of depression in the rat. Behav. Brain Res. 2019, 356, 156–169.
- Di Rosa, M.; Malaguarnera, M.; Nicoletti, F.; Malaguarnera, L. Vitamin D3: A helpful immuno-modulator. Immunology 2011, 134, 123–139.
- Kaviani, M.; Nikooyeh, B.; Zand, H.; Yaghmaei, P.; Neyestani, T.R. Effects of vitamin D supplementation on depression and some involved neurotransmitters. J. Affect. Disord. 2020, 269, 28–35.
- El-Salem, K.; Khalil, H.; Al-Sharman, A.; Al-Mistarehi, A.-H.; Yassin, A.; Alhayk, K.A.; Qawasmeh, M.A.; Bashayreh, S.Y.; Kofahi, R.M.; Obeidat, A.Z. Serum vitamin d inversely correlates with depression scores in people with multiple sclerosis. Mult. Scler. Relat. Disord. 2021, 48, 102732.
- Alavi, N.M.; Khademalhoseini, S.; Vakili, Z.; Assarian, F. Effect of vitamin D supplementation on depression in elderly patients: A randomized clinical trial. Clin. Nutr. 2019, 38, 2065–2070.
- McFarland, D.C.; Fernbach, M.; Breitbart, W.S.; Nelson, C. Prognosis in metastatic lung cancer: Vitamin D deficiency and depression—A cross-sectional analysis. BMJ Support. Palliat. Care 2022, 12, 339–346.
- Gu, Y.; Zhu, Z.; Luan, X.; He, J. Vitamin D status and its association with season, depression in stroke. Neurosci. Lett. 2019, 690, 99–105.
- Högberg, G.; Gustafsson, S.A.; Hällström, T.; Gustafsson, T.; Klawitter, B.; Petersson, M. Depressed adolescents in a case-series were low in vitamin D and depression was ameliorated by vitamin D supplementation. Acta Paediatr. 2012, 101, 779–783.
- Hansen, J.P.; Pareek, M.; Hvolby, A.; Schmedes, A.; Toft, T.; Dahl, E.; Nielsen, C.T. Vitamin D3 supplementation and treatment outcomes in patients with depression (D3-vit-dep). BMC Res. Notes 2019, 12, 203.
- Zhu, D.-M.; Zhao, W.; Zhang, B.; Zhang, Y.; Yang, Y.; Zhang, C.; Wang, Y.; Zhu, J.; Yu, Y. The Relationship Between Serum Concentration of Vitamin D, Total Intracranial Volume, and Severity of Depressive Symptoms in Patients with Major Deprewithe Disorder. Front. Psychiatry 2019, 10, 322.
- Shaffer, J.A.; Edmondson, D.; Wasson, L.T.; Falzon, L.; Homma, K.; Ezeokoli, N.; Li, P.; Davidson, K.W. Vitamin D Supplementation for Depressive Symptoms. Psychosom. Med. 2014, 76, 190–196.
- Hung, K.-C.; Wu, J.-Y.; Illias, A.M.; Chiu, C.-C.; Chang, Y.-J.; Liao, S.-W.; Wang, K.-F.; Chen, I.-W.; Sun, C.-K. Association of a low vitamin D status with risk of post-stroke depression: A meta-analysis and systematic review. Front. Nutr. 2023, 10, 1142035.
- Eid, A.; Khoja, S.; AlGhamdi, S.; Alsufiani, H.; Alzeben, F.; Alhejaili, N.; Tayeb, H.O.; Tarazi, F.I. Vitamin D supplementation ameliorates severity of generalized anxiety disorder (GAD). Metab. Brain Dis. 2019, 34, 1781–1786.
- GCasseb, A.S.; Kaster, M.P.; Rodrigues, A.L.S. Potential Role of Vitamin D for the Management of Depression and Anxiety. CNS Drugs 2019, 33, 619–637.
- De Koning, E.J.; Verweij, L.; Lips, P.; Beekman, A.T.F.; Comijs, H.C.; van Schoor, N.M. The relationship between serum 25(OH)D levels and anxiety symptoms in older persons: Results from the Longitudinal Aging Study Amsterdam. J. Psychosom. Res. 2017, 97, 90–95.
- Berridge, M.J. Vitamin D and Depression: Cellular and Regulatory Mechanisms. Pharmacol. Rev. 2017, 69, 80–92.
- Esnafoğlu, E.; Yaman, E. Vitamin B12, folic acid, homocysteine and vitamin D levels in children and adolescents with obsessive compulsive disorder. Psychiatry Res. 2017, 254, 232–237.
- Celik, G.; Tas, D.; Tahiroglu, A.; Avci, A.; Yuksel, B.; Cam, P. Vitamin D Deficiency in Obsessive–Compulsive Disorder Patients with Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections: A Case Control Study. Noro Psikiyatr. Ars. 2016, 53, 33–37.
- Yazici, K.U.; Yazici, I.P.; Ustundag, B. Vitamin D levels in children and adolescents with obsessive compulsive disorder. Nord. J. Psychiatry 2018, 72, 173–178.
- Celik, G.; Tas, D.A.; Varmıs, D.A.; Tahiroglu, A. Avci. Vitamin D insufficiency in a boy with obsessive–compulsive disorder. Pediatr. Int. 2016, 58, 646–648.
- Brady, K.T.; Killeen, T.K.; Brewerton, T.; Lucerini, S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J. Clin. Psychiatry 2000, 61 (Suppl. S7), 22–32.
- Furtado, M.; Katzman, M.A. Neuroinflammatory pathways in anxiety, posttraumatic stress, and obsessive compulsive disorders. Psychiatry Res. 2015, 229, 37–48.
- Kaneko, I.; Sabir, M.S.; Dussik, C.M.; Whitfield, G.K.; Karrys, A.; Hsieh, J.-C.; Haussler, M.R.; Meyer, M.B.; Pike, J.W.; Jurutka, P.W. 1,25-Dihydroxyvitamin D regulates expression of the tryptophan hydroxylase 2 and leptin genes: Implication for behavioral influences of vitamin D. FASEB J. 2015, 29, 4023–4035.
- Hansen, A.L.; Ambroziak, G.; Thornton, D.; Mundt, J.C.; Kahn, R.E.; Dahl, L.; Waage, L.; Kattenbraker, D.; Araujo, P.; Murison, R.; et al. Vitamin D Supplementation during Winter: Effects on Stress Resilience in a Randomized Control Trial. Nutrients 2020, 12, 3258.
- Veronese, N.; Solmi, M.; Rizza, W.; Manzato, E.; Sergi, G.; Santonastaso, P.; Caregaro, L.; Favaro, A.; Correll, C.U. Vitamin D status in anorexia nervosa: A meta-analysis. Int. J. Eat. Disord. 2015, 48, 803–813.
- Hanachi, M.; Dicembre, M.; Rives-Lange, C.; Ropers, J.; Bemer, P.; Zazzo, J.-F.; Poupon, J.; Dauvergne, A.; Melchior, J.-C. Micronutrients Deficiencies in 374 Severely Malnourished Anorexia Nervosa Inpatients. Nutrients 2019, 11, 792.
- Tasegian, A.; Curcio, F.; Dalla Ragione, L.; Rossetti, F.; Cataldi, S.; Codini, M.; Ambesi-Impiombato, F.S.; Beccari, T.; Albi, E. Hypovitaminosis D3, Leukopenia, and Human Serotonin Transporter Polymorphism in Anorexia Nervosa and Bulimia Nervosa. Mediat. Inflamm. 2016, 2016, 8046479.
- Modan-Moses, D.; Levy-Shraga, Y.; Pinhas-Hamiel, O.; Kochavi, B.; Enoch-Levy, A.; Vered, I.; Stein, D. High prevalence of vitamin D deficiency and insufficiency in adolescent inpatients diagnosed with eating disorders. Int. J. Eat. Disord. 2015, 48, 607–614.
- Velickovic, K.M.C.; Makovey, J.; Abraham, S.F. Vitamin D, bone mineral density and body mass index in eating disorder patients. Eat. Behav. 2013, 14, 124–127.
- Crescioli, C.; Morelli, A.; Adorini, L.; Ferruzzi, P.; Luconi, M.; Vannelli, G.B.; Marini, M.; Gelmini, S.; Fibbi, B.; Donati, S.; et al. Human Bladder as a Novel Target for Vitamin D Receptor Ligands. J. Clin. Endocrinol. Metab. 2005, 90, 962–972.
- Vaughan, C.P.; Tangpricha, V.; Motahar-Ford, N.; Goode, P.S.; Burgio, K.L.; Allman, R.M.; Daigle, S.G.; Redden, D.T.; Markland, A.D. Vitamin D and incident urinary incontinence in older adults. Eur. J. Clin. NutR 2016, 70, 987–989.
- Stumpf, E.; O’Brien, L.P. 1,25(OH)2 vitamin D3 sites of action in the brain. Histochemistry 1987, 87, 393–406.
- Shiue, I. Low vitamin D levels in adults with longer time to fall asleep: US NHANES, 2005–2006. Int. J. Cardiol. 2013, 168, 5074–5075.
- Lee, H.J.; Choi, H.; Yoon, I.-Y. Impacts of serum vitamin D levels on sleep and daytime sleepiness according to working conditions. J. Clin. Sleep. Med. 2020, 16, 1045–1054.
- Al-Shawwa, B.; Ehsan, Z.; Ingram, D.G. Vitamin D and sleep in children. J. Clin. Sleep. Med. 2020, 16, 1119–1123.
- McCarty, D.E.; Reddy, A.; Keigley, Q.; Kim, P.Y.; Marino, A.A. Vitamin D, Race, and Excessive Daytime Sleepiness. J. Clin. Sleep. Med. 2012, 8, 693–697.
- Carlander, B.; Puech-Cathala, A.M.; Jaussent, I.; Scholz, S.; Bayard, S.; Cochen, V.; Dauvilliers, Y. Low Vitamin D in Narcolepsy with Cataplexy. PLoS ONE 2011, 6, e20433.
- Zhao, K.; Luan, X.; Liu, Y.; Tu, X.; Chen, H.; Shen, H.; Qiu, H.; Zhu, Z.; He, J. Low serum 25-hydroxyvitamin D concentrations in chronic insomnia patients and the association with poor treatment outcome at 2 months. Clin. Chim. Acta 2017, 475, 147–151.
- Bouloukaki, I.; Tsiligianni, I.; Mermigkis, C.; Bonsignore, M.R.; Markakis, M.; Pataka, A.; Steiropoulos, P.; Ermidou, C.; Alexaki, I.; Tzanakis, N.; et al. Vitamin D deficiency in patients evaluated for obstructive sleep apnea: Is it associated with disease severity? Sleep Breath. 2021, 25, 1109–1117.
- Kheirandish-Gozal, L.; Peris, E.; Gozal, D. Vitamin D levels and obstructive sleep apnoea in children. Sleep Med. 2014, 15, 459–463.
- Fan, Z.; Cao, B.; Long, H.; Feng, L.; Li, Q.; Zhang, Y.; Li, T. Independent association of vitamin D and insulin resistance in obstructive sleep apnea. Ann. Endocrinol. 2019, 80, 319–323.
- Kerley, C.P.; Hutchinson, K.; Bolger, K.; McGowan, A.; Faul, J.; Cormican, L. Serum Vitamin D Is Significantly Inversely Associated with Disease Severity in Caucasian Adults with Obstructive Sleep Apnea Syndrome. Sleep 2016, 39, 293–300.
- Liguori, C.; Izzi, F.; Mercuri, N.B.; Romigi, A.; Cordella, A.; Tarantino, U.; Placidi, F. Vitamin D status of male OSAS patients improved after long-term CPAP treatment mainly in obese subjects. Sleep Med. 2017, 29, 81–85.
- Canguven, O.; Talib, R.A.; El Ansari, W.; Yassin, D.-J.; Al Naimi, A. Vitamin D treatment improves levels of sexual hormones, metabolic parameters and erectile function in middle-aged vitamin D deficient men. Aging Male 2017, 20, 9–16.
- Jalali-Chimeh, F.; Gholamrezaei, A.; Vafa, M.; Nasiri, M.; Abiri, B.; Darooneh, T.; Ozgoli, G. Effect of Vitamin D Therapy on Sexual Function in Women with Sexual Dysfunction and Vitamin D Deficiency: A Randomized, Double-Blind, Placebo Controlled Clinical Trial. J. Urol. 2019, 201, 987–993.
- Krysiak, R.; Szwajkosz, A.; Okopień, B. The effect of low vitamin D status on sexual functioning and depressive symptoms in apparently healthy men: A pilot study. Int. J. Impot. Res. 2018, 30, 224–229.
- Farag, Y.M.K.; Guallar, E.; Zhao, D.; Kalyani, R.R.; Blaha, M.J.; Feldman, D.I.; Martin, S.S.; Lutsey, P.L.; Billups, K.L.; Michos, E.D. Vitamin D deficiency is independently associated with greater prevalence of erectile dysfunction: The National Health and Nutrition Examination Survey (NHANES) 2001–2004. Atherosclerosis 2016, 252, 161–167.
- Crafa, A.; Cannarella, R.; Condorelli, R.A.; La Vignera, S.; Calogero, A.E. Is There an Association Between Vitamin D Deficiency and Erectile Dysfunction? A Systematic Review and Meta-Analysis. Nutrients 2020, 12, 1411.
- Beauchet, O.; Cooper-Brown, L.A.; Allali, G. Vitamin D Supplementation and Cognition in Adults: A Systematic Review of Randomized Controlled Trials. CNS Drugs 2021, 35, 1249–1264.
- Bivona, G.; Lo Sasso, B.; Gambino, C.M.; Giglio, R.V.; Scazzone, C.; Agnello, L.; Ciaccio, M. The Role of Vitamin D as a Biomarker in Alzheimer’s Disease. Brain Sci. 2021, 11, 334.
- Landel, V.; Annweiler, C.; Millet, P.; Morello, M.; Féron, F. Vitamin D, Cognition and Alzheimer’s Disease: The Therapeutic Benefit is in the D-Tails. J. Alzheimer’s Dis. 2016, 53, 419–444.
- Da Rosa, M.I.; Beck, W.O.; Colonetti, T.; Budni, J.; Falchetti, A.C.B.; Colonetti, L.; Coral, A.S.; Meller, F.O. Association of vitamin D and vitamin B12 with cognitive impairment in elderly aged 80 years or older: A cross-sectional study. J. Hum. Human. Nutr. Diet. 2019, 32, 518–524.
- Sultan, S.; Taimuri, U.; Basnan, S.A.; Ai-Orabi, W.K.; Awadallah, A.; Almowald, F.; Hazazi, A. Low Vitamin D and Its Association with Cognitive Impairment and Dementia. J. Aging Res. 2020, 2020, 6097820.
- Littlejohns, T.J.; Kos, K.; Henley, W.E.; Kuma, E.; Llewellyn, D.J. Vitamin D and Dementia. J. Prev. Alzheimers Dis. 2015, 3, 43–52.
- Aspell, N.; Lawlor, B.; O’Sullivan, M. Is there a role for vitamin D in supporting cognitive function as we age? Proc. Nutr. Soc. 2018, 77, 124–134.
- Al-Amin, M.; Bradford, D.; Sullivan, R.K.P.; Kurniawan, N.D.; Moon, Y.; Han, S.-H.; Zalesky, A.; Burne, T.H.J. Vitamin D deficiency is associated with reduced hippocampal volume and disrupted structural connectivity in patients with mild cognitive impairment. Hum. Brain Mapp. 2019, 40, 394–406.
- Yang, T.; Wang, H.; Xiong, Y.; Chen, C.; Duan, K.; Jia, J.; Ma, F. Vitamin D Supplementation Improves Cognitive Function Through Reducing Oxidative Stress Regulated by Telomere Length in Older Adults with Mild Cognitive Impairment: A 12-Month Randomized Controlled Trial. J. Alzheimer’s Dis. 2020, 78, 1509–1518.
- Kuźma, E.; Soni, M.; Littlejohns, T.J.; Ranson, J.M.; van Schoor, N.M.; Deeg, D.J.H.; Comijs, H.; Chaves, P.H.M.; Kestenbaum, B.R.; Kuller, L.H.; et al. Vitamin D and Memory Decline: Two Population-Based Prospective Studies. J. Alzheimer’s Dis. 2016, 50, 1099–1108.
- Chouët, J.; Sacco, G.; Karras, S.N.; Llewellyn, D.J.; Sánchez-Rodríguez, D.; Annweiler, C. Vitamin D and Delirium in Older Adults: A Case-Control Study in Geriatric Acute Care Unit. Front. Neurol. 2020, 11, 34.
- Kang, J.H.; Vyas, C.M.; Okereke, O.I.; Ogata, S.; Albert, M.; Lee, I.-M.; D’Agostino, D.; Buring, J.E.; Cook, N.R.; Grodstein, F.; et al. Effect of vitamin D on cognitive decline: Results from two ancillary studies of the VITAL randomized trial. Sci. Rep. 2021, 11, 23253.
This entry is offline, you can click here to edit this entry!
