Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Pharmacology & Pharmacy
Sparse and conflicting evidence exists regarding the localization, expression, and regulation of phase II drug-metabolizing enzymes and drug transporters across gestational stages. To resolve the uncertainties and assumptions in current knowledge, additional pharmacokinetic (PK) data and clinical pharmacology research are required to understand drug metabolism and transport in the pregnant woman and in the placenta. This comprehensive review aims to summarize the existing knowledge of drug metabolism and transport during pregnancy, aid incorporation of enzyme and transporter changes into physiologically based pharmacokinetic (PBPK) models, and inform predictions of PK changes in the pregnant population, especially as Sponsors and Regulators seek to serve this population in drug development programs.
- pregnancy
- placenta
- gestational change
- phase II enzyme
- drug transporter
1. Introduction
Physiological changes during pregnancy affect drug pharmacokinetics (PK), including absorption, distribution, metabolism, and elimination [1]. PK changes that affect the activity of drug-metabolizing enzymes and drug transporters can differ in each pregnancy trimester [2]. These gestational changes inform the selection of safe and effective drug doses for pregnant patients and guide the decision to conduct appropriate dose monitoring during pregnancy. Approximately 81% of pregnant women take at least one prescription or over-the-counter medication during gestation, excluding vitamins and dietary supplements [3]. Despite the high prevalence of medication use during pregnancy, most medications are administered “off-label” to pregnant patients, with doses based on PK data from nonpregnant individuals [4]. With limited clinical trials conducted in the pregnant population, PK changes during pregnancy are poorly characterized and optimal dose regimens for pregnant patients are insufficiently investigated [5].
Physiologically based pharmacokinetic (PBPK) modeling is an increasingly used method for predicting drug exposure during pregnancy [5]. Utilizing mathematical equations, PBPK models incorporate known physiological changes into a mechanistic model that describes drug PK [6]. Informed pregnancy PBPK models may support the evaluation of PK data in the pregnant population, guide the proposal of safe and effective doses for clinical drug development programs, and supplement clinical pharmacology studies during regulatory approval [7]. One aspect of PBPK model predictions is informed by adequate knowledge of gestational changes in drug-metabolizing enzymes and drug transporters; for instance, knowledge of these gestational changes may inform the robust prediction of drug renal clearance, systemic exposure, and their changes across pregnancy trimesters [6]. However, due to sparse or conflicting data, the gestational changes of only a small number of phase II enzymes and drug transporters have been incorporated into PBPK modeling software. The current gaps in knowledge emphasize the need to study changes in phase II enzymes and drug transporters across gestational trimesters.
Several literature reviews have been published that examine changes in enzyme and/or transporter expression in the pregnant woman and in the placenta. Gestational changes in select phase II enzymes and renal drug transporters have been elucidated through pharmacokinetic analysis of probe drugs administered during pregnancy [8,9]. Additional evidence suggests that drug-metabolizing enzymes and drug transporters in the placenta largely affect fetal drug exposure [10], but the lack of available or consistent information regarding gestational changes in some placental transporters necessitates further research [11]. Transcription factors, steroid hormones, genetic variations, and pregnancy complications have also been observed to change the expression of placental drug transporters [12,13].
2. Placenta
The human placenta links the fetus to the mother, providing nutrients to and removing wastes from the fetal circulation [14]. In addition to its function of supporting fetal metabolism, the placenta may play a fetoprotective role by extruding xenobiotics, such as drugs, from the fetal circulation.
2.1. Placental Anatomy
The human placenta possesses a hemochorial structure, in which the fetal tissue directly contacts maternal blood [15]. The fetal tissue consists of syncytiotrophoblasts, cytotrophoblasts, and vascular endothelial cells, of which the syncytiotrophoblast cells are the main barrier to drug transport [14,15]. The syncytiotrophoblasts comprise a maternal-facing brush border membrane (i.e., apical membrane) and a fetal-facing basal membrane (i.e., basolateral membrane) [14]. The apical membrane constitutes the main site of exchange for drugs, nutrients, and endogenous molecules between the maternal and fetal circulation, while the basolateral membrane provides structural attachment to cytotrophoblasts or fetal connective tissue, which houses the fetal capillaries [14,16]. Molecules are transported from the maternal uterine vasculature, across the apical and basolateral membranes of the syncytiotrophoblasts, through the fetal endothelium, and to the fetal circulation [1].
2.2. Placental Drug Transport
Both passive diffusion and transporter-mediated transfer are involved in the transport of drug molecules across the placental syncytiotrophoblast [16]. The rate of passive diffusion of a drug can be affected by its molecular weight, pKa, and/or lipophilicity [17]. In general, drugs of high molecular weight demonstrate limited passive transport across the placenta. Drugs that are unionized at physiological pH tend to diffuse across the placental membrane more easily than drugs that are ionized. Passive diffusion is also a common transport mechanism for lipophilic drugs [16].
Drug transporters are membrane proteins that efflux or influx endogenous and exogenous substances [15], offering an alternative mechanism of transport for drug substrates that do not easily diffuse across the placental syncytiotrophoblast [16]. For substrates of multiple drug transporters, the net direction of transport is determined by the relative abundance of each transporter, the affinity of the drug for each transporter, and the mechanisms that regulate transporter activity [14]. The localization of select placental drug transporters and the directionality of their transport are illustrated in Figure 1. A description of each drug transporter family is detailed in subsequent sections.
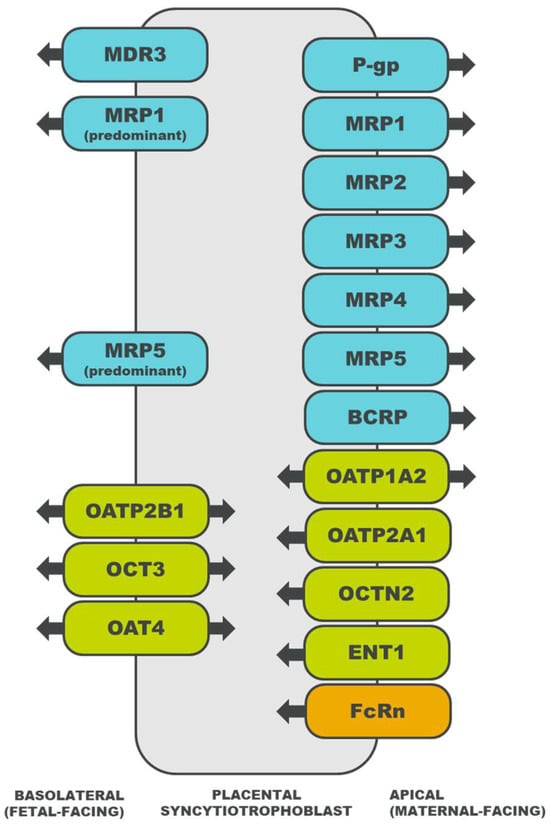
Figure 1. Localization of drug transporters in the placental syncytiotrophoblast and the directionality of their transport [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36]. ATP-binding cassette (ABC) transporters are depicted in blue, solute carrier (SLC) transporters in green, and an immunoglobulin transporter in orange. MDR, multidrug resistance protein; P-gp, P-glycoprotein; MRP, multidrug resistance associated protein; BCRP, breast cancer resistance protein; OATP, organic anion transporting polypeptide; OCT, organic cation transporter; OCTN, organic cation/carnitine transporter; OAT, organic anion transporter; ENT, equilibrative nucleoside transporter; and FcRn, neonatal Fc receptor.
3. Drug Transporters
3.1. ATP-Binding Cassette Superfamily
Transporters belonging to the ABC superfamily utilize ATP hydrolysis to efflux drugs from cells [15,37]. ABC transporters participate in the final steps of drug PK [38], including drug excretion by the liver or kidney and drug secretion by the placenta.
3.1.1. Multidrug Resistance Protein (MDR) Family
MDR1, alternatively known as P-glycoprotein (P-gp), is the most widely studied transporter within the MDR protein family (ABCB gene family) [10]. Located in the liver, kidney, intestine, and brain, MDR transporters facilitate the secretion of substrates from cells [15]. The placental MDR1, MDR3, and bile salt export pump (BSEP) may limit fetal exposure to toxic and nontoxic compounds [39,40].
3.1.2. Multidrug Resistance-Associated Protein (MRP) Family
Transporters in the MRP protein family (ABCC gene family) are expressed in various tissues, including the liver, kidney, intestine, and brain [41]. The MRP transporters export anionic drugs, as well as their sulfate, glucuronate, and glutathione metabolites. Placental MRP1 [14], MRP2 [22], MRP3 [23], and MRP5 [25] also efflux anionic and/or conjugated substrates, and the direction of transport to or from the fetal circulation depends on the transporter’s localization in the basolateral or apical membrane (Figure 1) [14].
3.1.3. Breast Cancer Resistance Protein (BCRP)
BCRP belongs to the ABCG gene family, with protein expression identified in the liver, kidney, intestine, and lung [14]. Though it can transport charged drugs and glucuronated metabolites [14], BCRP demonstrates a preference for the transport of sulfate conjugates [42]. In the placenta, BCRP effluxes xenobiotics [26], sulfated steroids [29], and bile acids [43] from the fetal circulation, which may confer protection to the fetus [42].
3.2. Solute Carrier Superfamily
Transporters belonging to the SLC superfamily influx drugs into cells via secondary active transport (e.g., antiport or symport) and passive transport (e.g., uniport) [37,38]. SLC transporters enable various processes of drug PK [38], such as drug absorption across the luminal membrane of enterocytes and drug distribution across the apical membrane of placental syncytiotrophoblasts.
3.2.1. Organic Anion-Transporting Polypeptide (OATP) Family
The OATP transporters, encoded by the SLC21/SLCO genes, are expressed in the liver, kidney, intestine, and brain [44]. OATP substrates include amphipathic organic compounds, such as drugs, bile acids, steroids, hormones, and peptides. OATP-mediated uptake may work in concert with ABC-mediated efflux [44], an interaction that has also been observed between placental transporters, including OATP2B1 and BCRP [29].
3.2.2. Organic Cation Transporter (OCT) Family
Transporters in the OCT family are encoded by the SLC22 genes [16]. OCT1 is largely expressed in the liver, OCT2 in the kidney, and OCT3 in the central nervous system and placenta; there is minimal overlap in tissue distribution between members of the OCT family [45]. OCTs enable the passive uptake of organic cations, which is coupled with cellular efflux facilitated by a different transporter on the opposite cellular membrane [16]. In addition to transporting cationic compounds, placental OCT3 also exhibits a high affinity for monoamines [30].
3.2.3. Organic Cation/Carnitine Transporter (OCTN) Family
The OCTN transporters, encoded by the SLC22 genes, have been identified in the liver, kidney, and intestine [45]. OCTNs transport cationic substrates and carnitine [44]. As carnitine influx transporters, placental OCTNs may function to supply carnitine for fetal development and placental metabolism [16].
3.2.4. Organic Anion Transporter (OAT) Family
Among the transporters in the OAT or SLC22 family, OAT1 and OAT3 have been widely studied due to their importance in drug transport [45]. Observed in the liver, kidney, intestine, central nervous system, skeletal muscle, heart, lung, pancreas, and adrenal gland, OATs are anion exchangers that pair the uptake of an anionic substrate with the efflux of another anion [44]. Though OAT1-3 are predominantly expressed in excretory organs [16], OAT4 mediates the transport of anions [27] and the uptake of estrogen precursors [46] in the placenta.
3.2.5. Concentrative Nucleoside Transporter (CNT) Family
CNTs are members of the SLC28 gene family and aid in the transport of nucleotides, nucleosides, and nucleoside analogs [47]. CNTs contribute to the biosynthesis, absorption, metabolism, and elimination of nucleotides in the brain, intestine, liver, and kidney, respectively [48]. Though limited expression of CNTs occurs in the placenta [34], CNT1 has been speculated to supply pyrimidine nucleosides for placental development [16].
3.2.6. Equilibrative Nucleoside Transporter (ENT) Family
ENTs are members of the SLC29 gene family, facilitating the transport of nucleosides, nucleobases, and monoamines [47]. Like CNTs, ENTs have been identified in the brain, intestine, liver, and kidney [34,48]. While ENT expression has been observed in the placenta, it is unclear whether these transporters are functional [34].
3.2.7. Multidrug and Toxin Extrusion (MATE) Family
The MATE transporters, encoded by the SLC47 genes, efflux organic cations from cells, often in tandem with the influx activity of OCTs [44]. MATE1 is expressed in the liver, kidney, skeletal muscle, and adrenal gland. MATE2 has two additional protein variants, MATE2-B and MATE2-K, with MATE2-K specifically expressed in the kidney. Based upon the observed interaction between MATE1 and OCT3 in the rat placenta, coupled transport of organic cations is also predicted to occur in the human placenta [49].
3.3. Neonatal Fc Receptor (FcRn)
FcRn is an immunoglobulin G (IgG) receptor that is distributed in the liver, kidney, lung, and skin [50]. In the placenta, FcRn mediates the transplacental transport of IgG from the mother to the fetus (Figure 1) [36]. As suggested with in vitro experiments, the mechanism of IgG transport involves endocytosis of the IgG–FcRn complex into acidic endosomes, transcytosis of the complex to the opposite membrane, and pH-triggered dissociation of the complex upon membrane fusion [51,52]. In addition to facilitating the transplacental transfer of IgG, the FcRn system may also enable the transplacental transport of monoclonal antibodies, which may increase fetal drug exposure or necessitate therapeutic drug monitoring during pregnancy [53].
4. Phase II Enzymes
4.1. Methyltransferase (MT) Superfamily
MTs transfer a methyl group from a donor molecule to a substrate [54,55] and are located in cells of the liver, kidney, intestine, brain, and blood [56]. In the placenta, MTs may affect the homeostasis of the human chorionic gonadotropin (HCG) hormone [54] and may contribute to placental and embryonic development [55].
4.2. Glutathione S-Transferase (GST) Superfamily
Enzymes in the GST superfamily catalyze the conjugation of glutathione moieties to xenobiotic electrophiles or reactive oxygen species [57]. GSTs are distributed in the liver, kidney, intestine, brain, heart, lung, pancreas, and spleen [58]. Placental GSTs detoxify and bioactivate xenobiotics [57].
4.3. N-Acetyltransferase (NAT) Superfamily
NATs transfer an acetyl group to a nitrogen acceptor of primary arylamines and hydrazines [59]. The NAT superfamily includes N-acetyltransferase 1 (NAT1), which is expressed in the intestine, bladder, and breast, and N-acetyltransferase 2 (NAT2), which is expressed in the liver and intestine [60]. Both NAT1 and NAT2 are expressed in the placenta, with NAT1 providing a greater contribution to placental acetylation capacity [59].
4.4. Sulfotransferase (SULT) Superfamily
Enzymes in the SULT superfamily catalyze the sulfonation of endogenous substrates and xenobiotics [56]. SULTs have been identified in cells of the liver, kidney, intestine, brain, blood, lung, adrenal gland, breast, endometrium, and ovary, though tissue distribution varies between SULT subfamilies. Placental SULTs catalyze the biotransformation of estrogens to regulate intracellular steroid concentrations [10,61].
4.5. UDP-Glucuronosyltransferase (UGT) Superfamily
UGTs catalyze the addition of glucuronic acid to endogenous substrates and hydrophobic drug molecules, forming β-D-glucuronide metabolites [62]. Though mostly distributed in the liver, UGTs have also been observed in the gastrointestinal tract, kidney, brain, lung, pancreas, breast, and nasal epithelium. In the placenta, UGTs may participate in the metabolism of steroid substrates, thyroid hormones, and bile acids [63].
This entry is adapted from the peer-reviewed paper 10.3390/pharmaceutics15112624
This entry is offline, you can click here to edit this entry!
