Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Cardiac & Cardiovascular Systems
Dual antiplatelet therapy (DAPT), comprising aspirin and a P2Y12 receptor inhibitor, is the cornerstone of post-percutaneous coronary intervention treatment to prevent stent thrombosis and reduce the risk of adverse cardiovascular events.
- dual antiplatelet therapy
- percutaneous coronary intervention
- acute coronary syndrome
1. Introduction to the Rationale of Antiplatelet Therapy after Coronary Stenting
Percutaneous coronary intervention (PCI), especially with the availability of new drug-eluting stent (DES) technologies and new devices and drugs, has revolutionized the management of coronary artery disease (CAD) by providing effective revascularization and improving clinical outcomes [1,2,3,4,5,6]. Despite these achievements, CAD still represents the leading cause of mortality in developed countries [7,8] and the outcome is still unsatisfactory in high-risk patients [9,10,11]. Therefore, great attention has been paid so far to the identification of new risk factors [12,13,14,15] and implementation of primary and secondary prevention [16,17,18,19]. Antiplatelet therapies represent a keystone in secondary cardiovascular prevention. In fact, dual antiplatelet therapy (DAPT), comprising aspirin and a P2Y12 receptor inhibitor, is a cornerstone therapy in both elective and Acute Coronary Syndrome (ACS) patients treated by PCI and stenting, to prevent both stent thrombosis (ST) and ischemic events of other vascular segments, as it is well known that platelet adhesion, activation, and aggregation play a crucial role in the pathogenesis of vascular thrombosis [16].
Aspirin is still widely considered the “primary agent” for the treatment of acute or chronic coronary syndrome to which additional antiplatelet drugs are added when a more intense antithrombotic effect is needed (Figure 1). Its antithrombotic action is based on the acetylation of the platelet’s cyclooxygenase (COX) [20], inhibiting the thromboxane A2 pathway. The interaction between ADP and the platelet P2Y12 receptor is another essential part of the platelet’s activation process, causing enhanced platelet degranulation and thromboxane production, and prolonged platelet aggregation [21]. The inhibition of the P2Y12 pathway prevents the binding of ADP to the receptor, attenuating platelet aggregation. In patients with acute coronary syndrome (ACS) or undergoing PCI for chronic coronary syndrome (CCS), DAPT has been shown to reduce recurrent major adverse cardiovascular events (MACE) compared to aspirin alone [22,23].
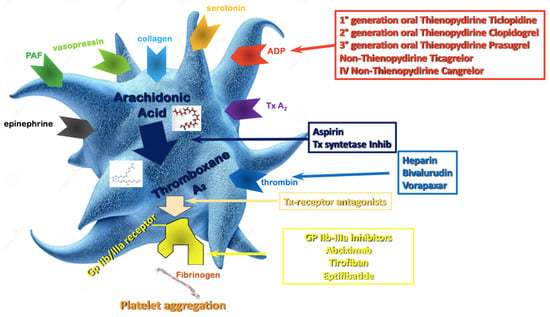
Figure 1. Antiplatelet therapy treatment pathways. ADP—Adenosine Diphosphate; Tx—Thromboxane; PAF—Platelet Activating Factor; Gp—Glycoprotein.
However, the anti-thrombotic benefits of DAPT are counterbalanced by an increase in bleeding, which is directly related to the duration and intensity of the antiplatelet regimen, and significantly impact mortality with similar time-dependency of myocardial infarction [24]. Hence, determining the optimal duration and selection of antiplatelet agents for DAPT is of the utmost importance to optimize clinical outcomes and remains a subject of ongoing investigation and clinical debate [25,26]. Recent studies have challenged the traditional notion of a one-size-fits-all approach, suggesting that individualized treatment strategies based on patient-specific factors and procedural characteristics may be necessary to select treatment [27]. Nowadays, the number of options to personalize DAPT treatment is vast, and those options are increasingly endorsed by international guidelines, leveraging on the modulation of DAPT duration (i.e., short vs. long treatment courses) [28], DAPT components in term of P2Y12 inhibitor type (i.e., potent vs. non-potent P2Y12 inhibitor), and dosage [29].
2. Optimal DAPT Duration
2.1. Twelve Months DAPT
In the last ten years, there has been a great number of studies exploring optimal duration of DAPT followed by a single antiplatelet agent. Initially the recommended duration for DAPT after coronary stenting was 1–6 months [36]. This treatment window was non-randomly tested in the studies that compared drug-eluting stents (DES) with bare metal stents (BMS). The mean follow-up time for clopidogrel-based DAPT in the PCI CURE trial was 8 months [16]. The evidence of an increased risk of late and very late ST after first-generation DES led to a more cautious approach with extension of DAPT well beyond 12 months after implantation [37,38,39,40]. Based on the available evidence, consensus-based guidelines recommended a minimum of 12 months of DAPT in this setting [41]. However, the introduction of safer stent platforms [42,43] progressively showed that DAPT duration could be safely shortened [44].
The main reason to strike an optimal duration of DAPT is to reasonably balance the risk of ischemic and bleeding events, both impacting prognosis, and both opposingly affected by the duration of antithrombotic therapy. In this context, trials comparing three or six months of DAPT to one-year DAPT found no difference in ischemic events and showed that a short-term DAPT was safer in terms of bleeding [45].
For patients presenting with CCS, 2019 ESC guidelines for the management of chronic coronary syndromes recommend a 6-month DAPT (ASA and clopidogrel) regimen after PCI (Class I, level A). Prasugrel or ticagrelor may be considered in high-risk situations, such as suboptimal stent deployment or complex PCI [46].
In patients with ACS, 2023 ESC guidelines for the management of ACS recommend a default strategy of 12 months of DAPT with a potent P2Y12 inhibitor (Class I); however, if the patient undergoes PCI, prasugrel should be considered as the P2Y12 inhibitor of choice, considering the results of the ISAR-REACT 5 RCT. Clopidgrel should only be used when ticagrelor and prasugrel are contraindicated, not available or in HBR patients [34].
2.2. Prolonged (>12 Months) DAPT
Compared to bare-metal stents, DESs reduced the rate of restenosis; however, there was an initial concern that first-generation DESs may be associated with an additional risk of late and very-late ST [47]. In addition, beyond stent-related events, ischemic events unrelated to the treated plaque may also occur, which supports the potential for prolonged antiplatelet therapy as a secondary prevention strategy [48,49].
Patients with MI have heightened platelet activation and aggregation compared with patients with CCS, leading to a higher predisposition to atherothrombosis [50,51,52], which may persist for years afterwards [53,54,55]. Hence, these patients may benefit from more intensive antiplatelet therapies following PCI.
The DAPT study was a multicenter randomized trial that enrolled patients treated with DAPT after PCI with DES. At 12 months, patients who had no MACCE, another revascularization, bleedings (moderate to severe) and had been adherent to the therapy were randomized to continue it or to placebo for another 18 months, to compare the 12 month-strategy to the 30-month strategy. The efficacy end points (cumulative incidence of definite or probable ST and the composite of death, MI, or stroke) were significantly lower in the group that continued thienopyridine (0.4% vs. 1.4% for stent thrombosis; 4.3% vs. 5.9% for MACCE) and was consistent across stent type and thienopyridine drug used. However, prolonged DAPT led to a significantly higher rate of bleeding, and all-cause mortality was increased by 36% in the prolonged DAPT group [56]. Importantly, most of the benefit observed with a prolonged DAPT treatment was observed among patients presenting with a MI [57,58].
Ticagrelor, when added to aspirin after an ACS, compared with clopidogrel, reduces the rate of major adverse CV events. Therefore, patients that suffered a MI, who are at higher risk for recurrent ischemic events, could benefit from prolonged DAPT with ticagrelor.
The Prevention of Cardiovascular Events in Patients with Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin–Thrombolysis in Myocardial Infarction 54 (PEGASUS-TIMI 54) trial, a randomized, double-blind, placebo-controlled clinical trial, tested long-term DAPT with ticagrelor, evaluating two different doses: 90 mg twice daily and 60 mg twice daily.
The patients were considered eligible if they had a spontaneous MI 1 to 3 years before, were 50 years old or older, and had one of these additional high-risk features: age of 65 years or older, diabetes mellitus (DM), a second prior spontaneous MI, multivessel coronary artery disease, or chronic renal dysfunction. They were randomly assigned in a 1:1:1 ratio to receive either ticagrelor at a dose of 90 mg twice daily (b.i.d.), ticagrelor at a dose of 60 mg b.i.d., or a placebo. The median time from the occurrence of MI, of which 53.6% were STEMI, to the point of randomization was 1.7 years. Both doses of ticagrelor reduced the incidence of cardiovascular death, MI, or stroke but led to a higher risk of bleeding, including TIMI major bleeding, bleeding requiring a transfusion, and bleeding leading to discontinuation of the study drug. Ultimately, the overall risk to benefit trade-off was improved with the ticagrelor 60 mg b.i.d. dose, which led to the final approval of this drug dose with the new indication for extended DAPT [59].
Udell et al. conducted a meta-analysis of six RCTs on secondary prevention, including 33,435 patients with prior-MI randomized to extended DAPT beyond 1 year or standard DAPT for 12 months. A DAPT regimen longer than 12 months led to a 22% reduction in the relative risk and a 1.1% reduction in the absolute risk of MACE during an average follow-up period of 31 months. There was a slight 0.8% absolute increase in the risk of major bleeding, but this did not result in a significant excess of ICH or fatal bleeding, and there were no significant differences in non-cardiovascular deaths. Importantly, extended DAPT was associated with a significant reduction in CV mortality [60]. Taking this into consideration, extended DAPT appears to be an attractive approach in patients with prior MI and a low risk for bleeding. Whether the type of P2Y12i may be associated with a different impact on the overall long-term outcomes is not well established [61].
According to current ESC guidelines, a prolonged DAPT duration should be considered in patients with high ischemic risk and without HBR (Class IIa) and may be considered in patients with moderate ischemic risk without HBR (Class IIb) [34].
2.3. Short (1 or 3 or 6-Months) DAPT
A short DAPT strategy of less than 12 months after implanting a coronary stent has been compared to one-year DAPT in several RCTs, generally testing non-inferiority for ischemic events and superiority for bleeding.
The EXCELLENT trial (A Comparison of Xience/Promus Versus Cypher in Reducing Late Loss After Stenting) aimed to assess the effectiveness of a short-term DAPT strategy (6 months). A total of 1443 patients were randomized according to DAPT duration (6 vs. 12 months) and the type of stent (everolimus-eluting stent vs. sirolimus-eluting stent). One of the points of the study was to determine if the short-term DAPT strategy was not inferior to the standard care concerning the occurrence of cardiac death, MI, or ischemia-driven target vessel revascularization (TVR).
The primary endpoint of the study was in-stent late loss at 9 months as the primary endpoint when comparing stent types, while the co-primary endpoint was the occurrence of target vessel failure (TVF) at 12 months, in relation to the duration of DAPT. The findings revealed that the six-month DAPT strategy was as effective as the standard care. Furthermore, while there was a numerical rise in TIMI minor and major bleeding events in the one-year DAPT group, this difference did not reach statistical significance (HR 0.40; 95% CI: 0.13–1.27; p = 0.12) [62].
The PRODIGY (PROlonging Dual antIplatelet treatment after Grading stent-induced intimal hYperplasia study) trial was a 4:2 randomized open-label clinical trial that evaluated the efficacy and the safety of prolonged DAPT with clopidogrel as P2Y12 inhibitor, randomly allocating patients (predominantly presenting with ACS) to four coronary stents (BMS, paclitaxel-eluting stent, E-ZES, everolimus-eluting stent) and two DAPT duration regimens (6 vs. 24 months of DAPT). The study showed no differences in the primary efficacy endpoint (death, MI, and stroke between 6 and 24 months of DAPT), and, as expected, among the patients receiving 24-month DAPT, there was a risk of type 2, 3 or bleeding events two-fold greater than in the group receiving 6-month DAPT (HR 2.17, 95% CI 1.44–3.22; p = 0.00018) [63]. Results remained largely consistent in multiple subgroups [64,65,66].
The REDUCE trial randomized 1496 ACS patients treated with COMBO stent to 3 or 12 months of DAPT. The composite primary study endpoint of all-cause mortality, MI, ST, stroke, target vessel revascularization and bleeding at 12 months was similar in the two groups, reaching prespecified non-inferiority (8.2% vs. 8.4%, p-value non-inferiority < 0.001). However, numerically higher rates of mortality and ST in the three-month DAPT group were observed [67]. The non-inferiority of 3 vs. 12 months DAPT was confirmed in several high-risk subgroups [68,69,70].
After 3–6 months of DAPT, in patients who are event-free and who are not at high ischemic risk, SAPT with a P2Y12 inhibitor or aspirin should be considered according to the current ESC guidelines (Class IIa) [34].
2.4. Individualization of DAPT Duration Based on Ischemic and Bleeding Risk
The optimal DAPT strategy, that maximizes the efficacy and the safety of the treatment, balancing ischemic and bleeding risk, should be individual and selected based on patient and procedural characteristics (Figure 2) [71,72,73].
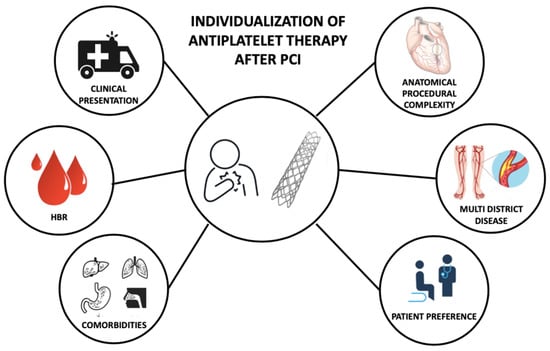
Figure 2. Features informing individualization of antiplatelet therapy after percutaneous coronary intervention. PCI—Percutaneous Coronary Intervention; HBR—High Bleeding Risk.
The clinical presentation (ACS vs. CCS) at the time of PCI is an important feature that influences the patient’s mortality risk (ranging between 0.36% in CCS and 4.78% in high-risk STEMI patients), and the risk of recurrent ischemic events [74,75]. Clinical presentation in the setting of an all-comer PCI population is also a treatment modifier of DAPT duration after coronary stenting. Costa et al. conducted an analysis of the PRODIGY trial, a study designed to compare 6- or 24-month DAPT regimens in patients treated with PCI with first- and second-generation DES with varying anti-intimal hyperplasia potency. It showed the lack of ischemic benefit in favor of a 2-year course of DAPT, in both CCS and ACS patients. In both CCS and ACS patients, the rate of bleeding was higher in the 24-month DAPT arm, with a greater magnitude in patients presenting with CCS. In terms of NACE rates, after excluding BARC 2 bleeding, there was a numerical increase in NACE in CCS patients only, with consistent borderline results in the 24-month DAPT arm, provided by the interaction testing. So, this analysis showed that clinical presentation plays a pivotal role in the treatment decision with respect to the value of DAPT duration (prolonged vs. shortened) [66].
In the DAPT trial, a randomized double-blind, placebo-controlled trial comparing 30 versus 12 months of DAPT after stent implantation, 30-month DAPT compared with one-year treatment reduced definite or probable ST in patients with MI (0.5 vs. 1.9%; p = 0.001) and without MI (0.4 vs. 1.1%; p = 0.001) (Pint = 0.69). The reduction in MACCE was greater for patients with MI (3.9 vs. 6.8%; p = 0.001) than patients without MI (4.4 vs. 5.3%; p = 0.08) at the time of presentation. Of 11,648 randomized patients (9961 treated with drug-eluting, 1687 with bare metal stents), 3576 (30.7%) presented with MI. Among patients presenting without MI, a longer DAPT regimen was also associated with a significant increase in all-cause death (2.1 vs. 1.5%; p = 0.04) [56].
The risk of ischemic events following PCI is also influenced by anatomical and procedural factors. These factors have consistently been recognized as crucial considerations when determining the duration of DAPT [76,77]. The complexity of a PCI can be quantified using previously validated and guideline-endorsed criteria: PCI with ≥3 stents implanted and 3 ≥ lesions and/or coronary vessels treated; and/or bifurcation with 2 stents implanted, total stent length > 60 mm, and/or treatment of a chronic total occlusion (CTO). In these patients, long-term DAPT (≥12 months) compared with a short period of DAPT (3 or 6 months), significantly reduced the risk of cardiac ischemic events [78].
Even the localization of the coronary artery stenosis should be considered a treatment modifier for DAPT duration, as suggested by Costa et al. in a retrospective analysis of the PRODIGY trial. In patients with a stenosis of at least 30% on angiography, appraised by visual estimation, of the left main or the proximal LAD, a 24-month DAPT regimen, compared to a 6-month DAPT regimen, significantly reduced the rate of definite, probable, or possible ST. A consistent interaction between CAD location and DAPT duration was also registered for the composite of CV death and MI. The 2-year DAPT regimen remained associated with possible benefits in patients with LM/pLAD lumen narrowing irrespective of stent implantation in these segments or patients’ clinical presentation [79].
In a patient-level meta-analysis comprising data from six RCTs (with a total of 9577 patients) that examined the optimal duration of DAPT following coronary stenting (comparing 12 months to 6 months), 17.5% of the patients exhibited characteristics associated with complex PCI. These characteristics included three-vessel PCI, implantation of three or more coronary stents, treatment of three or more coronary lesions, bifurcation stenting (using stents in both the main and side branches), a final total stent length exceeding 60 mm, and treatment of a chronic total occlusion (CTO). In this group, long DAPT compared with short DAPT reduced the adjusted MACCE rate (unadjusted event rates: 4.0 vs. 6.0%; adjusted HR 0.56, 95% CI 0.35–0.89), whereas, in the non-complex PCI group, no benefit for a longer treatment was observed (2.5 vs. 2.6%; adjusted HR 1.01; 95% CI 0.75–1.35) (Pint = 0.01). The magnitude of benefit in favor of long DAPT was directly related to the complexity of the procedure [80].
Concomitant high bleeding risk can mitigate the benefit from a longer DAPT regimen in patients undergoing a complex PCI. In an analysis that included 14,963 patients from eight randomized trials, long-term DAPT in non-HBR patients reduced the ischemic events in both complex and noncomplex PCI, but not among HBR (PRECISE-DAPT > 25) patients, regardless of complex PCI features [81].
Age is a relevant clinical factor to appraise in the choice of DAPT regimen. Although older patients (75 years old or older), have an increased thrombotic risk [82], age also represent a minor bleeding risk factor; indeed, it is included as one of the minor HBR criteria, due likely owing to concomitant renal impairment or anemia [83]. Common general strategies to reduce the rate of bleeding in this group of patients are use of proton pump inhibitors, use of radial arterial access for coronary angiography and PCI and a modulation of DAPT composition and duration [83]. According to current ESC guidelines, clopidogrel is the preferable P2Y12 inhibitor, due to a better safety profile. However, in elderly patients with a high thrombotic risk, the DAPT regimen has to be tailored, taking into account that, in the first months after the index event, the thrombotic risk is higher; therefore, a de-escalation strategy seems reasonable [84].
Gender-related differences have not been shown to affect the efficacy and safety of DAPT type or duration. No heterogeneous findings across genders have been found in pooled analysis or trials assessing a 12-year DAPT or longer vs. a shorter one [85]. A borderline quantitative interaction between reduction in ST and prolonged DAPT suggesting a relative treatment benefit in female patients compared to male patients has been shown in the DAPT trial; however, no differences were shown for MACCE or bleeding [56].
Current ESC guidelines recommend a similar type and duration of DAPT in male and female patients (Class I) [85].
Diabetes mellitus (DM) represents a risk modifier in patients presenting with both CCS and ACS, increasing the risk of fatal and non-fatal ischemic events. In terms of P2Y12 inhibitor type, there is no evidence that DM should affect the decision; indeed, no difference in benefits was shown in the CURE, the TRITON-TIMI 38 or the PLATO trial in patients with DM as compared to those without DM [16,31,32]. The DAPT study showed a lower risk reduction for MI in patients with DM but no differences for all other ischemic and safety endpoints [86]. The PEGASUS trial showed no difference for primary efficacy endpoint with respect to the presence or absence of DM [87]. Therefore, even in terms of DAPT duration, DM should not be the only patient feature to be taken into consideration, and similar DAPT type and duration should be considered in both patients with and without DM (Class IIa) [85].
Patients with peripheral artery disease are at high ischemic risk. In the CHARISMA trial, in 3096 patients, DAPT (clopidogrel plus aspirin), compared to aspirin alone, reduced the rate of MI, with no differences in terms of moderate, severe, or fatal bleeding. However, there was an increase in minor bleeding [88]. In a subgroup analysis of the PEGASUS study, the investigators found that patients with PAD and prior MI had a 60% higher risk of MACE compared to patients without PAD. In this group of patients, ticagrelor 60 mg b.i.d., compared to placebo, granted an absolute risk reduction in ischemic events of 5.2% at 3 years [89]. In the PRODIGY trial, PAD was associated with a higher risk of death and ischemic events, and prolonged DAPT, compared to short DAPT, reduced the primary efficacy endpoint in patients with PAD [90]. The ESC guidelines, considering this evidence, suggest that a prolonged DAPT (>12 months) may be considered in patients with PAD (Class IIb) [85].
This entry is adapted from the peer-reviewed paper 10.3390/jcm12227144
This entry is offline, you can click here to edit this entry!
