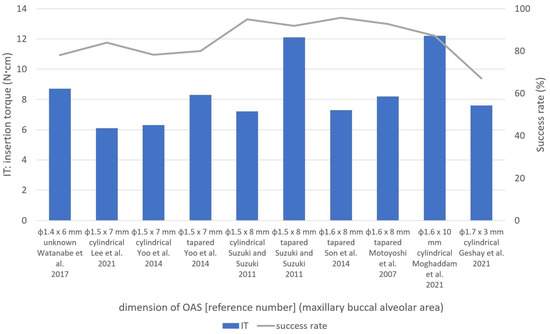
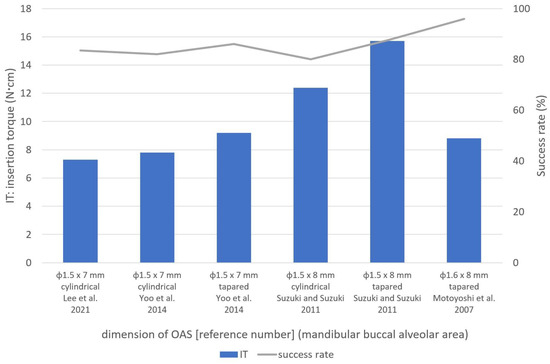
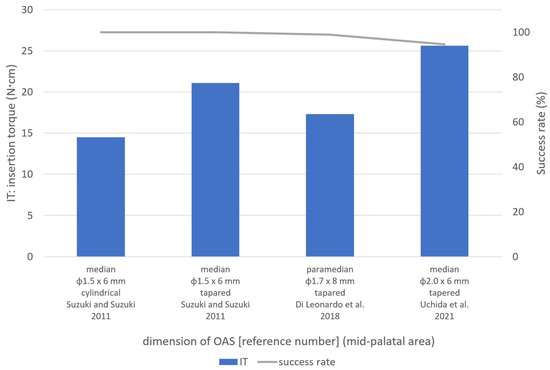
Eleven original articles with orthodontic anchoring screws (OASs) placement in humans including insertion torque (IT) and success rate were selected and were used to evaluate the relationships among IT, success rates, screw design, and placement methods at different sites. The ITs and success rates ranged from 6.0 ± 3.2 to 15.7 ± 2.3 Ncm and from 62.5 to 100.0% in the upper and lower buccal alveolar areas, respectively. For the mid-palatal area, the range was 14.5 ± 1.6 to 25.6 ± 5.5 Ncm and 83.0 to 100.0%, respectively. ITs of 5–12 and 6–14 Ncm were found to be optimal for the commonly used φ1.5–1.7 mm OASs in the upper and lower interproximal areas, respectively. In the mid-palatal suture area, ITs of 11–16 and 20–25 Ncm were considered suitable for tapered φ1.5 mm and φ2.0 mm OASs, respectively. Although identified optimal IT ranges deserve the recommendations, care must be taken to monitor the IT during placement constantly.
- orthodontic anchoring screw
- orthodontic mini-implant
- temporary anchorage device (TAD)
- placement torque
- insertion torque
- success rate
1. Introduction
2. Maternal Trait Mindfulness and Social Competence of Preschoolers
2.1. Placement Methods (Self-Drilling or Self-Tapping)
2.2. Shapes and Dimensions of OASs
2.2.1. Tapered and Cylindrical OASs
2.2.2. OAS Dimensions
An in vitro study by Chen et al. [18] examined the mechanical properties of φ1.3 × 7 mm OASs (self-drilling) using artificial bone with densities of 20, 30, and 40 pcf, and reported ITs of 3.9, 5.2, and 10.0 Ncm, respectively.
Large φ2.0 × 6 mm OASs used in one study in the mid-palatal suture area had a success rate of 94.5% and the highest ITs (25.6 ± 5.5 Ncm) [8]. An in vitro study by Nienkemper et al. [19] evaluated φ2.0 × 9 mm OASs using pig pelvic bone and reported that the ITs for insertion depths of 4 mm, 5 mm, and 6 mm were 15.4 ± 7.0 Ncm, 26.2 ± 10.4 Ncm, and 27.2 ± 14.1 Ncm, respectively. Considering these results [19], the high ITs of φ2.0 × 6 mm OASs [8] may be appropriate for regions with high-density bone, such as the mid-palatal suture area.
2.3. Placement Location
2.3.1. Buccal Alveolar Area
2.3.2. Mid-Palatal Area
OAS placement in the mid-palatal area is used for various purposes, such as the retraction of anterior teeth and intrusion, distalization, and protraction of molars in the maxillary arch [20]. OAS placement in this area is also considered anatomically more favorable than the interproximal area [21]. However, as reported by Naya-Imai et al. [22], the sutured depth of mid-palatal suture should be considered using adequate imaging, such as cone-beam computed tomography, before OAS placement because there could be incomplete suture closure even in adults. Concerning this matter, they concluded that the OAS placement in mid-palatal sutures should be avoided regardless of age to prevent the insertion into unsutured areas.
The mid-palatal area has a thicker cortex, especially close to the median suture, which often requires pre-drilling before OAS placement for IT control [8][15]. Suzuki and Suzuki [15] used both cylindrical and tapered OASs (φ1.5 mm) in this area and reported lower ITs for the former. Cylindrical OASs had ITs and success rates of 14.5 ± 1.6 Ncm and 100.0%, respectively.
In an in vitro study, Wilmes et al. [23] reported that the maximum torques at the time of fracture for φ1.5 mm and φ2.0 mm OASs were 20.1 ± 3.8 Ncm and 49.2 ± 7.5 Ncm, respectively. In an in vitro study by Dalla Rosa et al. [24], the yield torque to fracture for φ1.5 mm OASs was 16.3 ± 1.6 Ncm. Based on these studies, the ITs of 21.1 ± 2.2 Ncm for φ1.5 mm OASs reported by Suzuki and Suzuki [15] exceeded the yield torque. Therefore, the use of φ2.0 mm tapered OASs with ITs of 20–25 Ncm is thought to be suitable in the mid-palatal suture area.
2.3.3. Infrazygomatic Crest and the Buccal Shelf Areas
The infrazygomatic crest and the buccal shelf area have some clinical advantages over alveolar interproximal areas [25][26], but few studies have investigated OASs in these sites. Sreenivasagan et al. [3] investigated the ITs of OASs (φ2.0 × 12 mm) in these areas and found that the ITs and success rates at the infrazygomatic crest (12 screws) and buccal shelf (four screws) areas were 10.1 Ncm and 83.3%, and 10.3 Ncm and 100.0%, respectively. Approximately 10 Ncm IT is considered optimal in these areas, but further studies are required to investigate these placement sites.
3. Conclusions
This entry is adapted from the peer-reviewed paper 10.3390/app131910681
References
- Watanabe, T.; Miyazawa, K.; Fujiwara, T.; Kawaguchi, M.; Tabuchi, M.; Goto, S. Insertion torque and Periotest values are important factors predicting outcome after orthodontic miniscrew placement. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 483–488.
- Tepedino, M.; Masedu, F.; Chimenti, C. Comparative evaluation of insertion torque and mechanical stability for self-tapping and self-drilling orthodontic miniscrews—An in vitro study. Head Face Med. 2017, 13, 10.
- Nguyen, M.V.; Codrington, J.; Fletcher, L.; Dreyer, C.W.; Sampson, W.J. The influence of miniscrew insertion torque. Eur. J. Orthod. 2018, 40, 37–44.
- Marquezan, M.; Mattos, C.T.; Sant’Anna, E.F.; de Souza, M.M.; Maia, L.C. Does cortical thickness influence the primary stability of miniscrews?: A systematic review and meta-analysis. Angle Orthod. 2014, 84, 1093–1103.
- Casaña-Ruiz, M.D.; Bellot-Arcís, C.; Paredes-Gallardo, V.; García-Sanz, V.; Almerich-Silla, J.M.; Montiel-Company, J.M. Risk factors for orthodontic mini-implants in skeletal anchorage biological stability: A systematic literature review and meta-analysis. Sci. Rep. 2020, 10, 5848.
- Geshay, D.; Campbell, P.; Tadlock, L.; Schneiderman, E.; Kyung, H.M.; Buschang, P. Stability of immediately loaded 3 mm long miniscrew implants: A feasibility study. Dent. Press J. Orthod. 2021, 26, e2119155.
- Motoyoshi, M.; Matsuoka, M.; Shimizu, N. Application of orthodontic mini-implants in adolescents. Int. J. Oral Maxillofac. Surg. 2007, 36, 695–699.
- Uchida, Y.; Namura, Y.; Inaba, M.; Osada, A.; Charleston-Coad, T.; Nakamura, Y.; Motoyoshi, M. Influence of pre-drilling diameter on the stability of orthodontic anchoring screws in the mid-palatal area. J. Oral Sci. 2021, 63, 270–274.
- Lee, Y.; Choi, S.H.; Yu, H.S.; Erenebat, T.; Liu, J.; Cha, J.Y. Stability and success rate of dual-thread miniscrews. Angle Orthod. 2021, 91, 509–514.
- Sreenivasagan, S.; Subramanian, A.K.; Nivethigaa, B. Assessment of insertion torque of mini-implant and its correlation with primary stability and pain levels in orthodontic patients. J. Contemp. Dent. Pract. 2021, 22, 84–88.
- Moghaddam, S.F.; Mohammadi, A.; Behroozian, A. The effect of sandblasting and acid etching on survival rate of orthodontic miniscrews: A split-mouth randomized controlled trial. Prog. Orthod. 2021, 22, 2.
- Di Leonardo, B.; Ludwig, B.; Lisson, J.A.; Contardo, L.; Mura, R.; Hourfar, J. Insertion torque values and success rates for paramedian insertion of orthodontic mini-implants: A retrospective study. J. Orofac. Orthop. 2018, 79, 109–115.
- Yoo, S.H.; Park, Y.C.; Hwang, C.J.; Kim, J.Y.; Choi, E.H.; Cha, J.Y. A comparison of tapered and cylindrical miniscrew stability. Eur. J. Orthod. 2014, 36, 557–562.
- Son, S.; Motoyoshi, M.; Uchida, Y.; Shimizu, N. Comparative study of the primary stability of self-drilling and self-tapping orthodontic miniscrews. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 480–485.
- Suzuki, E.Y.; Suzuki, B. Placement and removal torque values of orthodontic miniscrew implants. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 669–678.
- Assad-Loss, T.F.; Kitahara-Céia, F.M.F.; Silveira, G.S.; Elias, C.N.; Mucha, J.N. Fracture strength of orthodontic mini-implants. Dent. Press J. Orthod. 2017, 22, 47–54.
- Da Cunha, A.C.; Marquezan, M.; Lima, I.; Lopes, R.T.; Nojima, L.I.; Sant’Anna, E.F. Influence of bone architecture on the primary stability of different mini-implant designs. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 45–51.
- Chen, Y.; Kyung, H.M.; Gao, L.; Yu, W.J.; Bae, E.J.; Kim, S.M. Mechanical properties of self-drilling orthodontic micro-implants with different diameters. Angle Orthod. 2010, 80, 821–827.
- Nienkemper, M.; Santel, N.; Hönscheid, R.; Drescher, D. Orthodontic mini-implant stability at different insertion depths: Sensitivity of three stability measurement methods. J. Orofac. Orthop. 2016, 77, 296–303.
- Kim, Y.H.; Yang, S.M.; Kim, S.; Lee, J.Y.; Kim, K.E.; Gianelly, A.A.; Kyung, S.H. Midpalatal miniscrews for orthodontic anchorage: Factors affecting clinical success. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 66–72.
- Stockmann, P.; Schlegel, K.A.; Srour, S.; Neukam, F.W.; Fenner, M.; Felszeghy, E. Which region of the median palate is a suitable location of temporary orthodontic anchorage devices? A histomorphometric study on human cadavers aged 15–20 years. Clin. Oral Implant. Res. 2009, 20, 306–312.
- Naya-Imai, H.; Uchida, Y.; Inaba, M.; Namura, Y.; Osada, A.; Charleston-Coad, T.; Nakamura, Y.; Motoyoshi, M. Age dependence of the maturation of the midpalatal suture in the stability of orthodontic anchoring screws. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 809–819.
- Wilmes, B.; Panayotidis, A.; Drescher, D. Fracture resistance of orthodontic mini-implants: A biomechanical in vitro study. Eur. J. Orthod. 2011, 33, 396–401.
- Dalla Rosa, F.; Burmann, P.F.; Ruschel, H.C.; Vargas, I.A.; Kramer, P.F. Evaluation of fracture torque resistance of orthodontic mini-implants. Acta Odontol. Latinoam. 2016, 29, 248–254.
- Chen, C.M.; Wu, J.H.; Lu, P.C.; Wang, H.C.; Lee, H.E.; Wang, C.H.; Du, J.K. Horizontal pull-out strength of orthodontic infrazygomatic mini-implant: An in vitro study. Implant Dent. 2011, 20, 139–145.
- Nucera, R.; Lo Giudice, A.; Bellocchio, A.M.; Spinuzza, P.; Caprioglio, A.; Perillo, L.; Matarese, G.; Cordasco, G. Bone and cortical bone thickness of mandibular buccal shelf for mini-screw insertion in adults. Angle Orthod. 2017, 87, 745–751.
