Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Orthopedics
Thoracic outlet syndrome (TOS) is a group of symptoms that result from compression of the neurovascular bundle that exits the thoracic outlet. The thoracic outlet is defined as an anatomical area in the lower neck, extended from the supraclavicular fossa to the axilla, and consists of three main spaces, the interscalene triangle, the costoclavicular, and the subcoracoid space. These confined spaces go through relevant structures, which include the subclavian and axillary arteries, their venous counterparts, and the brachial plexus (BP).
- thoracic outlet syndrome
- risk factors
- congenital
- acquired
- trauma related
1. Pathophysiology—Trauma of the Shoulder or Neck
Thoracic outlet syndrome typically develops as nerve entrapment syndrome under pathophysiological mechanisms, including a combination of anatomical predisposition and extraneous factors. Extraneous factors leading to decompensation include acquired factors (mentioned above) and neck trauma, as well as shoulder trauma [114]. This type of injury can lead to TOS development in several different ways—Figure 5.
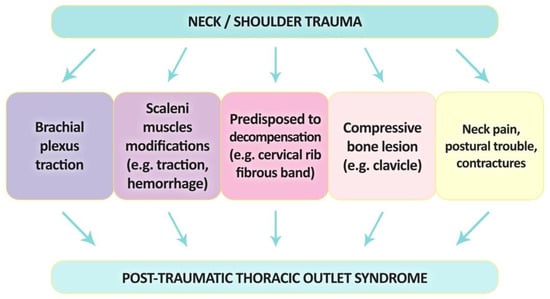
Figure 5. A diagram showing potential pathomechanisms causing trauma-related thoracic outlet syndrome.
Firstly, BP traction injuries are most often after the extension or acute flection of the neck [115]. This mechanism is responsible for the largest number of nTOS cases. BP can undergo soft, straight traction that causes signs that are immediately noticed by the patient (secondary to whiplash injury) [115,116]. Ide et al. described a series of 119 patients with whiplash injuries caused by traffic accidents. The 45 of 119 (37.8%) injured had nTOS caused by irritation of the BP [116]. Interestingly, more women, compared to men, had a higher BP irritation rate. The left side was injured more frequently than the right. According to this research, driving position is associated with a lower risk of symptoms than among passengers, and fastened seat belts reduce the risk of symptoms [116].
Second, BP entrapment may also be caused by fibrotic scar tissue, which is formed in this region as a result of AS and MS traction, microhemorrhages, and injuries to contiguous structures [117]. Several research studies agree that the direct cause of symptoms in this pathophysiological mechanism is the narrowing of the interscalene triangle as a consequence of the modification of the structure of AS and MS after trauma [114,118,119,120]. This is the most described cause of TR-TOS in the literature. Sanders et al. described the changes that occur in the structure of AS and MS after injury occurring in patients with TOS [117]. They also noted a definite predominance of type 1 fibers over type 2 in muscle structures after injury. In comparison, this muscle has an approximate amount of both types of fibers. Additionally, post-traumatic muscles had a significantly increased connective tissue content. These observations were consistent with a history of neck injury [117].
The thoracic outlet can be narrowed by various structures such as CR, prolonged TP, additional scalene muscles, scars, or inborn ligament or bands. The predisposed thoracic outlet can be decompressed by the sudden force received at this location at the time of injury. Decompression can occur quickly and most often lead to a neurogenic type of TOS, which several authors in the literature [21,117,121,122].
TOS can occur after fractures of the FR, the transverse process of C7, or the clavicle; eight patients with developed TOS in this pathomechanism were described by Dubuisson et al. [122]. In 1973, Mulder described a few patients who had various forms of TOS after trauma to the collarbone, cervical spine, shoulder, or FR [123]. Casbas et al. reported 13 cases of TOS with procured bone lesions, and in their work, they pointed out that these types of cases may account for approximately 5% of all patients with TOS [124]. In this mechanism, damage to BP can first be explained by edema, bleeding, or compression by bone fragments (due to the fact that free bone block may cause a reduction in the space in the costoclavicular area).
Several authors have hypothesized that spasms or pain of the neck/shoulder muscle (which are often seen after whiplash injuries), as well as poor shoulder posture, can contribute to the development of TR-TOS. It is worth noting that not all individuals who experience a car accident develop TR-TOS, and its occurrence may be influenced by factors such as anatomical conformation, work habits, and pretraumatic posture. The prolonged anticontraction following whiplash injury can result in connective tissue changes and the formation of micro adhesions, which may lead to the development of TR-TOS.
2. Incidence of TR-TOS
Trauma-related thoracic outlet syndrome accounts for a very large proportion of the causes of this condition. Ellison et al. wrote about the frequency reaching 49% (single trauma leading to TOS) [114,122]. Among TR-TOS, the most common reason for its occurrence was traffic accidents. In the study described by Dubuisson et al., this reason represented 63% of cases [122]. The force hyperextends the neck and stretches the cranial muscles (most often the scaleni muscles). Muscles stretch, bleed, hypertrophy, and shorten. In the process, the already crowded triangular tunnel through which the neurovascular bundles pass becomes even narrower [122].
In 1978, Woods reported that TOS occurred in 459 of 1958 patients with cervical soft tissue trauma, representing a rate of up to 23% [125]. In a recent article by Ide et al., 45 of 119 patients (37.8%) injured in car accidents were diagnosed with BP irritation [116]. In turn, Ellison et al. reported that TR-TOS among their patients was the most common result of a motorcycle accident (47.78%), followed by falls (20.45%), with traction injury (11.36%) being the third most common reason [114]. These statistics show that TR-TOS is a large percentage of TOS cases. Injuries of this type are not only a direct trigger of TOS but are also a serious risk factor for future symptoms as a long-term complication. The incidence of whiplash injury has increased over the years and is becoming, along with accidents, one of the most common causes of TR-TOS. Acceleration-extension lesions of the cervical spine also account for a large percentage of TR-TOS triggers [122].
3. TOS Secondary to Inflammations
Weinberg et al. described TOS as a result of arthritis of the first costovertebral joint. In this article, 40 of 232 patients studied (who were tested for TOS) over 6 years of medical practice were found to have this kind of arthritis as a cause [126]. The authors believe that the mechanism that causes this syndrome is that when hydrocortisone is injected into the costovertebral joint, the first intercostal nerve is entrapped as it crosses the narrow space between the first and second costovertebral joints [126].
Another example of inflammation leading to TOS is neuritis of BP. However, in this case, the pathomechanism is completely different from that in the previous paragraph. The research identified neuritis as the cause of TOS atrophy of the shoulder girdle, leading to biomechanical dysfunction. Muscle weakness leading to an abnormal head or shoulder position has already been described in this study, but the main cause is precisely BP neuritis. The most common nerves in neuritis are the long thoracic, suprascapular, and interosseus nerves [127]. The etiology is often unknown but may occur after surgery or illness [128].
This entry is adapted from the peer-reviewed paper 10.3390/jcm12216811
This entry is offline, you can click here to edit this entry!
