Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Others
Chronic hepatitis B caused by persistent infection with the hepatitis B virus (HBV) is a major public health threat in endemic regions like the World Health Organization (WHO) Africa region. Chronic infection with HBV poses a 15–25% lifetime risk of acquiring liver cirrhosis or hepatocellular carcinoma. This is inversely proportionate to the age of acquisition and in the absence of interventions, ~90% of babies born to mothers testing positive for the hepatitis B surface (HBsAg) or e (HBeAg) antigens will develop chronic infection, raising significant global public health concern.
- Africa
- birth-dose
- hepatitis B
- health systems
- vaccine
1. Current Knowledge on the Risk of HBV MTCT in the WHO Africa Region
Areas of high endemicity are defined as having an HBsAg prevalence of ≥8%, moderate endemicity between 2–7% and low endemicity of <2% in the general population [2,6]. In Africa, an estimated HBsAg prevalence of 7.5% is recorded, and Africa is considered home to approximately 28% of the world’s 296 million chronic carriers [16,17]. Prior to regional adoption of routine hepatitis B vaccination, >95% of all infections occurring in infancy were associated with horizontal transmission [3]. In recent years, a growing risk of vertical transmission (>5%) has been observed and is cited to be influenced by the HIV epidemic, as subsequently discussed in Section 3.1.2 [3,19]. Despite this, strategies employed to control the burden of hepatitis B depend almost solely on the 1992 WHO recommendation of universal hepatitis B infant vaccination commencing at 4 or 6 weeks of life [5]. In the absence of strategies targeting the interruption of vertical transmission, the cycle of chronic infection continues to fuel the morbidity and mortality [2,15]. The immaturity of the neonatal immune system increases the risk of viral replication and is suggested as the reason for delayed clearance of HBeAg [44], whereas acute infections in immunocompetent adults are likely to be cleared [15]. In a meta-analysis of 15 articles investigating HBV infection among women in sub-Saharan Africa, a total of 14,239 women were screened for HBsAg and a further 951 for HBeAg [45]. Among these studies, HBeAg positivity was shown to increase the risk of vertical transmission to 38.3% compared to 4.8% in HBeAg negative women [45]. Therefore, assessing the increased risk of HBV MTCT, the influence of HIV co-infection, and the strategies available for effective prevention of HBV MTCT in Africa is essential.
3.2. Status of HBV MTCT Mitigation Strategies in the WHO Africa Region
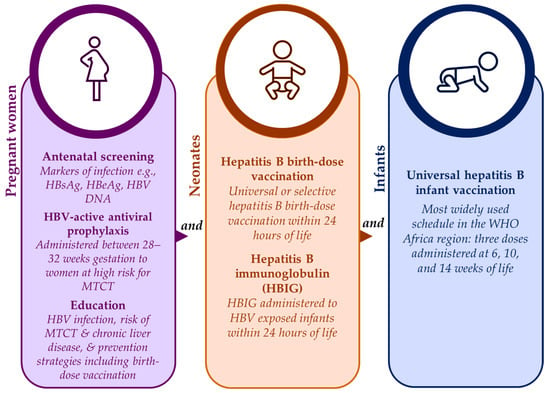
Safe and effective strategies are available for prevention of HBV MTCT to neonates and infants from as early as the in-utero stage, as shown in Figure 1. Antenatal screening has the advantage of identifying those at risk for HBV MTCT who can then be timely linked to appropriate care such as HBV-active antiviral prophylaxis [47]. During antenatal visits, pregnant women should also be provided with information on HBV infection, the lifetime risk for chronic liver disease associated with HBV MTCT, and the prevention strategies available to them and their babies including hepatitis B birth-dose vaccination [23,47]. Unfortunately, for some African countries, antenatal screening for HBV infection can be expensive and impractical if laboratory facilities are not situated close to antenatal clinics [23,47]. Despite this, the feasibility of antenatal screening for HBV infection has been proven in South Africa [15], and cost-effectiveness has been demonstrated in Namibia as part of the national HBV MTCT prevention package [3]. Maximum gains can be achieved if HBV antenatal screening is integrated with existing HIV and syphilis point-of-care testing infrastructure [15,55].
Antiviral prophylaxis offered in the third trimester to at-risk pregnant women has been proven to suppress maternal viral loads and decrease the likelihood of HBV MTCT [4,15,20]. The HBV-active antiviral prophylaxis is safe, effective, and readily available in Africa [20,47]. Despite this access for HBV mono-infected pregnant women in the region appears limited given that there are no subsidized HBV-active antiviral programs [20,47]. To the contrary, HBV–HIV co-infected pregnant women have access to lifesaving prophylaxis through established HIV treatment programs [20,47]. The fixed combination dosage of HBV-active antivirals (tenofovir, lamivudine/emtricitabine and efavirenz) prescribed for the treatment of HIV is subsidized, leaving resource-constrained settings having to pay higher prices for treatment options (such as tenofovir) for HBV mono-infection [20]. This calls for further interventions at the policy level to improve access to low-cost antiviral prophylaxis for HBV mono-infected pregnant women as part of HBV MTCT prevention strategies [47].
For neonates born to women living with chronic HBV infection, hepatitis B immunoglobulin (HBIG) offers further benefit in preventing HBV MTCT by providing passive immunization to HBV-exposed neonates, particularly when administered within 24 h of birth [3]. According to the international guidelines from key special interest groups like the American and European Associations for the Study of Liver Disease, HBV-exposed infants should receive both HBIG and a birth-dose of the hepatitis B vaccine [56,57]. In high-income countries, the standard of care includes both interventions [20,55]. In low-resource settings, the high cost and the logistics of cold-chain storage and administration of HBIG limit its acceptability as an HBV MTCT prevention strategy [3,4,15,20,47,55].
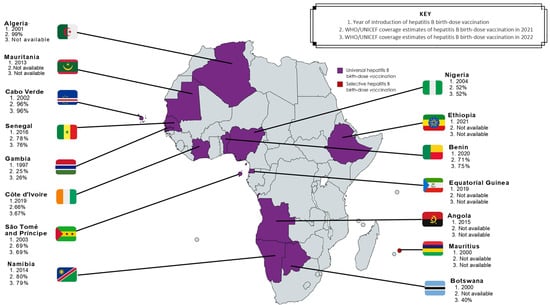
Although all strategies have proven effective [23,58], universal hepatitis B birth-dose vaccination has demonstrated suitability for the African context [23] due to both vaccine effectiveness [2,46] and high cost-effectiveness in the region [1,22]. Unlike HBIG, the hepatitis B birth-dose vaccine is stable outside of the cold chain [59], and therefore improves accessibility in low- and middle-income countries (LMICs) [60]. It also presents a feasible opportunity for integration into existing infrastructure like the Expanded Program on Immunization and prevention of HIV MTCT packages [14]. Hence, universal hepatitis B birth-dose vaccination offers an equitable solution to accelerating regional progress towards achieving global elimination of hepatitis B by 2030. Between 75–95% of vertical transmissions can be prevented by vaccinations alone if the birth-dose is followed by completion of at least 3 doses of the hepatitis B vaccine in infancy [22]. The global coverage of hepatitis B birth-dose vaccination has steadily improved from 5% in 2000 to 45% in 2022 [21], although this is well below the GHSS 2030 target of 90% [25]. Among all 6 WHO regions, the coverage rate of the hepatitis B birth-dose vaccine in Africa is significantly dismal at 18%, compared to 80% in the Western Pacific, 65% in the Americas, 58% in South-East Asian, 42% in European, and 32% in the Eastern Mediterranean regions [21]. This suboptimal coverage is independent of the number of African countries who have adopted universal hepatitis B birth-dose vaccination programs [29,30,61]. As shown in Figure 2, only 15 member states currently offer this intervention; Algeria, Angola, Botswana, Cabo Verde, The Gambia, Mauritania, Namibia, Nigeria, São Tomé and Príncipe, Senegal, Cote d’Ivoire, Benin, Equatorial Guinea, and Ethiopia all have universal hepatitis B birth-dose policies in place, whereas Mauritius currently provides selective hepatitis B birth-dose vaccination to HBV-exposed neonates [2,29,30]. It is important to note that while other African countries have not adopted a national universal hepatitis B birth-dose vaccination policy [29], they may provide targeted hepatitis B birth-dose vaccination to infants born to HBeAg-positive mothers in certain sub-regions or health facilities, as per national guidelines for prevention of MTCT or as part of project-based programs like research studies conducted in order to motivate national implementation [14,15]. In this regard, there may be an underestimation of the true coverage of the hepatitis B birth-dose vaccine in Africa compared to what is officially reported to the WHO [21,62]. Without universal and optimal screening programs to identify all at-risk pregnant women, these targeted approaches may encounter significant challenges. Nevertheless, the low implementation of universal hepatitis B birth-dose vaccination within Africa is concerning given the growing risk of HBV MTCT in this region.
Despite the lack of region-wide adoption of hepatitis B birth-dose vaccination, universal hepatitis B infant vaccination programs have been successful at reducing the incidence of horizontally transmitted HBV infection in under-5-year-olds, leading to a significant reduction in the burden of the disease worldwide [63]. The WHO Africa regional office reports that all 47 member states have introduced routine childhood hepatitis B vaccination with the majority (94%) using the pentavalent vaccine (a combination vaccine for diphtheria, tetanus, hepatitis B, pertussis, and Haemophilus influenzae type B), administered in a 3-dose schedule at 6, 10, and 14 weeks of life [2]. However, various studies have demonstrated ongoing HBV infection in children despite the receipt of all 3 doses [4,64,65,66,67], suggesting susceptibility to infection from exposure early on at birth [19]. It is therefore clear that the current strategy is insufficient at interrupting HBV MTCT, which carries a higher likelihood of life-long infection and fatal outcomes.
This entry is adapted from the peer-reviewed paper 10.3390/tropicalmed8100474
This entry is offline, you can click here to edit this entry!