Autoimmune thyroid disease (AITD) is the most common organ-specific autoimmune disorder clinically presented as Hashimoto thyroiditis (HT) and Graves’ disease (GD). The pathogenesis of AITD is caused by an inappropriate immune response related to genetic, non-genetic, and environmental factors. Pregnancy is one of the factors that have a great influence on the function of the thyroid gland because of the increased metabolic demand and the effects of hormones related to pregnancy. During pregnancy, an adaptation of the maternal immune system occurs, especially of the innate immune system engaged in maintaining adaptive immunity in the tolerant state, preventing the rejection of the fetus. Pregnancy-related hormonal changes (estrogen, progesterone, hCG) may modulate the activity of innate immune cells, potentially worsening the course of AITD during pregnancy. This especially applies to NK cells, which are associated with exacerbation of HD and GD. On the other hand, previous thyroid disorders can affect fertility and cause adverse outcomes of pregnancy, such as placental abruption, spontaneous abortion, and premature delivery. Additionally, it can cause fetal growth retardation and may contribute to impaired neuropsychological development of the fetus.
1. Introduction
Autoimmune thyroid disease (AITD) is the most common organ-specific autoimmune disorder presenting clinically as Hashimoto thyroiditis (HT) and Graves’ disease (GD). Estimates suggest that AITD affects considerably more women than men, with a prevalence of 5–15% vs. 1–5%, respectively [
1]. In addition, an increase in the incidence of AITD has been reported in recent years [
2,
3]. The underlying pathophysiology of AITD includes an aberrant immune response targeted against own body antigens in thyroid cells due to the lack of self-tolerance, in interaction with genetic, non-genetic, and environmental factors.
Genetic factors connected with AITD include polymorphism in human leukocyte antigen system (HLA) genes, cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) gene, protein tyrosine phosphatase non-receptor type 22 (PTPN22) gene, FOXP3 gene [
4], chromosome X inactivation patterns, cytokines and receptors interleukin-2 (IL-2), IL-2 receptor (IL-2R), estrogen receptors, adhesion molecules (CD14, CD40), selenoprotein S, and gene products associated with apoptosis. There are also thyroid-specific AITD susceptibility genes, such as thyroid-stimulating hormone receptor (TSHR), thyroglobulin (Tg), and thyreoperoxidase (TPO) genes, potentially connected to AITD [
4].
Non-genetic, environmental factors usually have a role in genetically predisposed patients and include cigarette smoking, alcohol, exposure to radiation and chemicals (phthalates, flame retardants), bacterial and viral infections (
Yersinia enterocolitica,
Helicobacter pylori, hepatitis C virus), but the risk has also been described with living in sterile conditions. Dietary problems connected with higher AITD prevalence are iron deficiency, decreased selenium and vitamin D intake, and a gluten-rich diet. Variable iodine exposure with higher AITD prevalence in iodine-rich and lower prevalence in iodine-deficient areas is already well known [
8,
9]. Gut microbiota with
Bacteroides fragilis overgrowth, stress, and certain drugs, such as tyrosine kinase inhibitors, amiodarone, and lithium are also considered risk factors for AITD development [
10,
11].
Clinical presentation of overt AITD is generally the reflection of the hormonal status, with some exceptions in subclinical cases. Although GD and HT are also functionally and clinically different entities, they are pathophysiologically related and may cross-develop. In the case of HT, which is characterized by an increase in thyrotropin (TSH) and lower levels of thyroid hormones, triiodothyronine (T3), and thyroxine (T4), the signs of thyroid hypofunction prevail, including weight gain, slower heart rate, slow bowel movement with constipation, enlarged thyroid gland, normocytic anemia, skin changes, hair and body hair loss, edema, fatigue, and memory impairment [
12]. On the other hand, hyperthyroidism in GD is characterized by the opposite, higher T3 and T4 hormone levels, suppressed TSH, weight loss, rapid heartbeat, and accelerated bowel movement with diarrhea, while thyroid gland enlargement, hair loss, and fatigue are also present but caused by different underlying pathophysiological mechanisms. There are also effects connected with the reproductive system, such as anovulatory cycles due to impaired estrogen precursor conversion and menorrhagia [
13]. Subclinical cases of HT are defined as elevated TSH with normal thyroid hormone levels, and although the majority is asymptomatic, there are some clinical data on increased rate of cardiovascular morbidity in those patients [
14,
15,
16].
In patients with initial HT, symptoms and signs of thyroid hyperfunction can be seen due to enhanced thyroid hormone release from damaged thyroid cells into circulation. This type of thyrotoxicosis is self-limiting and further progresses to permanent hypothyroidism. In silent and postpartum thyroiditis, thyrotoxicosis is also present but is of shorter duration, followed by hypothyroidism, which in the majority of cases recovers completely within the first year postpartum.
Apart from genetic and environmental factors, pregnancy has a great influence on the function of the thyroid gland. It has been proposed that there is an export of cells between the mother and the fetus in both directions, starting from the second week of pregnancy, including cells of immune origin, which can persist in the host for years, and is referred to as fetal and maternal cell microchimerism [
17].
For about 20 weeks, the fetus is dependent on the maternal production of thyroid hormones. After that, the fetal thyroid begins to produce its own hormones but is still dependent on the mother’s iodine supply. Thyroid volume increases by 10% to 40% depending on iodine status. Therefore, an iodine intake of 250 micrograms/day is recommended during pregnancy, and 150 micrograms/day is required for women planning pregnancy or breastfeeding [
18].
To meet the increased metabolic demand during pregnancy, there are significant changes in thyroid function, such as an increase in serum thyroid-binding globulin (TBG) and stimulation of TSHR by human chorionic gonadotropin (hCG).
Serum TBG concentrations during pregnancy rise nearly twofold because estrogen increases TBG production and TBG sialylation, which results in a decreased clearance of TBG [
18,
19].
hCG stimulates the secretion of thyroid hormones and transiently suppresses the maternal TSH, especially in the first trimester in 15% of healthy pregnant women [
18]. This is known as gestational transient thyrotoxicosis. There are changes in the reference values of maternal TSH; the lower limit decreases for 0.1–0.2 mU/L and the upper limit for 0.5–1.0 mU/L compared with the reference range of non-pregnant women [
20], which is especially pronounced in multiple pregnancies. Circulating TBG and total thyroxine (TT4) concentrations gradually increase until 16 weeks of gestation and remain high until delivery [
18].
2. The Delicate Thyroid Equilibrium in Pregnancy
Thyroid dysfunction is a pathological condition commonly seen in pregnant women, and likewise, AITD can undesirably affect fertility. Its association with adverse outcomes such as placental abruption, spontaneous abortion, and premature delivery [
21], gestational hypertension, and fetal growth retardation is confirmed by a plethora of studies [
22].
Maternal biochemical hypothyroidism is usually a priori defined as TSH above 6.0 mIU/L, and exposure to TSH above 10 mIU/L is used as a marker of overt maternal hypothyroidism. It is known that subclinical thyroid dysfunction before conception is related to an increased risk of adverse pregnancy outcomes [
26], which significantly occur in pregnant women having TSH above 10 mIU/L. Interestingly, no significant association between thyroid autoantibodies and pregnancy outcomes was found in recent research by Knøsgaard et al. [
27]. Increasing evidence emphasizes an elevated risk of adverse gestational and neonatal outcomes induced by subclinical hypothyroidism in women during the early gestational period. Particularly, the risk of pregnancy-specific complications has been increased in TPOAb-positive women having serum TSH levels exceeding 2.5 mIU/L, especially in those with serum TSH levels greater than 4.0 mIU/L [
28].
Concerns were raised about thyroid dysfunction in newborns whose mothers have (autoimmune) hypothyroidism, which led to the practice of thyroid hormone testing in the early neonatal period.
3. Autoimmune Hyperthyroidism in Pregnancy
The most common cause of hyperthyroidism in pregnancy is GD, which occurs in about 0.2% of all pregnancies in iodine-rich areas [
20,
31], whereas in iodine-deficient countries, excessive thyroid hormone production is usually caused by autonomous thyroid nodules [
32], GD often improves during the third trimester of pregnancy and may worsen during the first year after birth. It is characterized by the production of thyroid-stimulating immunoglobulin (TSI) autoantibodies that bind to the TSH receptor and stimulate the overproduction of thyroid hormones. TSI antibodies cross the placenta and cause fetal or neonatal hyperthyroidism (incidence between 1% and 5% in women with GD) [
33]. However, if the mother is taking antithyroid drugs (ATDs) for GD, fetal hyperthyroidism is rare because ATDs also cross the placenta, preventing fetal hyperthyroidism [
34]. Elevated TPOAb or TgAb were found in 2% to 17% of pregnant women [
35].
It is very difficult to distinguish GD from gestational transient thyrotoxicosis (GTT) in early pregnancy since both conditions have similar symptoms: palpitations, tremors, and heat intolerance. The likelihood of transient thyrotoxicosis during pregnancy is higher in pregnant women who have not had previous thyroid disease, goiter, or orbitopathy and have a mild vomiting disorder [
37].
Hyperthyroidism in pregnancy can also be caused by toxic multinodular goiter and toxic adenoma [
38]. Subacute painful or silent thyroiditis are very rare causes of thyrotoxicosis in pregnancy, while TSH-secreting pituitary adenoma, struma ovarii, functional thyroid cancer metastases, or a TSH receptor mutation leading to functional hypersensitivity to hCG [
39] are even rarer.
4. Autoimmune Hypothyroidism in Pregnancy
Hypothyroidism in pregnancy is commonly defined as the presence of elevated TSH and decreased serum T4 concentration during gestation, with both concentrations outside the trimester-specific reference ranges. For women with a TSH above the population and trimester-specific upper limit, or above 4.0 mIU/L when local reference ranges are not available, free T4 should be measured [
41]. The most common cause of thyroid hypofunction during pregnancy is HT.
It is estimated that 2–3% of healthy non-pregnant women of reproductive age have elevated TSH, and thyroid autoantibodies are present in around 30–60% of those cases. [
42].
Continuing pregnancies with overt hypothyroidism have been associated with an increased risk of several complications such as preeclampsia, gestational hypertension, placental abruption, preterm delivery, low birth weight, increased rate of cesarean section, postpartum hemorrhage, perinatal morbidity and mortality, and neuropsychological and cognitive impairment in the child.
De Leo reports the presence of TPOAbs and TgAbs in 5–14% and 3–18% of pregnant women, respectively [
43]. In addition to this, TPOAbs were found in 9.5% of women with previous pregnancy loss or subfertility [
44].
AITD is the most common autoimmune disease in women of reproductive age, affecting nearly 10% of that group. Keeping this in mind is of great interest to clinicians because of the potential negative impact on female fertility and pregnancy outcomes [
45].
5. The Immunological Background of AITD
The immunological background of AITD includes innate and adaptive mechanisms. In general, innate mechanisms are cell-mediated and ensure a prompt response to pathogens, whereas adaptive mechanisms are specific and involve the formation of antibodies targeted to specific antigens [
46] but also seem to be directed by innate factors. HT is primarily characterized by cell-mediated autoimmunity in the form of lymphocytic infiltration, causing the destruction of thyroid follicles. It has recently been proposed that the presence of specific stromal cells in the thyroid of patients with HT stimulates inflammatory cell recruitment, even the formation of highly organized lymphocytic infiltrates termed tertiary lymphoid organs [
47]. Tissue destruction and the consequent exposure of thyroid antigens cause autoantibody production.
Contrary to adaptive immunity that has been extensively described in AITD, the cells of innate immunity involved in the pathophysiology of AITD have recently gained more attention. The main cells involved in the innate immunological processes are polymorphonuclear leukocytes (mainly neutrophils), innate lymphoid cells including natural killer (NK) cells, natural killer T (NKT) cells, monocytes, macrophages, and dendritic cells (DCs) [
51,
52,
53,
54].
6. Innate Immunity during Normal Pregnancy
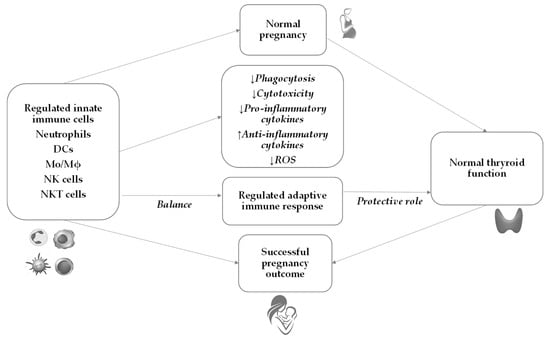
During normal pregnancy, a complex and extensive adaptation of the maternal immune system occurs to protect the mother and the fetus from infection and activation of detrimental immune response against the semi-allogeneic fetus. Throughout pregnancy, the innate immune system changes and plays a critical role in maintaining adaptive immunity in the tolerant state (
Figure 1). This tolerogenic state during pregnancy is well established systemically and especially locally where maternal and fetal tissues are in direct contact with each other. It is considered that decidua and, as lately described, placenta play pivotal roles in the innate immune response [
57].
Figure 1. Pregnancy outcome in normal pregnancy. In a normal pregnancy, a well-regulated innate immune response leads to balanced thyroid function and contributes to a successful pregnancy outcome. DCs—dendritic cells; Mo—monocytes; Mϕ—macrophages; ROS—reactive oxygen species; NK—natural killer; NKT—natural killer T cells.
Throughout pregnancy, the decidual cells secrete chemokines that attract NK cells, NKT cells, DCs, macrophages, and T-regulatory (Tregs) lymphocytes. During the initial weeks of pregnancy, about 70% of decidual lymphocytes are NK cells, 20% are macrophages, and only 2% are DCs. In contrast to decidual tissue, up to 90% of maternal peripheral blood leukocytes are comprised of neutrophils [
58,
59,
60].
This increased number of neutrophils during pregnancy, especially in the second and third trimesters, is called neutrophilia and is a physiological condition [
60]. The neutrophils are considered the first line of innate immunity responsible for the defense of the mother and the fetus due to their ability to exert a variety of mechanisms to combat tissue damage and infection such as cytotoxic activity, phagocytosis, synthesis of reactive nitrogen species (RNS), reactive oxygen species (ROS), and secretion of a variety of cytokines and chemokines [
61,
62].
Together with an increased number of neutrophils, the number of monocytes increases during pregnancy, starting in the first trimester [
64]. This upregulation of monocytes is predominantly due to a higher proportion of intermediate CD14
+CD16
+ monocytes, which are responsible for pro-inflammatory cytokine production, such as interleukin (IL)-1α, IL-6, IL-12, tumor necrosis factor-alpha (TNF-α) [
65] and decreased phagocytic activity throughout pregnancy [
66]. An increased number of monocytes is accompanied by their progressive activation [
67].
In decidua, macrophages represent the second most abundant decidual leukocytes after fertilization, attracted by decidual-derived chemokines such as monocyte chemoattractant protein-1 (MCP-1), MCP-3, macrophage inflammatory protein 1-alpha (MIP-1α), MIP-1β, MIP-2γ, and fractalkine [
70]. There are two different types of macrophages, M1 with pro-inflammatory functions and M2 with immunomodulatory functions [
71].
The most predominant and the best-characterized cells of innate immunity throughout pregnancy are NK cells [
76]. It is proposed that peripheral blood NK cells under the influence of cytokines (predominantly IL-15) and hormones (progesterone) proliferate, migrate to the decidua, and differentiate into decidual NK cells by transforming growth factor-beta (TGF-β) and IL-11 [
57]. The decidual NK cells are gaining much attention because their number increases dramatically in the first trimester of pregnancy, reaching over 70% of all decidual lymphocytes [
77].
7. Innate Immunity in AITD and Pregnancy
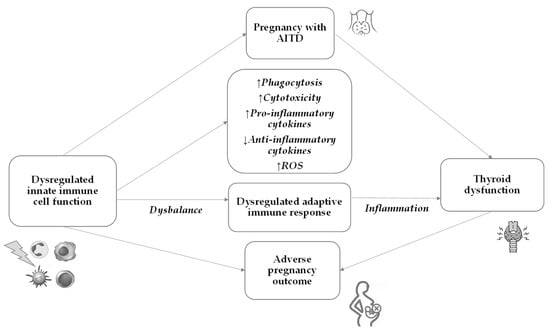
The innate immune system plays a pivotal role in the early recognition and initiation of the immune response against the thyroid gland in AITD. The subsequent activation of the adaptive immune response further perpetuates the autoimmune process, leading to thyroid dysfunction (Figure 2).
Figure 2. Pregnancy outcome in pregnancy with AITD. In pregnancy with AITD, dysregulated innate immune cell function leads to a dysregulated adaptive immune response, which causes thyroid dysfunction and may lead to an adverse pregnancy outcome. AITD—autoimmune thyroid disease; ROS—reactive oxygen species.
The role of immune cells, including macrophages, neutrophils, and DCs, is essential in both the development of AITD and its impact on pregnancy. The immune system undergoes significant changes during pregnancy to prevent the fetus from being rejected as a foreign body. Pregnancy induces a shift toward a more tolerant immune response to accommodate the fetus [
80]. However, the dysregulated immune response in AITD may affect maternal immune adaptations during pregnancy, potentially influencing the risk of pregnancy complications.
8. Emerging Causal Connection: Microbiota and the Thyroid (Dis)balance
It is interesting to mention that studies analyzing the relationship between microbiota composition and thyroid function have been increasing rapidly in recent years. Evidence has been presented about the involvement of the gut microbiota in various aspects of thyroid pathology, which opened a new potential therapeutic target [
137]. Since a healthy gut microbiota has beneficial effects on the activity of the immune system but also on thyroid function, the thyroid–gut axis emerged as a new focus in the field. The gut microbiota influences the availability of vital micronutrients: iodine, iron, and copper are crucial for thyroid hormone synthesis, selenium and zinc are required for converting T4 to T3, and vitamin D is involved in regulating the immune response. Those micronutrients are commonly deficient in AITDs, contributing to thyroid malfunctioning. Therefore, the interplay between gut microbiota and AITD should be taken into consideration when treating patients, especially pregnant women with thyroid diseases [
138]. It has recently been found that gut microbiota exhibits distinctive appearances in patients with AITD, which could be associated with a disbalance in the immune system and gut microbiota [
139].
9. Conclusions
The etiopathogenesis of AITD includes an immune reaction against own body antigens in thyroid cells of genetically susceptible individuals, in interaction with epigenetic and environmental factors. An activated cascade of immunological changes, which leads to the loss of immune tolerance, includes innate immunity, which further activates cells and mediators of adaptive immunity. Trigger antigen in this cascade as well as some other molecular events are still not known. For instance, a new area of investigation is the influence of gut dysbiosis on AITD. Until further studies resolve the background and help in new therapeutical approaches, it is of the utmost importance to identify and manage AITD in pregnant women to avoid adverse pregnancy outcomes and to ensure appropriate development of the newborns’ nervous system. Monitoring the thyroid function and proper thyroid hormone replacement medication are crucial to ensure that thyroid levels are within the appropriate range throughout the pregnancy. Regular follow-up visits and additional blood tests may be required to assess thyroid function and adjust medication dosage as needed. Proper diagnosis and management of autoimmune thyroiditis during pregnancy can significantly reduce the risk of complications for both the mother and the fetus. However, extensive studies are still needed to understand the complex immunopathogenesis of thyroid autoimmunity.
This entry is adapted from the peer-reviewed paper 10.3390/ijms242015442