Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
The exponential growth of artificial intelligence (AI) has allowed for its integration into multiple sectors, including, notably, healthcare. Chatbots have emerged as a pivotal resource for improving patient outcomes and assisting healthcare practitioners through various AI-based technologies. In critical care, kidney-related conditions play a significant role in determining patient outcomes.
- chatbots
- artificial intelligence
- critical care nephrology
- nephrology
1. Features of Chatbots in Critical Care Nephrology
Chatbot technology, which is driven by AI algorithms, has gained considerable attention due to its potential applications across various sectors, including healthcare [1][2]. In critical care nephrology, chatbots possess unique features that can revolutionize patient care, enhance clinical decision making, and improve overall outcomes. This section explores the specific characteristics of chatbots in critical care nephrology and their potential benefits (Figure 1).
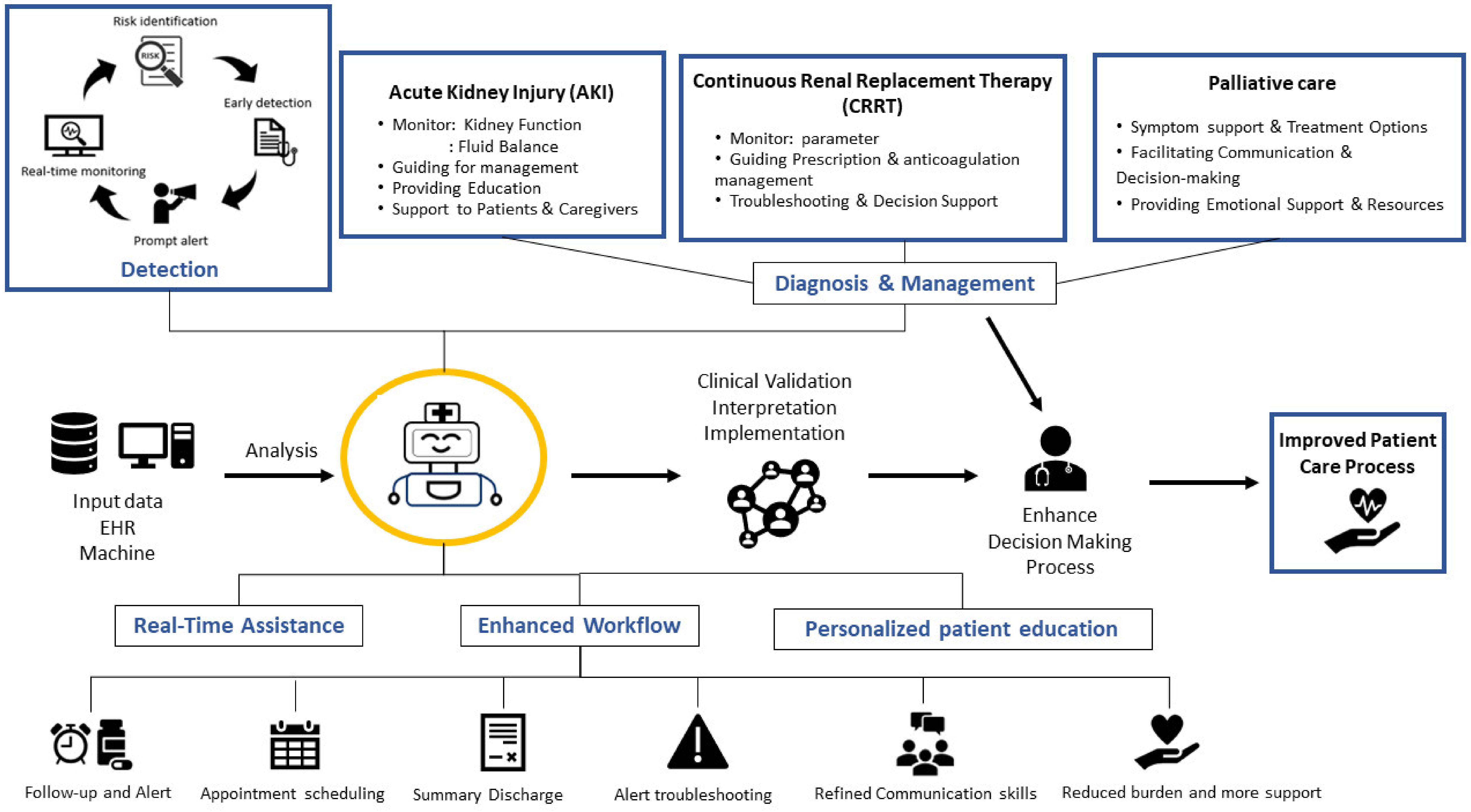
Figure 1. Features and potential uses for chatbots in critical care nephrology.
1.1. Real-Time Assistance and Accessibility
Chatbots can potentially play a pivotal role in critical care nephrology by offering immediate assistance to both patients and healthcare providers [3]. With the backing of advanced AI algorithms, these chatbots provide continuous support, promptly responding to frequent patient inquiries and worries. This capability considerably amplifies healthcare accessibility, ensuring that patients obtain relevant information and backing even beyond traditional clinical operating times [4]. For those grappling with kidney-related challenges, chatbots may emerge as indispensable assets, delivering instant counsel and easing apprehension.
1.2. Data Analysis and Decision Support
The capability of chatbots to analyze extensive patient data [5], including laboratory results, vital signs, and medical histories, is a notable feature. Through AI algorithms, chatbots can identify patterns, detect abnormalities, and provide valuable insights to healthcare providers [6][7]. This feature is especially valuable in critical care nephrology, enabling chatbots to alert healthcare providers to potential complications and suggest appropriate interventions [8]. Real-time data analysis and decision support by chatbots can save crucial time, leading to more-informed decision making, particularly in critical situations where swift actions are vital.
1.3. Personalized Patient Education
Chatbots can be used as tools for providing personalized patient education on various health topics, including conditions, treatment options, and self-management strategies [9][10]. By engaging in conversations with patients, chatbots gather relevant information and offer tailored educational content. A systematic review of randomized control trials on the effectiveness of chatbots in healthcare intervention demonstrated that implementing chatbots is feasible and positively affects physical functioning, healthy lifestyle, mental health, and psychosocial outcomes. Furthermore, chatbots could support patient health before or after medical treatment [11]. In critical care nephrology, this feature proves beneficial for patients with kidney-related issues who require comprehensive understanding and guidance [12]. Such tools can provide detailed information on medication compliance, dietary limitations, and necessary lifestyle changes. This enables patients to actively engage in their healthcare, which can lead to improved overall health results [13].
1.4. Access to Medical Literature and Guidelines
Healthcare professionals in critical care nephrology can leverage chatbots to access up-to-date medical literature, guidelines, and protocols [14]. By integrating chatbots with relevant databases and resources, healthcare providers can quickly retrieve accurate and evidence-based information [15][16]. This feature ensures that healthcare professionals can access the latest research, treatment guidelines, and best practices, enabling them to make informed decisions and deliver evidence-based care. It also supports continuous professional development by facilitating easy access to educational materials.
1.5. Language Processing and Multilingual Support
Chatbots equipped with advanced natural language processing capabilities excel in understanding and responding to patients’ queries and concerns effectively [1][17]. In critical care nephrology, where clear communication is crucial, this feature becomes highly valuable. Chatbots can interpret complex medical terminologies and provide explanations in layman’s terms, enhancing patient understanding and engagement. Furthermore, chatbots can offer multilingual support, overcoming language barriers and ensuring that patients from diverse backgrounds can access the care they need [18].
1.6. Integration with EHRs
To maximize their effectiveness, chatbots can seamlessly integrate with EHR systems. This integration allows chatbots to access patients’ medical histories, test results, and treatment plans, compiling a comprehensive patient health status [19]. By retrieving and analyzing relevant data in real time, chatbots can offer personalized recommendations and reminders, improving care coordination and treatment adherence. This feature streamlines the workflow for healthcare providers, enabling them to make more informed decisions based on up-to-date patient information [20][21].
1.7. Privacy and Security Measures
Given the sensitive nature of healthcare data, implementing robust privacy and security measures is crucial when integrating chatbots [22]. Measures such as robust encryption, authentication mechanisms, and strict data governance protocols should be in place to preserve patient privacy and maintain compliance with relevant regulations [23]. Ensuring data confidentiality and implementing secure data storage practices are essential to building trust among patients and healthcare providers.
2. Potential Applications of Chatbots in Critical Care Nephrology
As the management of kidney-related conditions in critically ill patients becomes increasingly complex, chatbots offer a potential novel approach to addressing various challenges and improving patient outcomes (Figure 2).
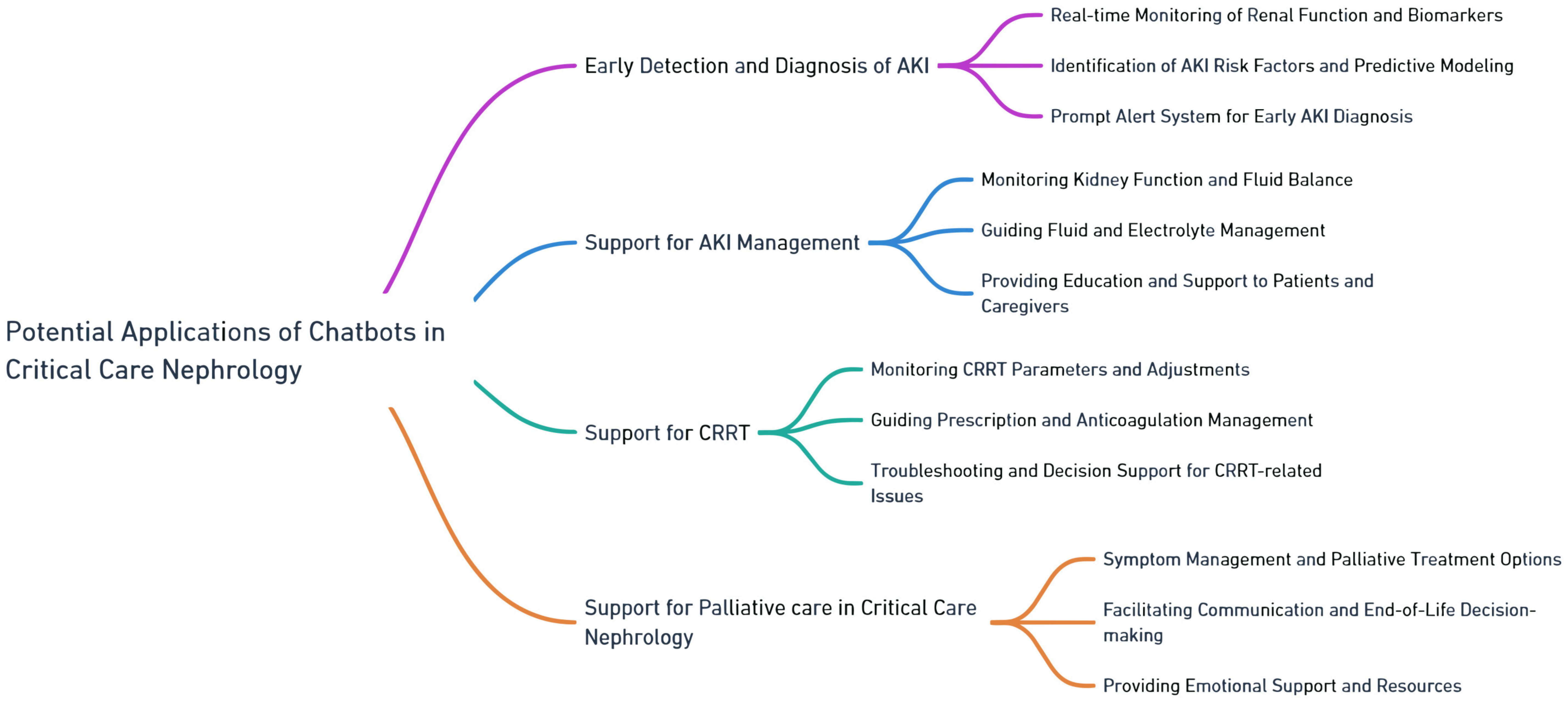
Figure 2. Potential applications of chatbots in critical care nephrology.
2.1. Early Detection and Diagnosis of AKI
Critical care nephrology is a specialized discipline involving the management of kidney-related conditions in critically ill patients. The implementation of chatbots in critical care nephrology has demonstrated potential in enhancing patient outcomes by enabling the early detection and diagnosis of AKI [24][25][26]. This section will explore the unique uses of chatbots in critical care nephrology, such as the real-time monitoring of renal function and biomarkers, the identification of AKI risk factors, and the development of a prompt alert system for early AKI diagnosis.
2.1.1. Real-Time Monitoring of Renal Function and Biomarkers
The integration of chatbots offers promising avenues in the continuous monitoring of renal function and biomarkers for critically ill patients. With seamless connections to EHRs and laboratory systems, chatbots are well-positioned to collect and interpret real-time data, which includes serum creatinine levels [27][28], urine output [5], and other relevant parameters [29]. Through advanced NLP algorithms, chatbots hold the potential to translate these data into actionable insights, offering healthcare providers immediate updates and aiding in the early identification of AKI [30].
By actively monitoring renal function and biomarkers in real time [28][31], chatbots present healthcare providers with the opportunity to observe shifts and swiftly pinpoint irregularities. For example, should a patient’s creatinine levels surpass a specified limit, the chatbot might produce an alert, suggesting that healthcare professionals delve deeper and perhaps consider timely interventions to curb the progression of AKI [32].
2.1.2. Identification of AKI Risk Factors and Predictive Modeling
Chatbots offer the potential to aid in pinpointing risk factors linked with AKI by accumulating patient-centric data and applying predictive modeling algorithms. Through dialogues with patients or caregivers, chatbots gather details about medical history, comorbidities, medications, and physiological parameters [7][28][33]. Utilizing machine learning techniques, chatbots can potentially analyze this information to discern risk factors leading to AKI development.
Employing predictive modeling, chatbots could produce risk scores or probabilities that denote the chance of AKI manifestation in critically ill patients [34]. This information equips healthcare providers with valuable insights to prioritize interventions, allocate resources effectively, and implement preventive measures to mitigate the risk of AKI [28][32][35]. For example, should a chatbot identify a patient with several AKI risk factors, it might suggest that healthcare professionals consider interventions like fine-tuning fluid management, recalibrating medication dosages, or adopting renal protective approaches.
2.1.3. Prompt Alert System for Early AKI Diagnosis
The timely diagnosis of AKI poses a significant challenge in its management. Chatbots address this challenge by serving as prompt alert systems for the early detection of AKI. Through uninterrupted monitoring of patient data, encompassing renal function parameters and AKI risk determinants, chatbots might generate notifications upon specific criteria being fulfilled or certain thresholds being reached [36].
When a chatbot identifies an abnormal trend or a combination of risk factors indicative of potential AKI, it could immediately inform healthcare providers. This early alert system empowers healthcare teams to initiate diagnostic evaluations, implement appropriate interventions, and prevent further renal damage [37][38][39]. Moreover, chatbots might enhance decision making by recommending specific diagnostic procedures or strategies, all rooted in evidence-backed guidelines or institutional directives [32][40][41].
2.2. Support for AKI Management
AKI is a critical condition characterized by the sudden loss of kidney function, leading to the accumulation of waste products and imbalances in bodily fluids. Kidney replacement therapy, such as dialysis or CRRT, is crucial in managing AKI. The integration of chatbots in supporting AKI and CRRT management holds promise with regard to amplifying patient outcomes by assisting in various aspects of care [42][43]. This section explores the specific applications of chatbots within the context of AKI and CRRT management.
2.2.1. Monitoring Kidney Function and Fluid Balance
Chatbots offer the possibility of aiding in the observation of kidney function and fluid equilibrium in AKI patients. Through seamless connections with electronic health records and laboratory systems, chatbots might gather and interpret real-time data points, encompassing serum creatinine levels, urine production, and fluid consumption and excretion [5]. With such data at their disposal, chatbots are well-poised to provide healthcare professionals with consistent updates on kidney functionality trends and fluid conditions [8].
Employing machine learning algorithms, chatbots could discern patterns and departures from typical benchmarks, alerting healthcare experts to crucial shifts or the exacerbation of AKI [36]. Such insights equip medical teams with the foundation for swift response measures, be it modulating fluid treatments or commencing kidney replacement therapies, aiming to avert complications and enhance patient results [44].
2.2.2. Guiding Fluid and Electrolyte Management
Fluid and electrolyte management is critical to AKI care. Chatbots present the opportunity to bolster healthcare providers’ decision-making processes concerning fluid balance, electrolyte substitution, and medication modifications.
By analyzing patient-centric data regarding fluid consumption and expulsion, electrolyte metrics, and medication profiles, chatbots might propose strategies for fluid and electrolyte management [8][45]. These digital assistants could recommend suitable fluid revival volumes, the nature of fluids (for instance, isotonic or colloid), and the pace of dispensation, all tailored to the patient’s clinical state and distinct requirements.
In addition, chatbots hold the potential to provide guidance regarding electrolyte replenishment, such as recalibrating potassium or sodium concentrations, with due regard to renal performance and broader patient stability. Such insights play a role in averting electrolyte disparities and facilitating the reestablishment of regular physiological benchmarks [43].
2.2.3. Providing Education and Support to Patients and Caregivers
Chatbots may act as invaluable educational platforms for AKI patients and their caregivers, delivering guidance and backing throughout the care journey. These digital assistants might offer tailored counsel on kidney health [45][46], lifestyle modifications, and self-care practices to promote recovery or prevent further kidney damage [47][48][49].
With the integration of evidence-rooted resources and instructive content [50], chatbots may potentially educate patients and caregivers about AKI causes, symptoms, and the importance of adherence to prescribed treatments [51]. Furthermore, chatbots might oversee medication oversight, elucidating the correct deployment and probable adverse reactions of drugs pivotal to AKI treatment (Figure 3).
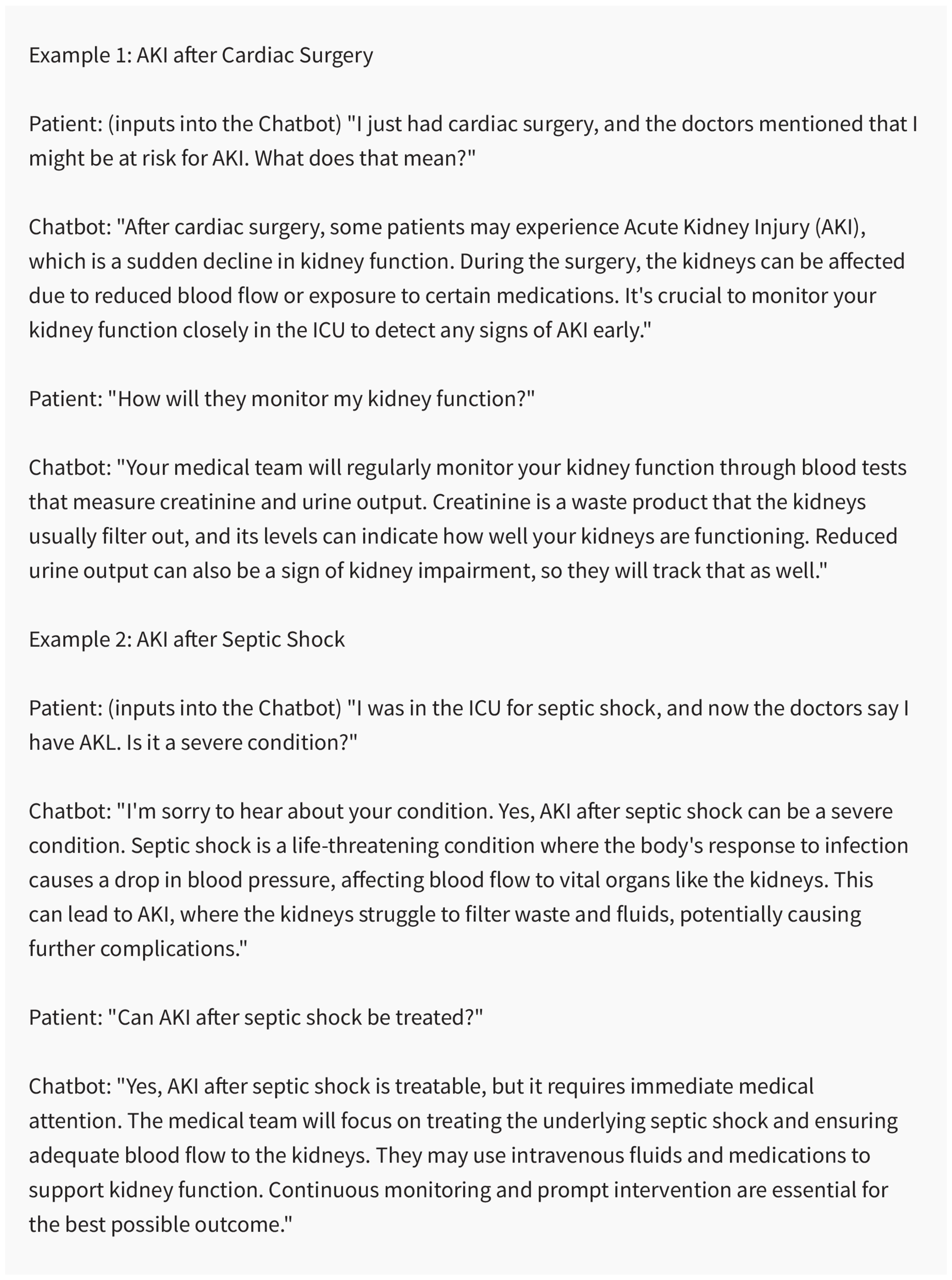
Figure 3. Chatbots serving as valuable educational tools for AKI patients. Created using ChatGPT 3.5.
Furthermore, chatbots might present timely reminders for subsequent appointments, laboratory tests, and medication schedules, promoting patient engagement and compliance with the recommended treatment plan [8][45][49]. These digital assistants are well-placed to tackle patient questions, soothe anxieties, and extend emotional backing, augmenting the holistic patient journey and paving the way for improved results in AKI management [52].
2.3. Support for CRRT
CRRT is a widely utilized method for kidney replacement therapy in the management of AKI and other kidney-related conditions [53][54]. The inclusion of chatbots in the orchestration of CRRT management holds promise in amplifying patient outcomes, providing support throughout diverse care dimensions [31][53][54]. This section examines potential the specific development applications of chatbots within the context of CRRT management.
2.3.1. Monitoring CRRT Parameters and Adjustments
In the context of CRRT, chatbots could play a crucial role in monitoring parameters and guiding adjustments to optimize treatment. By seamlessly integrating with CRRT machines and electronic health records, these bots have the potential to collect real-time data on critical factors like blood flow rates, dialysate flow rates, ultrafiltration rates, and other relevant parameters [55].
Leveraging machine learning algorithms, chatbots have the potential capacity to perpetually interpret data, positioning themselves to supply healthcare professionals with up-to-date information regarding the efficacy of CRRT. Such chatbots might discern patterns, detect deviations from desired targets, and promptly alert healthcare providers to significant changes or potential issues that may arise [31][44].
By actively monitoring CRRT parameters, chatbots might assist healthcare teams in undertaking timely interventions by providing data guidance support, such as fine-tuning blood flow rates, adjusting dialysate composition, or modifying ultrafiltration rates. This proactive approach helps maintain proper fluid and electrolyte balance, optimize solute clearance, and minimize the risk of complications associated with CRRT.
2.3.2. Guiding Prescription and Anticoagulation Management
Chatbots might emerge as instrumental assets in aiding healthcare providers with orchestrating prescription and anticoagulation management for CRRT. By accessing patient-centric data, which includes weight, clinical status, and laboratory findings, chatbots hold the potential to suggest prescription configurations, such as suitable dosages and therapeutic durations [54][56].
Chen et al. [56] demonstrated the good performance and feasibility of using AI deep neural network models to detect and determine how to adjust the dose of regional citrate anticoagulant (RCA) to avoid citric acid overdose in CRRT patients by conducting an analysis of patient-specific parameters, such as coagulation profiles and bleeding risk factors. The overall accuracy of the neural network models was 90.77%. Even in anticoagulant-free patients, Zhang et al. validated and used AI to guide and predict filter lifespan among CRRT patients [57]. The findings showed that the internal validation model and area under the curve were 0.8 (95% CI (0.74–0.87) and 0.82 (95% confidence interval (CI) (0.76–0.88)), respectively.
Such chatbot assistance ensures the safe and effective delivery of CRRT, thereby minimizing the risk of clotting or bleeding complications arising from insufficient or excessive anticoagulation.
2.3.3. Facilitating Troubleshooting and Providing Decision Support for CRRT-Related Issues
Chatbots are potentially valuable sources of troubleshooting support and decision-making assistance for CRRT-related issues (Figure 4). In instances of alarms or technical difficulties with CRRT machines, chatbots might offer sequential guidance for foundational troubleshooting and issue mitigation.
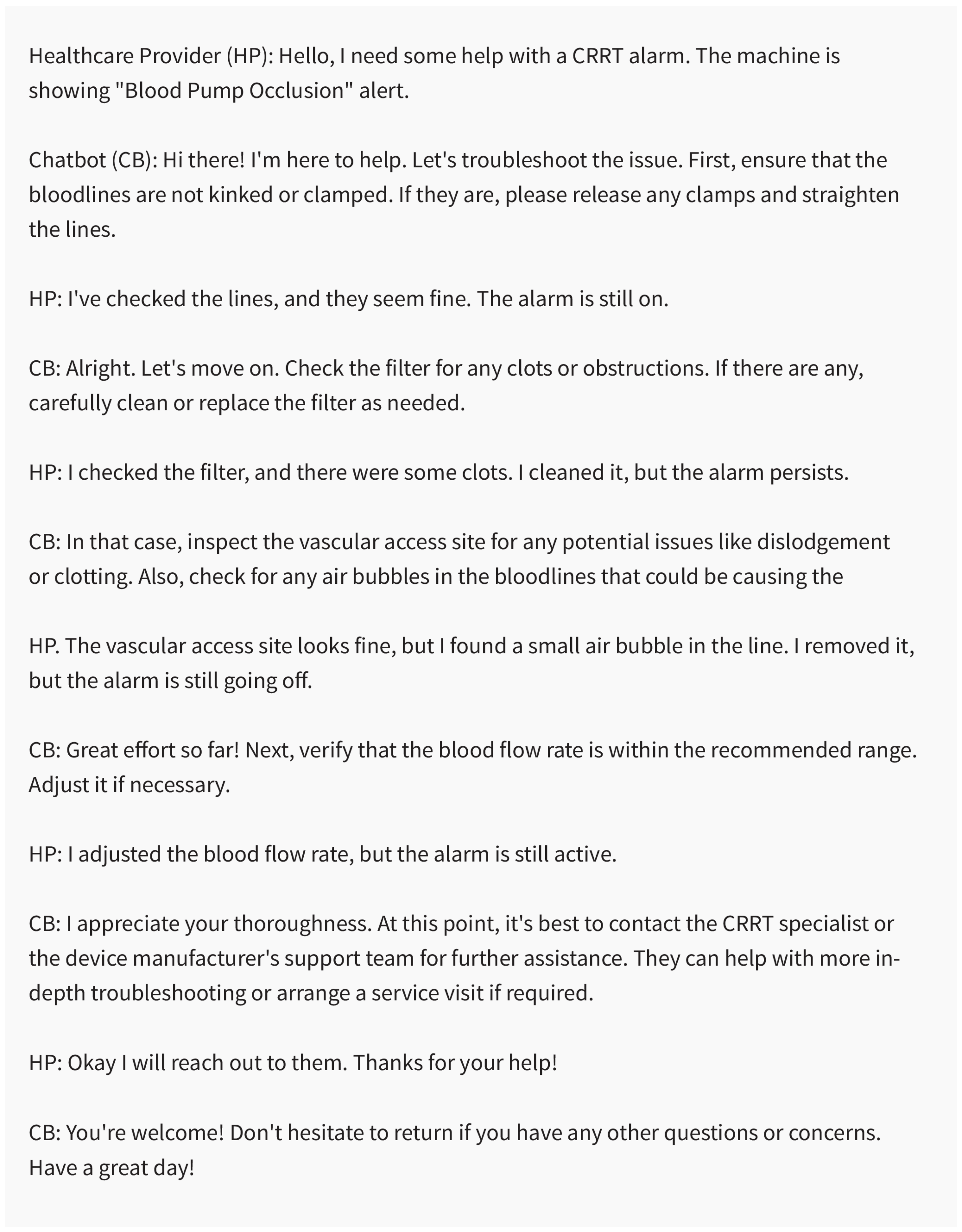
Figure 4. The chatbot provides troubleshooting support for the CRRT alarm, and the healthcare provider follows the recommended steps to resolve the issue. Created using ChatGPT 3.5.
Furthermore, chatbots can act as decision support tools by integrating clinical guidelines and expert knowledge. When confronted with complex situations or uncertainties in CRRT management, healthcare providers might turn to chatbots to acquire evidence-rooted suggestions and counsel.
For example, if an adjustment to the CRRT prescription is necessitated due to changing patient conditions or the need to address specific complications, chatbots might proffer insights on fitting alterations grounded in optimal practices and clinical standards.
Furthermore, chatbots hold the potential to aid in determining the ideal span for CRRT. Through analysis of patient-specific factors such as fluid balance, kidney function recovery, and clinical stability, chatbots might guide healthcare professionals in discerning the right moment to cease CRRT and shift to other renal replacement therapies or supportive care strategies.
2.4. Support for Palliative Care in Critical Care Nephrology
The deployment of chatbots presents distinct merits and backup options within the realm of palliative care in critical care nephrology [58]. These automated dialogue facilitators have the capacity to elevate patient journeys and proffer invaluable assets [59]. Below is an exploration of the roles chatbots might play within the aforementioned spheres of palliative care.
2.4.1. Assisting with Symptom Management and Palliative Treatment Options
Chatbots are poised to dispense tailored data and backing for symptom oversight [60][61]. In the previously mentioned study, which investigated the interaction between 958 cancer patients and chatbots in monitoring patients’ symptoms and concerns, 132,970 message interactions were observed per month. The study showed that receiving medical reminders and accessing information via chatbots positively impacted patient satisfaction by 94%. Additionally, the chatbots helped and supported patients to effectively follow their treatment, with a success rate of 88% [9]. Another noninferiority RCT study compared chatbots and physicians regarding ability to give patients information and was conducted on 141 breast cancer patients. The findings revealed that the perceived quality of the answer by the chatbot was found to be non-inferior to the scores of the physicians. The success rates of the chatbot and physician groups were 69% and 64%, respectively (Figure 5). Patient satisfaction rates were 85% and 81% for the chatbot and physician groups, and the rates of helpful answers were 85% and 83%, respectively. The findings revealed that 62% of patients overall needed additional information: 65% in the physician group, and 59% in the chatbot group [62].
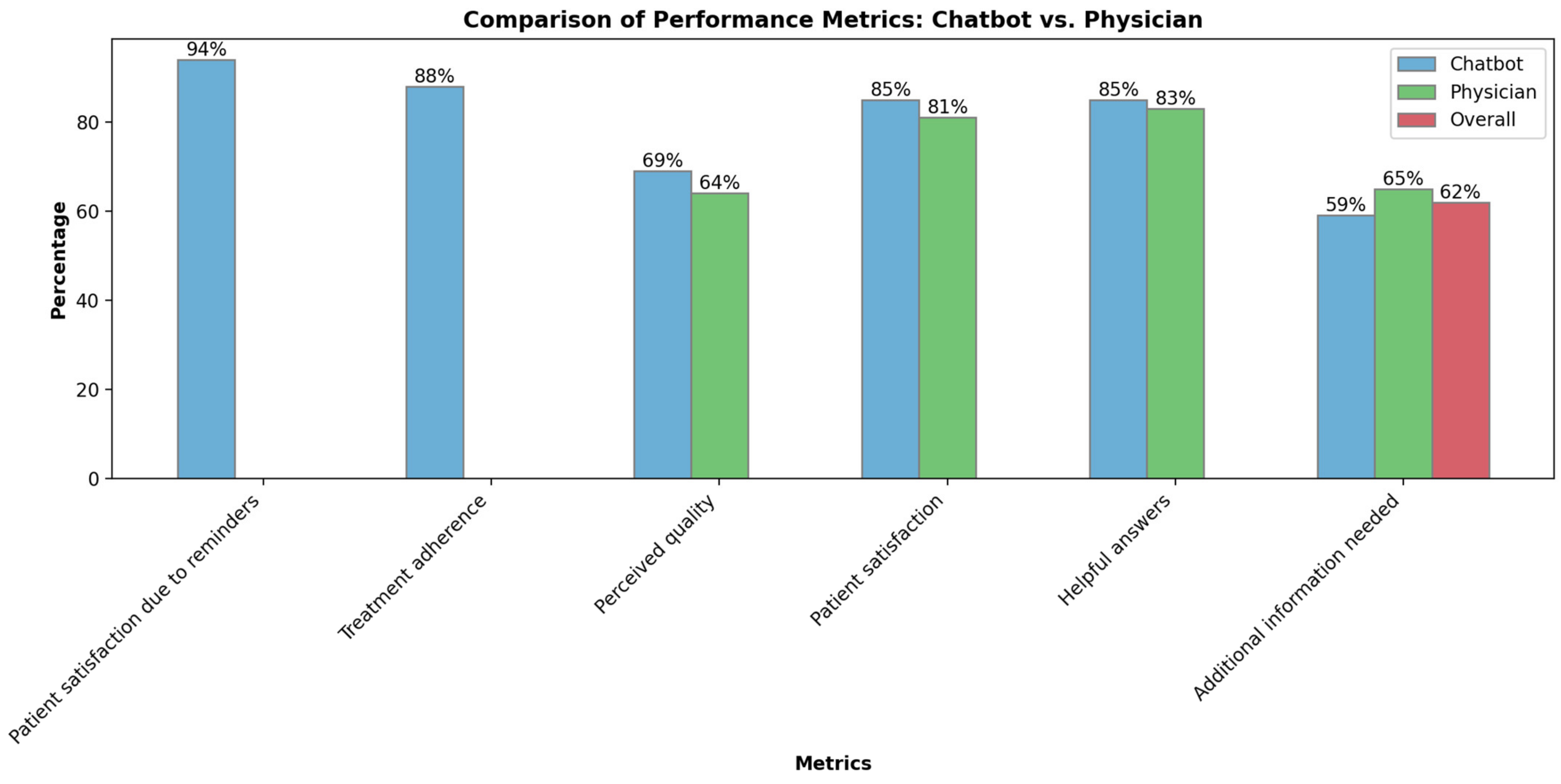
Figure 5. Performance metric comparisons between chatbots and physicians.
Patients might interact with the chatbot to detail their symptoms, and reciprocally, the chatbot could suggest an array of techniques for easing discomfort, such as breathing drills or relaxation methodologies. Moreover, chatbots have the capacity to dispatch medication alerts and tackle prevalent inquiries about palliative treatment alternatives, like palliative dialysis. Employing natural language processing, chatbots might partake in dynamic dialogues, tailoring their feedback to each patient’s distinct requirements and predilections [46][63][64]. Chatbots hold promise in guiding healthcare professionals in risk classification by tapping into data from EHRs and identifying patients with potential risks associated with specific treatment procedures [65]. Chatbots may determine whether patients would benefit from a meeting with a palliative care team, or create a comprehensive care plan to enhance the quality of life for patients with critical illnesses [66][67][68][69].
2.4.2. Facilitating Communication and End-of-Life Decision Making
Chatbots stand well-poised to amplify communication efficacy by providing patients and their kin with precise and dependable data about prognosis, accessible treatment avenues, and prospective outcomes [9][64][70]. Patients might engage in dialogues with the chatbot to delve deeper into the advantages and potential pitfalls aligned with diverse treatment options [46][70][71]. In addition, chatbots could play a role in documenting patients’ inclinations concerning end-of-life care, revival, and medical maneuvers. Steering patients through these deliberations and ensuring the meticulous recording of their choices, chatbots play a part in enlightened decision making at pivotal junctures [12][72]. Moreover, chatbots can potentially assist the healthcare team in developing and refining effective communication skills within challenging situations such as end-of-life care and breaking bad news [73]. Chatbots might facilitate simulated case scenarios, refining language and tone in a risk-free environment, and give feedback. Consequently, this practice would enable better management of patients’ emotional responses and foster trust during critical moments [59].
2.4.3. Providing Emotional Support and Resources
Chatbots hold immense potential as readily available platforms, offering emotional support to patients and their families during the challenging phases of palliative care (Figure 6). They possess the ability to engage in active listening and voice interaction [50], detect patients’ concerns and emotional status through tone analysis [20][21], and give empathic responses [63][73][74]. Beyond that, chatbots might supply authenticated data and proffer resources connected to coping strategies, grief guidance [75], and community support groups [70][76].
Figure 6. Chatbots serving as accessible sources of emotional support for patients. Created using ChatGPT 3.5.
Chatbots extend emotional support beyond the confines of physical healthcare settings by connecting patients and families with relevant resources and providing guidance.
Chatbots stand well-poised to act as virtual collaborators, allowing healthcare providers to navigate intricate and sensitive facets with heightened proficiency and empathy [77]. Chatbots can assist with navigating critical conversations, meaningful engagement, and support for patients and their families in the context of advance care planning and palliative care. Additionally, using chatbots could help alleviate emotional burden, reducing communication-related errors and misunderstandings, improving satisfaction, having a meaningful and positive impact on quality of life, and providing holistic care [64].
It remains vital to discern that, though chatbots might lend considerable support in palliative care, they are not meant to eclipse the innate human bond and individualized care rendered by medical experts [78]. Chatbots should be incorporated as complementary tools that enhance the services provided by palliative care teams, rather than seeking to replace them. Human oversight and intervention should be readily available to address complex situations and ensure patients receive appropriate care tailored to their circumstances. In comprehensive healthcare, chatbots play a significant role in offering valuable support. However, it is imperative to acknowledge that chatbots cannot act as substitutes for essential humanization and personalized doctor–patient interaction, which remains a crucial aspect of healthcare that professionals provide [78]. Instead, chatbots should be viewed as supplementary tools that augment services and alleviate the burden on the healthcare team. Particularly in intricate and demanding situations, the presence of healthcare professionals is indispensable, providing oversight and intervention to ensure patients receive holistic care tailored to their unique circumstances, with the warmth and compassion that only human beings can offer.
This entry is adapted from the peer-reviewed paper 10.3390/medicines10100058
References
- Ali, O.; Abdelbaki, W.; Shrestha, A.; Elbasi, E.; Alryalat, M.A.A.; Dwivedi, Y.K. A systematic literature review of artificial intelligence in the healthcare sector: Benefits, challenges, methodologies, and functionalities. J. Innov. Knowl. 2023, 8, 100333.
- Darcy, A.M.; Louie, A.K.; Roberts, L.W. Machine Learning and the Profession of Medicine. JAMA 2016, 315, 551–552.
- Hueso, M.; Vellido, A.; Montero, N.; Barbieri, C.; Ramos, R.; Angoso, M.; Cruzado, J.M.; Jonsson, A. Artificial Intelligence for the Artificial Kidney: Pointers to the Future of a Personalized Hemodialysis Therapy. Kidney Dis. 2018, 4, 1–9.
- Schario, M.E.; Bahner, C.A.; Widenhofer, T.V.; Rajaballey, J.I.; Thatcher, E.J. Chatbot-assisted care management. Prof. Case Manag. 2022, 27, 19–25.
- Schwager, E.; Lanius, S.; Ghosh, E.; Eshelman, L.; Pasupathy, K.S.; Barreto, E.F.; Kashani, K. Including urinary output to define AKI enhances the performance of machine learning models to predict AKI at admission. J. Crit. Care 2021, 62, 283–288.
- Thongprayoon, C.; Kattah, A.G.; Mao, M.A.; Keddis, M.T.; Pattharanitima, P.; Vallabhajosyula, S.; Nissaisorakarn, V.; Erickson, S.B.; Dillon, J.J.; Garovic, V.D.; et al. Distinct phenotypes of hospitalized patients with hyperkalemia by machine learning consensus clustering and associated mortality risks. QJM 2022, 115, 442–449.
- De Vlieger, G.; Kashani, K.; Meyfroidt, G. Artificial intelligence to guide management of acute kidney injury in the ICU: A narrative review. Curr. Opin. Crit. Care 2020, 26, 563–573.
- Celi, L.A.; Hinske Christian, L.; Alterovitz, G.; Szolovits, P. An artificial intelligence tool to predict fluid requirement in the intensive care unit: A proof-of-concept study. Crit. Care 2008, 12, R151.
- Chaix, B.; Bibault, J.-E.; Pienkowski, A.; Delamon, G.; Guillemassé, A.; Nectoux, P.; Brouard, B. When chatbots meet patients: One-year prospective study of conversations between patients with breast cancer and a chatbot. JMIR Cancer 2019, 5, e12856.
- Kadariya, D.; Venkataramanan, R.; Yip, H.Y.; Kalra, M.; Thirunarayanan, K.; Sheth, A. kBot: Knowledge-Enabled Personalized Chatbot for Asthma Self-Management. In Proceedings of the 2019 IEEE International Conference on Smart Computing (SMARTCOMP), Washington, DC, USA, 12–15 June 2019; pp. 138–143.
- Li, Y.; Liang, S.; Zhu, B.; Liu, X.; Li, J.; Chen, D.; Qin, J.; Bressington, D. Feasibility and effectiveness of artificial intelligence-driven conversational agents in healthcare interventions: A systematic review of randomized controlled trials. Int. J. Nurs. Stud. 2023, 143, 104494.
- Furtado, E.S.; Oliveira, F.; Pinheiro, V. Conversational Assistants and their Applications in Health and Nephrology. In Innovations in Nephrology: Breakthrough Technologies in Kidney Disease Care; Bezerra da Silva Junior, G., Nangaku, M., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 283–303.
- Tsai, W.-C.; Li, W.-Y.; Tsai, J.-Y.; Yang, J.-S. Improving Self-diet Management of Chronic Kidney Disease Patients Through Chatbots. In Proceedings of the Human Aspects of IT for the Aged Population, Technology in Everyday Living, Virtual Event, 26 June–1 July 2022; pp. 268–276.
- Sallam, M. ChatGPT Utility in Healthcare Education, Research, and Practice: Systematic Review on the Promising Perspectives and Valid Concerns. Healthcare 2023, 11, 887.
- Miao, J.; Thongprayoon, C.; Cheungpasitporn, W. Assessing the Accuracy of ChatGPT on Core Questions in Glomerular Disease. Kidney Int. Rep. 2023, 8, 1657–1659.
- Vaishya, R.; Misra, A.; Vaish, A. ChatGPT: Is this version good for healthcare and research? Diabetes Metab. Syndr. Clin. Res. Rev. 2023, 17, 102744.
- Olujimi, P.A.; Ade-Ibijola, A. NLP techniques for automating responses to customer queries: A systematic review. Discov. Artif. Intell. 2023, 3, 20.
- Badlani, S.; Aditya, T.; Dave, M.; Chaudhari, S. Multilingual Healthcare Chatbot Using Machine Learning. In Proceedings of the 2021 2nd International Conference for Emerging Technology (INCET), Belagavi, India, 21–23 May 2021; pp. 1–6.
- Lal, H.; Lal, P. NLP chatbot for Discharge Summaries. In Proceedings of the 2019 2nd International Conference on Intelligent Communication and Computational Techniques (ICCT), Jaipur, India, 28–29 September 2019; pp. 250–257.
- Lu, Y.; Wu, H.; Qi, S.; Cheng, K. Artificial Intelligence in Intensive Care Medicine: Toward a ChatGPT/GPT-4 Way? Ann. Biomed. Eng. 2023, 51, 1898–1903.
- Ralston, K.; Chen, Y.; Isah, H.; Zulkernine, F. A Voice Interactive Multilingual Student Support System using IBM Watson. In Proceedings of the 2019 18th IEEE International Conference On Machine Learning And Applications (ICMLA), Boca Raton, FL, USA, 16–19 December 2019; pp. 1924–1929.
- Haupt, C.E.; Marks, M. AI-Generated Medical Advice—GPT and Beyond. JAMA 2023, 329, 1349–1350.
- Marks, M.; Haupt, C.E. AI Chatbots, Health Privacy, and Challenges to HIPAA Compliance. JAMA 2023, 330, 309–310.
- Schwager, E.; Ghosh, E.; Eshelman, L.; Pasupathy, K.S.; Barreto, E.F.; Kashani, K. Accurate and interpretable prediction of ICU-acquired AKI. J. Crit. Care 2023, 75, 154278.
- Kashani, K.B. Automated acute kidney injury alerts. Kidney Int. 2018, 94, 484–490.
- Ostermann, M.; Zarbock, A.; Goldstein, S.; Kashani, K.; Macedo, E.; Murugan, R.; Bell, M.; Forni, L.; Guzzi, L.; Joannidis, M.; et al. Recommendations on Acute Kidney Injury Biomarkers From the Acute Disease Quality Initiative Consensus Conference: A Consensus Statement. JAMA Netw. Open 2020, 3, e2019209.
- Ghosh, E.; Eshelman, L.; Lanius, S.; Schwager, E.; Pasupathy, K.S.; Barreto, E.F.; Kashani, K. Estimation of Baseline Serum Creatinine with Machine Learning. Am. J. Nephrol. 2021, 52, 753–762.
- Dong, J.; Feng, T.; Thapa-Chhetry, B.; Cho, B.G.; Shum, T.; Inwald, D.P.; Newth, C.J.L.; Vaidya, V.U. Machine learning model for early prediction of acute kidney injury (AKI) in pediatric critical care. Crit. Care 2021, 25, 288.
- Thongprayoon, C.; Hansrivijit, P.; Bathini, T.; Vallabhajosyula, S.; Mekraksakit, P.; Kaewput, W.; Cheungpasitporn, W. Predicting Acute Kidney Injury after Cardiac Surgery by Machine Learning Approaches. J. Clin. Med. 2020, 9, 1767.
- Song, X.; Liu, X.; Liu, F.; Wang, C. Comparison of machine learning and logistic regression models in predicting acute kidney injury: A systematic review and meta-analysis. Int. J. Med. Inform. 2021, 151, 104484.
- Lin, C.H.; Ho, T.F.; Chen, H.F.; Chang, H.Y.; Chien, J.H. Applying Healthcare Failure Mode and Effect Analysis and the Development of a Real-Time Mobile Application for Modified Early Warning Score Notification to Improve Patient Safety During Hemodialysis. J. Patient Saf. 2022, 18, 475–485.
- Lachance, P.; Villeneuve, P.-M.; Rewa, O.G.; Wilson, F.P.; Selby, N.M.; Featherstone, R.M.; Bagshaw, S.M. Association between e-alert implementation for detection of acute kidney injury and outcomes: A systematic review. Nephrol. Dial. Transplant. 2017, 32, 265–272.
- Zhu, W.; Barreto, E.F.; Li, J.; Lee, H.K.; Kashani, K. Drug-drug interaction and acute kidney injury development: A correlation-based network analysis. PLoS ONE 2023, 18, e0279928.
- Mistry, N.S.; Koyner, J.L. Artificial Intelligence in Acute Kidney Injury: From Static to Dynamic Models. Adv. Chronic. Kidney Dis. 2021, 28, 74–82.
- Wang, Y.; Wei, Y.; Yang, H.; Li, J.; Zhou, Y.; Wu, Q. Utilizing imbalanced electronic health records to predict acute kidney injury by ensemble learning and time series model. BMC Med. Inform. Decis. Mak. 2020, 20, 238.
- Thongprayoon, C.; Pattharanitima, P.; Kattah, A.G.; Mao, M.A.; Keddis, M.T.; Dillon, J.J.; Kaewput, W.; Tangpanithandee, S.; Krisanapan, P.; Qureshi, F.; et al. Explainable Preoperative Automated Machine Learning Prediction Model for Cardiac Surgery-Associated Acute Kidney Injury. J. Clin. Med. 2022, 11, 6264.
- Chiofolo, C.; Chbat, N.; Ghosh, E.; Eshelman, L.; Kashani, K. Automated continuous acute kidney injury prediction and surveillance: A random forest model. Mayo Clin. Proc. 2019, 94, 783–792.
- Cheungpasitporn, W.; Kashani, K. Electronic Data Systems and Acute Kidney Injury. Contrib. Nephrol. 2016, 187, 73–83.
- Sutherland, S.M.; Chawla, L.S.; Kane-Gill, S.L.; Hsu, R.K.; Kramer, A.A.; Goldstein, S.L.; Kellum, J.A.; Ronco, C.; Bagshaw, S.M.; Group, A.C. Utilizing electronic health records to predict acute kidney injury risk and outcomes: Workgroup statements from the 15th ADQI Consensus Conference. Can. J. Kidney Health Dis. 2016, 3, 99.
- Ostermann, M.; Liu, K.; Kashani, K. Fluid Management in Acute Kidney Injury. Chest 2019, 156, 594–603.
- Shawwa, K.; Kashani, K.B. Prevention and Management of the Critically Injured Kidney. Int. Anesthesiol. Clin. 2019, 57, 48–60.
- Kotanko, P.; Zhang, H.; Wang, Y. Artificial Intelligence and Machine Learning in Dialysis: Ready for Prime Time? Clin. J. Am. Soc. Nephrol. 2023, 18, 803–805.
- Pack, S.; Lee, J. Randomised controlled trial of a smartphone application-based dietary self-management program on haemodialysis patients. J. Clin. Nurs. 2021, 30, 840–848.
- Barbieri, C.; Cattinelli, I.; Neri, L.; Mari, F.; Ramos, R.; Brancaccio, D.; Canaud, B.; Stuard, S. Development of an Artificial Intelligence Model to Guide the Management of Blood Pressure, Fluid Volume, and Dialysis Dose in End-Stage Kidney Disease Patients: Proof of Concept and First Clinical Assessment. Kidney Dis. 2019, 5, 28–33.
- Torabi Khah, M.; Farsi, Z.; Sajadi, S.A. Comparing the effects of mHealth application based on micro-learning method and face-to-face training on treatment adherence and perception in haemodialysis patients: A randomised clinical trial. BMJ Open 2023, 13, e071982.
- da Silva Junior, G.B.; de Oliveira, J.G.R.; de Araújo, E.M.R.; Albuquerque, A.; Mota, F.A.X.; de Freitas Filho, R.A.; de Vasconcelos Filho, J.E.; Rodrigues, M.A.F. Renal Health: Providing Information and Technological Tools to Empower Patients to Live Better with Kidney Disease. Stud. Health Technol. Inform. 2021, 281, 674–678.
- Campbell, J.; Porter, J. Dietary mobile apps and their effect on nutritional indicators in chronic renal disease: A systematic review. Nephrology 2015, 20, 744–751.
- Li, W.-Y.; Chiu, F.-C.; Zeng, J.-K.; Li, Y.-W.; Huang, S.-H.; Yeh, H.-C.; Cheng, B.-W.; Yang, F.-J. Mobile health app with social media to support self-management for patients with chronic kidney disease: Prospective randomized controlled study. J. Med. Internet Res. 2020, 22, e19452.
- Malkina, A.; Tuot, D.S. Role of telehealth in renal replacement therapy education. Semin. Dial. 2018, 31, 129–134.
- May, R.; Denecke, K. Extending patient education with CLAIRE: An interactive virtual reality and voice user interface application. In Proceedings of the Addressing Global Challenges and Quality Education: 15th European Conference on Technology Enhanced Learning, EC-TEL 2020, Heidelberg, Germany, 14–18 September 2020; Proceedings 15, 2020. pp. 482–486.
- Torabikhah, M.; Farsi, Z.; Sajadi, S.A. Comparing the effects of mHealth app use and face-to-face training on the clinical and laboratory parameters of dietary and fluid intake adherence in hemodialysis patients: A randomized clinical trial. BMC Nephrol. 2023, 24, 194.
- Singh, K. Mobile Health in Dialysis: The Best Engagement Medium Is the One that’s with Patients. Clin. J. Am. Soc. Nephrol. 2021, 16, 12–13.
- Hammouda, N.; Neyra, J.A. Can Artificial Intelligence Assist in Delivering Continuous Renal Replacement Therapy? Adv. Chronic Kidney Dis. 2022, 29, 439–449.
- Liu, L.J.; Takeuchi, T.; Chen, J.; Neyra, J.A. Artificial Intelligence in Continuous Kidney Replacement Therapy. Clin. J. Am. Soc. Nephrol. 2023, 18, 671–674.
- Zhang, L.; Baldwin, I.; Zhu, G.; Tanaka, A.; Bellomo, R. Automated electronic monitoring of circuit pressures during continuous renal replacement therapy: A technical report. Crit. Care Resusc. 2015, 17, 51–54.
- Chen, H.; Ma, Y.; Hong, N.; Wang, H.; Su, L.; Liu, C.; He, J.; Jiang, H.; Long, Y.; Zhu, W. Early warning of citric acid overdose and timely adjustment of regional citrate anticoagulation based on machine learning methods. BMC Med. Inform. Decis. Mak. 2021, 21, 1–11.
- Zhang, W.; Bai, M.; Zhang, L.; Yu, Y.; Li, Y.; Zhao, L.; Yue, Y.; Li, Y.; Zhang, M.; Fu, P. Development and external validation of a model for predicting sufficient filter lifespan in anticoagulation-free continuous renal replacement therapy patients. Blood Purif. 2022, 51, 668–678.
- Avati, A.; Jung, K.; Harman, S.; Downing, L.; Ng, A.; Shah, N.H. Improving palliative care with deep learning. BMC Med. Inform. Decis. Mak. 2018, 18, 122.
- Chua, I.S.; Ritchie, C.S.; Bates, D.W. Enhancing serious illness communication using artificial intelligence. NPJ Digit. Med. 2022, 5, 14.
- Lee, N.S.; Luong, T.; Rosin, R.; Asch, D.A.; Sevinc, C.; Balachandran, M.; Josephs, M.; Rusk, M.H.; McHenry, N.L.; Asch, E.L.; et al. Developing a Chatbot–Clinician Model for Hypertension Management. NEJM Catal. 2022, 3, CAT.22.0228.
- Linder, C. The Effects of a Healthcare Chatbots’ Language and Persona on User Trust, Satisfaction, and Chatbot Effectiveness. Master’s Thesis, Clemson University, Clemson, SC, USA, 2020.
- Bibault, J.E.; Chaix, B.; Guillemassé, A.; Cousin, S.; Escande, A.; Perrin, M.; Pienkowski, A.; Delamon, G.; Nectoux, P.; Brouard, B. A Chatbot Versus Physicians to Provide Information for Patients With Breast Cancer: Blind, Randomized Controlled Noninferiority Trial. J. Med. Internet Res. 2019, 21, e15787.
- Milne-Ives, M.; de Cock, C.; Lim, E.; Shehadeh, M.H.; de Pennington, N.; Mole, G.; Normando, E.; Meinert, E. The Effectiveness of Artificial Intelligence Conversational Agents in Health Care: Systematic Review. J. Med. Internet Res. 2020, 22, e20346.
- Cox, C.E.; Jones, D.M.; Reagan, W.; Key, M.D.; Chow, V.; McFarlin, J.; Casarett, D.; Creutzfeldt, C.J.; Docherty, S.L. Palliative Care Planner: A Pilot Study to Evaluate Acceptability and Usability of an Electronic Health Records System-integrated, Needs-targeted App Platform. Ann. Am. Thorac. Soc. 2018, 15, 59–68.
- Vu, E.; Steinmann, N.; Schröder, C.; Förster, R.; Aebersold, D.M.; Eychmüller, S.; Cihoric, N.; Hertler, C.; Windisch, P.; Zwahlen, D.R. Applications of Machine Learning in Palliative Care: A Systematic Review. Cancers 2023, 15, 1596.
- Yang, M.; Tu, W.; Qu, Q.; Zhao, Z.; Chen, X.; Zhu, J. Personalized response generation by dual-learning based domain adaptation. Neural Netw. 2018, 103, 72–82.
- Murphree, D.H.; Wilson, P.M.; Asai, S.W.; Quest, D.J.; Lin, Y.; Mukherjee, P.; Chhugani, N.; Strand, J.J.; Demuth, G.; Mead, D.; et al. Improving the delivery of palliative care through predictive modeling and healthcare informatics. J. Am. Med. Inform. Assoc. 2021, 28, 1065–1073.
- Radionova, N.; Becker, G.; Mayer-Steinacker, R.; Gencer, D.; Rieger, M.A.; Preiser, C. The views of physicians and nurses on the potentials of an electronic assessment system for recognizing the needs of patients in palliative care. BMC Palliat. Care 2020, 19, 45.
- Zhang, H.; Li, Y.; McConnell, W. Predicting potential palliative care beneficiaries for health plans: A generalized machine learning pipeline. J. Biomed. Inform. 2021, 123, 103922.
- Muscat, D.M.; Lambert, K.; Shepherd, H.; McCaffery, K.J.; Zwi, S.; Liu, N.; Sud, K.; Saunders, J.; O’Lone, E.; Kim, J.; et al. Supporting patients to be involved in decisions about their health and care: Development of a best practice health literacy App for Australian adults living with Chronic Kidney Disease. Health Promot. J. Austr. 2021, 32 (Suppl. 1), 115–127.
- Patzer, R.E.; Basu, M.; Larsen, C.P.; Pastan, S.O.; Mohan, S.; Patzer, M.; Konomos, M.; McClellan, W.M.; Lea, J.; Howard, D.; et al. iChoose Kidney: A Clinical Decision Aid for Kidney Transplantation Versus Dialysis Treatment. Transplantation 2016, 100, 630–639.
- De Panfilis, L.; Peruselli, C.; Tanzi, S.; Botrugno, C. AI-based clinical decision-making systems in palliative medicine: Ethical challenges. BMJ Support. Palliat. Care 2023, 13, 183–189.
- Webb, J.J. Proof of Concept: Using ChatGPT to Teach Emergency Physicians How to Break Bad News. Cureus 2023, 15, e38755.
- Ayers, J.W.; Poliak, A.; Dredze, M.; Leas, E.C.; Zhu, Z.; Kelley, J.B.; Faix, D.J.; Goodman, A.M.; Longhurst, C.A.; Hogarth, M.; et al. Comparing Physician and Artificial Intelligence Chatbot Responses to Patient Questions Posted to a Public Social Media Forum. JAMA Intern. Med. 2023, 183, 589–596.
- Xygkou, A.; Siriaraya, P.; Covaci, A.; Prigerson, H.G.; Neimeyer, R.; Ang, C.S.; She, W.-J. The “Conversation” about Loss: Understanding How Chatbot Technology was Used in Supporting People in Grief. In Proceedings of the 2023 CHI Conference on Human Factors in Computing Systems, Hamburg, Germany, 23–29 April 2023; pp. 1–15.
- Lisetti, C.; Amini, R.; Yasavur, U.; Rishe, N. I can help you change! An empathic virtual agent delivers behavior change health interventions. ACM Trans. Manag. Inf. Syst. 2013, 4, 1–28.
- Yang, J.H.; Shin, G. End-of-Life Care Mobile App for Intensive-Care Unit Nurses: A Quasi-Experimental Study. Int. J. Environ. Res. Public Health 2021, 18, 1253.
- Drummond, D. Between competence and warmth: The remaining place of the physician in the era of artificial intelligence. NPJ Digit. Med. 2021, 4, 85.
This entry is offline, you can click here to edit this entry!
