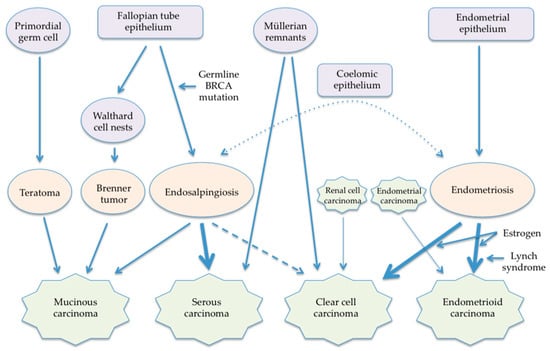
Primary retroperitoneal carcinomas are very rare tumors. Their pathogenesis remains unknown but may be associated with that of ovarian carcinomas, considering the similarity in morphology and gender preference. Mucinous carcinoma, which develops in both women and men, may originate in both primordial germ cells and Walthard cell nests that may be derived from the fallopian tube. Serous carcinomas may be associated with endosalpingiosis and a remnant Müllerian tract. Endometrioid and clear cell carcinomas appear to be associated with extraovarian endometriosis. Additionally, both carcinomas in the retroperitoneal lymph nodes may be metastatic diseases from endometrial and/or renal cell cancers that regress spontaneously (carcinoma of unknown primary).
- retroperitoneal carcinoma
- ovarian carcinoma
- carcinoma of unknown primary
- pathogenesis
1. Introduction
2. Classification of Retroperitoneal Carcinomas
2.1. Histological Subtype
2.2. Site of Disease
3. Previously Postulated Pathogenesis of Retroperitoneal Carcinomas
4. Pathogenesis of Ovarian Carcinomas
Traditionally, all of the four major subtypes of ovarian carcinomas, i.e., serous, endometrioid, clear cell, and mucinous tumors, were thought to derive from the common origin, i.e., ovarian surface epithelium [54][55]. The ovarian surface epithelium, which is derived from the coelomic epithelium, is the pelvic peritoneum that overlies the ovary and lines ovarian epithelial inclusion cysts [56][57]. In contrast to this traditional view, most ovarian carcinomas are now believed to derive from endometrial tissue, fallopian tube tissue, and germ cells [58]. Thus, most ovarian carcinomas are primarily imported from either endometrial or fallopian tube epithelium, unlike other human cancers in which all primary tumors arise de novo [59].
4.1. Mucinous Carcinoma
4.2. Serous Carcinoma
4.3. Endometrioid Carcinoma
4.4. Clear Cell Carcinoma
4.5. Carcinosarcoma
5. Newly Proposed Hypothesis on Pathogenesis of Retroperitoneal Carcinomas
5.1. Mucinous Carcinoma
5.2. Serous Carcinoma
5.3. Endometrioid Carcinoma
5.4. Clear Cell Carcinoma
5.5. Carcinosarcoma
6. Retroperitoneal Carcinoma as a Part of Carcinoma of Unknown Primary
7. Conclusions
This entry is adapted from the peer-reviewed paper 10.3390/cancers15184614
References
- Otsuka, I. Development and rapid growth of retroperitoneal leiomyoma during carboplatin/paclitaxel chemotherapy in an ovarian cancer patient. Eur. J. Obs. Gynecol. Reprod. Biol. 2018, 231, 282–283.
- Neville, A.; Herts, B.R. CT Characteristics of Primary Retroperitoneal Neoplasms. Crit. Rev. Comput. Tomogr. 2004, 45, 247–270.
- Pinson, C.W.; ReMine, S.G.; Fletcher, W.S.; Braasch, J.W. Long-term results with primary retroperitoneal tumors. Arch. Surg. 1989, 124, 1168–1173.
- Crum, C.P. Intercepting pelvic cancer in the distal fallopian tube: Theories and realities. Mol. Oncol. 2009, 3, 165–170.
- Kurman, R.J.; Shih, I.M. The origin and pathogenesis of epithelial ovarian cancer: A proposed unifying theory. Am. J. Surg. Pathol. 2010, 34, 433–443.
- Prat, J. New insights into ovarian cancer pathology. Ann. Oncol. 2012, 23 (Suppl. S10), x111–x117.
- Kuhn, E.; Kurman, R.J.; Shih, I.M. Ovarian cancer is an imported disease: Fact or fiction? Curr. Obs. Gynecol. Rep. 2012, 1, 1–9.
- Myriokefalitaki, E.; Luqman, I.; Potdar, N.; Brown, L.; Steward, W.; Moss, E.L. Primary retroperitoneal mucinous cystadenocarcinoma (PRMCa): A systematic review of the literature and meta-analysis. Arch. Gynecol. Obs. 2016, 293, 709–720.
- Wolf, B.; Kunert, C.; Horn, L.C.; Einenkel, J. Management of Primary Retroperitoneal Mucinous Tumors. A Retrospective Meta-Analysis. Int. J. Gynecol. Cancer 2017, 27, 1064–1071.
- Roma, A.A.; Malpica, A. Primary retroperitoneal mucinous tumors: A clinicopathologic study of 18 cases. Am. J. Surg. Pathol. 2009, 33, 526–533.
- Sonntag, B.; Lelle, R.J.; Steinhard, J.; Brinkmann, O.A.; Hungermann, D.; Kiesel, L. Retroperitoneal mucinous adenocarcinoma occurring during pregnancy in a supernumerary ovary. J. Obs. Gynaecol. 2005, 25, 515–516.
- Kashima, K.; Yahata, T.; Fujita, K.; Tanaka, K. Primary retroperitoneal mucinous cystadenocarcinoma associated with pregnancy. Int. J. Gynecol. Cancer 2008, 18, 908–912.
- Hanhan, H.M.; Gungorduk, K.; Ozdemir, I.A.; Gokcu, M.; Sanci, M.; Ayaz, D.; Ozeren, M. Primary retroperitoneal mucinous cystadenocarcinoma during pregnancy. J. Obs. Gynaecol. 2014, 34, 535–538.
- Ulbright, T.M.; Morley, D.J.; Roth, L.M.; Berkow, R.L. Papillary serous carcinoma of the retroperitoneum. Am. J. Clin. Pathol. 1983, 79, 633–637.
- Caruncho, M.; Pombo, F.; Arnal-Monreal, F. Primary retroperitoneal serous cystadenocarcinoma of ‘ovarian type’: US and CT findings. Eur. J. Radiol. 1993, 17, 115–116.
- Kurosaki, Y.; Kuramoto, K. Case Report: Serous cystadenocarcinoma of the retroperitoneum: CT and sonographic appearance. Clin. Radiol. 1998, 53, 916–918.
- Fujiwara, K.; Oda, T.; Suzuki, S.; Kohno, I.; Hirokawa, M. Primary serous adenocarcinoma of the retroperitoneum with a response of platinum-based chemotherapy: A case report. Int. J. Gynecol. Cancer 1999, 9, 170–172.
- Kaku, M.; Ohara, N.; Seima, Y.; Imanishi, K.; Tomura, N.; Kobayashi, A.; Yamasaki, M.; Hirata, Y.; Murao, S. A primary retroperitoneal serous cystadenocarcinoma with clinically aggressive behavior. Arch. Gynecol. Obs. 2004, 270, 302–306.
- Demir, M.K.; Unlu, E.; Genchellac, H.; Temizoz, O.; Ozdemir, H. Primary serous papillary carcinioma of the retroperitoneum: Magnetic resonance imaging findings with pathologic correlation. Australas. Radiol. 2007, 51, B71–B73.
- Iura, A.; Sasajima, Y.; Katsumata, N.; Kasamatsu, T. Serous adenocarcinoma of the retroperitoneum, as a type of multifocal müllerian carcinoma. Int. J. Clin. Oncol. 2009, 14, 254–257.
- Arichi, N.; Yasumoto, H.; Mitsui, Y.; Hiraoka, T.; Honda, S.; Shiina, H.; Igawa, M. A case of primary retroperitoneal serous adenocarcinoma. Int. J. Urol. 2011, 18, 844–846.
- Zhang, M.M.; Zhao, X.W.; Zhao, J.; Kang, S. A case of primary retroperitoneal serous adenocarcinoma and literature review. Ann. Clin. Case. Rep. 2017, 2, 277.
- Kohada, Y.; Teishima, J.; Hattori, Y.; Kurimura, Y.; Fujii, S.; Sadahide, K.; Fukuoka, K.; Ueno, T.; Kitano, H.; Goto, K.; et al. Serous adenocarcinoma of retroperitoneum: A case report. Int. Cancer Conf. J. 2017, 6, 154.
- Nakatake, R.; Ishizaki, M.; Ishida, M.; Matsui, K.; Kawaguchi, Y.; Kaibori, M. Resection for Primary Retroperitoneal Serous Adenocarcinoma and Liver Metastasis. Intern. Med. 2018, 57, 3371–3375.
- Chae, Y.K.; Saleem, N.; Roh, Y.; Bilal, H.; Viveiros, P.; Sukhadia, B.; Lin, X.; Sheikh, M.M.; Park, L.C. Exceptional response to chemotherapy followed by concurrent radiotherapy and immunotherapy in a male with primary retroperitoneal serous adenocarcinoma: A case report and literature review. BMC Cancer 2019, 19, 748.
- Suda, K.; Nakaoka, H.; Hata, C.; Yahata, N.; Isobe, M.; Kameyama, H.; Wakai, T.; Motoyama, T.; Inoue, I.; Yoshihara, K.; et al. Concurrent isolated retroperitoneal HGSC and STIC defined by somatic mutation analysis: A case report. Diagn. Pathol. 2019, 14, 17.
- Win, T.T.; Aye, S.N.; Abdul Hamad, N.S.; Emilia Tuan Sharif, S. Primary retroperitoneal serous adenocarcinoma: A case report of rare malignancy with literature review. Indian J. Cancer 2021, 58, 262–266.
- Zhou, L.Y.; Zhu, X.D.; Jiang, J.; Bai, Y.F.; Jiang, T.A. Added value of contrast-enhanced ultrasound (CEUS) in the diagnosis of primary retroperitoneal serous adenocarcinoma: A case report. BMC Med. Imaging 2021, 21, 80.
- Otsuka, I.; Honma, K. FDG PET/CT in primary retroperitoneal serous carcinoma. Clin. Nucl. Med. 2023, 48, 625–626.
- Salerno, M.G.; Masciullo, V.; Naldini, A.; Zannoni, G.F.; Vellone, V.; Scambia, G. Endometrioid adenocarcinoma with squamous differentiation arising from ureteral endometriosis in a patient with no history of gonadal endometriosis. Gynecol. Oncol. 2005, 99, 749–752.
- Tanaka, K.; Kobayashi, Y.; Shibuya, H.; Nishigaya, Y.; Momomura, M.; Matsumoto, H.; Iwashita, M. Primary retroperitoneal Müllerian adenocarcinoma arising from endometriosis. J. Obs. Gynaecol. Res. 2014, 40, 1823–1827.
- Osaku, D.; Taniguchi, F.; Moriyama, M.; Sato, S.; Oishi, T.; Harada, T. Retroperitoneal Endometrioid Carcinoma Arising from Ureteral Endometriosis. Case. Rep. Obs. Gynecol. 2019, 2019, 9273858.
- Koual, M.; Benoit, L.; Pacelli, J.; Belda, M.L.; Azaïs, H.; Bats, A.S. Discovery of an endometrioid cancer lymph node metastasis without primary tumor in a context of Lynch syndrome. J. Gynecol. Obs. Hum. Reprod. 2021, 50, 102060.
- Fischerova, D.; Scovazzi, U.; Sousa, N.; Hovhannisyan, T.; Burgetova, A.; Dundr, P.; Nemejcova, K.; Bennett, R.; Vocka, M.; Fruhauf, F.; et al. Primary retroperitoneal nodal endometrioid carcinoma associated with Lynch syndrome: A case report. Front. Oncol. 2023, 13, 1092044.
- Brooks, J.J.; Wheeler, J.E. Malignancy arising in extragonadal endometriosis. A case report and summary of the world literature. Cancer 1977, 40, 3065–3073.
- Maruschke, M.; Anastasiadis, A.G.; Hakenberg, O.W. Spontaneous Regression of Renal Cell Carcinoma: Reality or Myth? World J. Clin. Urol. 2014, 3, 201–208.
- Vatansever, D.; Misirlioglu, S.; Arslan, T.; Zeren, E.H.; Celik, C.; Bolukbasi, Y.; Kaban, K.; Taskiran, C. Primary Retroperitoneal Müllerian Adenocarcinoma: Report of Two Cases Treated with Radical Surgery. J. Obs. Gynaecol. Can. 2021, 43, 242–246.
- Zeng, D.B.; Chang, C.; Liu, X.S.; Gao, Y.; Wang, Y.L.; Pei, Z.J. Magnetic resonance imaging and 18F-fludeoxyglucose positron emission tomography/computed tomography findings of retroperitoneal clear cell carcinoma with an unknown primary site: A case report. Front. Med. 2022, 9, 1024008.
- Ferrie, R.K.; Ross, R.C. Retroperitoneal Müllerian carcinosarcoma. Can. Med. Assoc. J. 1967, 97, 1290–1292.
- Herman, C.W.; Tessler, A.N. Extragenital mixed heterologous tumor of Müllerian type arising in retroperitoneum. Urology 1983, 22, 49–50.
- Booth, C.; Zahn, C.; McBroom, J.; Maxwell, G.L. Retroperitoneal Müllerian carcinosarcoma associated with endometriosis: A case report. Gynecol. Oncol. 2004, 93, 546–549.
- Marquez, R.T.; Baggerly, K.A.; Patterson, A.P.; Liu, J.; Broaddus, R.; Frumovitz, M.; Atkinson, E.N.; Smith, D.I.; Hartmann, L.; Fishman, D.; et al. Patterns of gene expression in different histotypes of epithelial ovarian cancer correlate with those in normal fallopian tube, endometrium, and colon. Clin. Cancer Res. 2005, 11, 6116–6126.
- Cameron, R.I.; Ashe, P.; O’Rourke, D.M.; Foster, H.; McCluggage, W.G. A Panel of Immunohistochemical Stains Assists in the Distinction Between Ovarian and Renal Clear Cell Carcinoma. Int. J. Gynecol. Pathol. 2003, 22, 272–276.
- Fujii, S.; Konishi, I.; Okamura, H.; Mori, T. Mucinous cystadenocarcinoma of the retroperitoneum. A light and electron microscopic study. Gynecol. Oncol. 1986, 24, 103–112.
- Nelson, H.; Benjamin, B.; Alberty, R. Primary retroperitoneal mucinous cystadenocarcinoma. Cancer 1988, 61, 2117–2121.
- Pearl, M.L.; Valea, F.; Chumas, J.; Chalas, E. Primary retroperitoneal mucinous cystadenocarcinoma of low malignant potential: A case report and literature review. Gynecol. Oncol. 1996, 61, 150–152.
- Kessler, T.M.; Kessler, W.; Neuweiler, J.; Nachbur, B.H. Treatment of a case of primary retroperitoneal mucinous cystadenocarcinoma: Is adjuvant hysterectomy and bilateral salpingo-oophorectomy justified? Am. J. Obs. Gynecol. 2002, 187, 227–232.
- Green, J.M.; Bruner, B.C.; Tang, W.W.; Orihuela, E. Retroperitoneal mucinous cystadenocarcinoma in a man: Case report and review of the literature. Urol. Oncol. 2007, 25, 53–55.
- Auersperg, N. The origin of ovarian carcinomas: A unifying hypothesis. Int. J. Gynecol. Pathol. 2011, 30, 12–21.
- Orvis, G.D.; Behringer, R.R. Cellular mechanisms of Müllerian duct formation in the mouse. Dev. Biol. 2007, 306, 493–504.
- d’A Fearn, C.B. Retroperitoneal pseudomucinous cystadenoma of the ovary. Br. J. Surg. 1969, 56, 153–155.
- Signorile, P.G.; Baldi, F.; Bussani, R.; D’Armiento, M.; De Falco, M.; Baldi, A. Ectopic endometrium in human fetuses is a common event and sustains the theory of müllerianosis in the pathogenesis of endometriosis, a disease that predisposes to cancer. J. Exp. Clin. Cancer Res. 2009, 28, 49.
- Erdemoglu, E.; Ayodgou, T.; Tokyol, C. Primary retroperitoneal mucinous cystadenoma. Acta. Obs. Gynecol. Scand. 2003, 82, 486–487.
- Cheng, W.; Liu, J.; Yoshida, H.; Rosen, D.; Naora, H. Lineage infidelity of epithelial ovarian cancers is controlled by HOX genes that specify regional identity in the reproductive tract. Nat. Med. 2005, 11, 531–537.
- Dubeau, L.; Drapkin, R. Coming into focus: The nonovarian origins of ovarian cancer. Ann. Oncol. 2013, 24 (Suppl. S8), viii28–viii35.
- Auersperg, N.; Woo, M.M.; Gilks, C.B. The origin of ovarian carcinomas: A developmental view. Gynecol. Oncol. 2008, 110, 452–454.
- Salvador, S.; Gilks, B.; Köbel, M.; Huntsman, D.; Rosen, B.; Miller, D. The fallopian tube: Primary site of most pelvic high-grade serous carcinomas. Int. J. Gynecol. Cancer 2009, 19, 58–64.
- Kurman, R.J.; Shih, I.M. The dualistic model of ovarian carcinogenesis: Revisited, revised, and expanded. Am. J. Pathol. 2016, 186, 733–747.
- Shih, I.M.; Wang, Y.; Wang, T.L. The Origin of Ovarian Cancer Species and Precancerous Landscape. Am. J. Pathol. 2021, 191, 26–39.
- Purdie, D.M.; Webb, P.M.; Siskind, V.; Bain, C.J.; Green, A.C. The different etiologies of mucinous and nonmucinous epithelial ovarian cancers. Gynecol. Oncol. 2003, 88, S145–S148.
- Chiaffarino, F.; Parazzini, F.; Bosetti, C.; Franceschi, S.; Talamini, R.; Canzonieri, V.; Montella, M.; Ramazzotti, V.; Franceschi, S.; La Vecchia, C. Risk factors for ovarian cancer histotypes. Eur. J. Cancer 2007, 43, 1208–1213.
- Kurian, A.W.; Balise, R.R.; McGuire, V.; Whittemore, A.S. Histologic types of epithelial ovarian cancer: Have they different risk factors? Gynecol. Oncol. 2005, 96, 520–530.
- Jordan, S.J.; Green, A.C.; Whiteman, D.C.; Webb, P.M.; for the Australian Cancer Study (Ovarian Cancer); the Australian Ovarian Cancer Study Group. Risk factors for benign, borderline and invasive mucinous ovarian tumors: Epidemiological evidence of a neoplastic continuum? Gynecol. Oncol. 2007, 107, 223–230.
- Soegaard, M.; Jensen, A.; Hogdall, E.; Christensen, L.; Hogdall, C.; Blaakaer, J.; Kjaer, S.K. Different risk factor profiles for mucinous and nonmucinous ovarian cancer: Results from the Danish MALOVA study. Cancer Epidemiol. Biomark. Prev. 2007, 16, 1160–1166.
- Puls, L.E.; Powell, D.E.; DePriest, P.D.; Gallion, H.H.; Hunter, J.E.; Kryscio, R.J.; van Nagell, J.R., Jr. Transition from benign to malignant epithelium in mucinous and serous ovarian cystadenocarcinoma. Gynecol. Oncol. 1992, 47, 53–57.
- Cheasley, D. The molecular origin and taxonomy of mucinous ovarian carcinoma. Nat. Commun. 2019, 10, 3935.
- Fathalla, M.F. Incessant ovulation—A factor in ovarian neoplasia? Lancet 1971, 2, 163.
- Vercellini, P.; Crosignani, P.; Somigliana, E.; Vigano, P.; Buggio, L.; Bolis, G.; Fedele, L. The ‘incessant menstruation’ hypothesis: A mechanistic ovarian cancer model with implications for prevention. Hum. Reprod. 2011, 26, 2262–2273.
- Otsuka, I. Mechanisms of high-grade serous carcinogenesis in the fallopian tube and ovary: Current hypotheses, etiologic factors, and molecular alterations. Int. J. Mol. Sci. 2021, 22, 4409.
- Karaman, A.; Azılı, M.N.; Boduroglu, E.C.; Karaman, I.; Erdogan, D.; Cavusoglu, Y.H.; Aslan, M.K.; Cakmak, O. A Huge Ovarian Mucinous Cystadenoma in a 14-Year-Old Premenarchal Girl: Review on Ovarian Mucinous Tumor in Premenarchal Girls. J. Pediatr. Adolesc. Gynecol. 2008, 21, 41–44.
- Modugno, F.; Ness, R.B.; Allen, G.O. Alcohol consumption and the risk of mucinous and nonmucinous epithelial ovarian cancer. Obs. Gynecol. 2003, 102, 1336–1343.
- Newcomb, P.A.; Storer, B.E.; Marcus, P.M. Cancer of the large bowel in women in relation to alcohol consumption: A case-control study in Wisconsin (United States). Cancer Causes Control 1993, 4, 405–411.
- Simons, M.; Simmer, F.; Bulten, J.; Lightenberg, M.J.; Hollema, H.; van Vilet, S.; de Voer, R.M.; Kamping, E.J.; van Essen, D.F.; Ylstra, B.; et al. Two types of primary mucinous ovarian tumors can be distinguished based on their origin. Mod. Pathol. 2020, 33, 722–733.
- Vang, R.; Gown, A.M.; Zhao, C.; Barry, T.S.; Isacson, C.; Richardson, M.S.; Ronnett, B.M. Ovarian Mucinous Tumors Associated With Mature Cystic Teratomas. Morphologic and Immunohistochemical Analysis Identifies a Subset of Potential Teratomatous Origin That Shares Features of Lower Gastrointestinal Tract Mucinous Tumors More Commonly Encountered as Secondary Tumors in the Ovary. Am. J. Surg. Pathol. 2007, 31, 854–869.
- Kerr, S.E.; Flotte, A.B.; McFalls, M.J.; Vrana, J.A.; Halling, K.C.; Bell, D.A. Matching maternal isodisomy in mucinous carcinomas and associated ovarian teratomas provides evidence of germ cell derivation for some mucinous ovarian tumors. Am. J. Surg. Pathol. 2013, 37, 1229–1235.
- Elias, K.M.; Tsantoulis, P.; Tille, J.C.; Vitonis, A.; Doyle, L.A.; Hornick, J.L.; Kaya, G.; Barnes, L.; Cramer, D.W.; Puppa, G.; et al. Primordial germ cells as a potential shared cell of origin for mucinous cystic neoplasms of the pancreas and mucinous ovarian tumors. J. Pathol. 2018, 246, 459–469.
- Lee, Y.; Miron, A.; Drapkin, R.; Nucci, M.R.; Medeiros, F.; Saleemuddin, A.; Garber, J.; Birch, C.; Mou, H.; Gordon, R.W.; et al. A candidate precursor to serous carcinoma that originates in the distal fallopian tube. J. Pathol. 2007, 211, 26–35.
- Crum, C.P.; Drapkin, R.; Kindelberger, D.; Medeiros, F.; Miran, A.; Lee, Y. Lessons from BRCA: The tubal fimbria emerges as an origin for pelvic serous cancer. Clin. Med. Res. 2007, 5, 35–44.
- Otsuka, I.; Kameda, S.; Hoshi, K. Early detection of ovarian and fallopian tube cancer by examination of cytological samples from the endometrial cavity. Br. J. Cancer 2013, 109, 603–609.
- Otsuka, I.; Matsuura, T. Screening and prevention for high-grade serous carcinoma of the ovary based on carcinogenesis—Fallopian tube- and ovarian-derived tumors and incessant retrograde bleeding. Diagnostics 2020, 10, 120.
- Kindelberger, D.W.; Lee, Y.; Miron, A.; Hirsch, M.S.; Feltmate, C.; Medeiros, F.; Callahan, M.J.; Garner, E.O.; Gordon, R.W.; Birch, C.; et al. Intraepithelial carcinoma of the fimbria and pelvic serous carcinoma: Evidence for a causal relationship. Am. J. Surg. Pathol. 2007, 31, 161–169.
- Ducie, J.; Dao, F.; Considine, M.; Olvera, N.; Shaw, P.A.; Kurman, R.J.; Shih, I.M.; Soslow, R.A.; Cope, L.; Levine, D.A. Molecular analysis of high-grade serous ovarian carcinoma with and without associated serous tubal intra-epithelial carcinoma. Nat. Commun. 2017, 8, 990.
- Hao, D.; Li, J.; Jia, S.; Meng, Y.; Zhang, C.; Di, L.-j. Integrated analysis reveals tubal- and ovarian-originated serous ovarian cancer and predicts differential therapeutic responses. Clin. Cancer Res. 2017, 23, 7400–7411.
- Nezhat, F.; Cohen, C.; Rahaman, J.; Gretz, H.; Cole, P.; Kalir, T. Comparative immunohistochemical studies of Bcl-2 and p53 proteins in benign and malignant ovarian endometriotic cysts. Cancer 2002, 94, 2935–2940.
- Dinulescu, D.M.; Ince, T.A.; Quade, B.J.; Shafer, S.A.; Crowley, D.; Jacks, T. Role of K-ras and Pten in the development of mouse models of endometriosis and endometrioid ovarian cancer. Nat. Med. 2005, 11, 63–70.
- Prowse, A.H.; Manek, S.; Varma, R.; Liu, J.; Godwin, A.K.; Maher, E.R.; Tomlinson, I.P.; Kennedy, S.H. Molecular genetic evidence that endometriosis is a precursor of ovarian cancer. Int. J. Cancer 2006, 119, 556–562.
- Zondervan, K.T.; Becker, C.M.; Missmer, S.A. Endometriosis. N. Engl. J. Med. 2020, 382, 1244–1256.
- Yamamoto, S.; Tsuda, H.; Takano, M.; Iwaya, K.; Tamai, S.; Matsubara, O. PIK3CA mutation is an early event in the development of endometriosis-associated ovarian clear cell adenocarcinoma. J. Pathol. 2011, 225, 189–194.
- Worley, M.J.; Welch, W.R.; Berkowitz, R.S.; Ng, S.W. Endometriosis-associated ovarian cancer: A review of pathogenesis. Int. J. Mol. Sci. 2013, 14, 5367–5379.
- He, H.; Zhou, G.X.; Zhou, M.; Chen, L. The Distinction of Clear Cell Carcinoma of the Female Genital Tract, Clear Cell Renal Cell Carcinoma, and Translocation-Associated Renal Cell Carcinoma: An Immunohistochemical Study Using Tissue Microarray. Int. J. Gynecol. Pathol. 2011, 30, 425–430.
- Thompson, L.; Chang, B.; Barsky, S.H. Monoclonal origins of malignant mixed tumors (carcinosarcomas). Evidence for a divergent histogenesis. Am. J. Surg. Pathol. 1996, 20, 277–285.
- McConechy, M.K.; Hoang, L.N.; Chui, M.H.; Senz, J.; Yang, W.; Rozenberg, N.; Mackenzie, R.; McAlpine, J.N.; Huntsman, D.G.; Clarke, B.A.; et al. In-depth molecular profiling of the biphasic components of uterine carcinosarcomas. J. Pathol. Clin. Res. 2015, 1, 173–185.
- Masuda, A.; Takeda, A.; Fukami, H.; Yamada, C.; Matsuyama, M. Characteristics of cell lines established from a mixed mesodermal tumor of the ovary. Carcinomatous cells are chnageable to sarcomatous cells. Cancer 1987, 60, 2696–2703.
- Costa, M.J.; Walls, J. Epidermal growth factor receptor and c-erbB-2 oncoprotein expression in female genital tract carcinosarcoma (malignant mixed Müllerian tumors). Clinicopathologic study of 82 cases. Cancer 1996, 77, 533–542.
- Zhao, S.; Bellone, S.; Lopez, S.; Thakral, D.; Schwab, C.; English, D.P.; Black, J.; Cocco, E.; Choi, J.; Zammataro, L.; et al. Mutational landscape of uterine and ovarian carcinosarcomas implicates histone genes in epithelial–mesenchymal transition. Proc. Natl. Acad. Sci. USA 2016, 113, 12238–12243.
- Cherniack, A.D.; Shen, H.; Walter, V.; Stewart, C.; Murray, B.A.; Bowlby, R.; Hu, X.; Ling, S.; Soslow, R.A.; Broaddus, R.R.; et al. Integrated molecular characterization of uterine carcinosarcoma. Cancer Cell 2017, 31, 411–423.
- Tenti, P.; Romagnoli, S.; Pellegata, N.S.; Zappatore, R.; Giunta, P.; Ranzani, G.N.; Carnevali, L. Primay retroperitoneal mucinous cystadenocarcinomas: An immunohistochemical and molecular study. Virchows Arch. 1994, 424, 53–57.
- Song, E.S.; Choi, S.J.; Kim, L.; Choi, S.K.; Ryu, J.S.; Lim, M.K.; Song, Y.S.; Im, M.W. Mucinous adenocarcinoma arising from one retroperitoneal mature cystic teratoma in a postmenopausal woman. J. Obs. Gynaecol. Res. 2005, 31, 127–132.
- Kim, J.H.; Lee, T.S.; Oh, H.K.; Choi, Y.S. A case of mucinous adenocarcinoma arising from retroperitoneal teratoma treated with chemoradiation. J. Gynecol. Oncol. 2009, 20, 126–128.
- Prentice, L.; Stewart, A.; Mohiuddin, S.; Johnson, N.P. What is endosalpingiosis? Fertil. Steril. 2012, 98, 942–947.
- Sunde, J.; Wasickanin, M.; Katz, T.A.; Wickersham, E.L.; Steed, E.; Simper, N. Prevalence of endosalpingiosis and other benign gynecologic lesions. PLoS ONE 2020, 15, e232487.
- Hesseling, M.; De Wilde, R. Endosalpingiosis in laparoscopy. J. Am. Assoc. Gynecol. Laparosc. 2000, 7, 215–218.
- Wang, Y.; Sessine, M.S.; Zhai, Y.; Tipton, C.; McCool, K.; Kuick, R.; Connolly, D.C.; Fearon, E.R.; Cho, K.R. Lineage tracing suggests that ovarian endosalpingiosis does not result from escape of oviductal epithelium. J. Pathol. 2019, 249, 206–214.
- Gallan, A.J.; Antic, T. Benign Müllerian glandular inclusions in men undergoing pelvic lymph node dissection. Hum. Pathol. 2016, 57, 136–139.
- Djordjevic, B.; Clement-Kruzel, S.; Atkinson, N.E.; Malpica, A. Nodal Endosalpingiosis in Ovarian Serous Tumors of Low Malignant Potential With Lymph Node Involvement: A Case for a Precursor Lesion. Am. J. Surg. Pathol. 2010, 34, 1442–1448.
- Gruessner, C.; Gruessner, A.; Glaser, K.; AbuShahin, N.; Laughren, C.; Zheng, W.; Chambers, S.K. Biomarkers and endosalpingiosis in the ovarian and tubal microenvironment of women at high-risk for pelvic serous carcinoma. Am. J. Cancer Res. 2014, 4, 61–72.
- Chui, M.H.; Shih, I.M. Oncogenic BRAF and KRAS mutations in endosalpingiosis. J. Pathol. 2020, 250, 148–158.
- Esselen, K.M.; Terry, K.; Samuel, A.; Elias, K.M.; Davis, M.; Welch, W.R.; Muto, M.G.; Ng, S.W.; Berkowitz, R.S. Endosalpingiosis: More than just an incidental finding at the time of gynecologic surgery? Gynecol. Oncol. 2016, 142, 255–260.
- Dehari, R.; Kurman, R.J.; Loghani, S.; Shih, I.M. The development of high-grade serous carcinoma from atypical proliferative (borderline) serous tumors and low-grade micropapillary serous carcinoma: A morphologic and molecular genetic analysis. Am. J. Surg. Pathol. 2007, 31, 1007–1012.
- Quddus, M.R.; Rashid, L.B.; Hansen, K.; Sung, C.J.; Lawrence, W.D. High-grade serous carcinoma arising in a low-grade serous carcinoma and micropapillary serous borderline tumour of the ovary in a 23-year-old woman. Histopathology 2009, 54, 771–773.
- Boyd, C.; McCluggage, W.G. Low-Grade Ovarian Serous Neoplasms (Low-Grade Serous Carcinoma and Serous Borderline Tumor) Associated With High-Grade Serous Carcinoma or Undifferentiated Carcinoma: Report of a Series of Cases of an Unusual Phenomenon. Am. J. Surg. Pathol. 2012, 36, 368–375.
- Shah, I.A.; Jayram, L.; Gani, O.S.; Fox, I.S.; Stanley, T.M. Papillary serous carcinoma of the peritoneum in a man. Cancer 1998, 82, 860–866.
- Young, R.H.; Scully, R.E. Testicular and paratesticular tumors and tumor-like lesions of ovarian common epithelial and müllerian-types. A report of four cases and review of the literature. Am. J. Clin. Pathol. 1986, 86, 146–152.
- González, R.S.; Vnencak-Jones, C.L.; Shi, C.; Fadare, O. Endomyometriosis (“Uterus-like mass”) in an XY Male: Case Report With Molecular Confirmation and Literature Review. Int. J. Surg. Pathol. 2014, 22, 421–426.
- Heaps, J.M.; Nieberg, R.K.; Berek, J.S. Malignant neoplasm arising in endometriosis. Obstet. Gynecol. 1990, 75, 1023–1028.
- Jerman, L.F.; Hey-Cunningham, A.J. The role of the lymphatic system in endometriosis: A comprehensive review of the literature. Biol. Reprod. 2015, 92, 64.
- Tempfer, C.; Wenzl, R.; Horvat, R.; Grimm, C.; Polterauer, S.; Buekle, B.; Reinthaller, A.; Huber, J. Lymphatic spread of endometriosis to pelvic sentinel lymph nodes: A prospective clinical study. Fertil. Steril. 2011, 96, 692–696.
- Helder-Woolderink, J.M.; Blok, E.A.; Vasen, H.F.; Hollema, H.; Mourits, M.J.; De Bock, G.H. Ovarian cancer in Lynch syndrome; a systematic review. Eur. J. Cancer 2016, 55, 65–73.
- Zanetta, G.M.; Webb, M.J.; Li, H.; Keeney, G.L. Hyperestrogenism: A Relevant Risk Factor for the Development of Cancer from Endometriosis. Gynecol. Oncol. 2000, 79, 18–22.
- Boussios, S.; Karathanasi, A.; Zakynthinakis-Kyriakou, N.; Tsiouris, A.K.; Chatziantoniou, A.A.; Kanellos, F.S.; Tatsi, K. Ovarian carcinosarcoma: Current developments and future perspectives. Crit. Rev. Oncol. Hematol. 2019, 134, 46–55.
- Fizazi, K.; Greco, F.A.; Pavlidis, N.; Daugaard, G.; Oien, K.; Pentheroudakis, G.; on behalf of the ESMO Guidelines Committee. Cancers of unknown primary site: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2015, 26, v133–v138.
- Olivier, T.; Fernandez, E.; Labidi-Galy, I.; Dietrich, P.Y.; Rodriguez-Bravo, V.; Baciarello, G.; Fizazi, K.; Patrikidou, A. Redefining cancer of unknown primary: Is precision medicine really shifting the paradigm? Cancer Treat Rev. 2021, 97, 102204.
- Rassy, E.; Parent, P.; Lefort, F.; Boussios, S.; Baciarello, G.; Pavlidis, N. New rising entities in cancer of unknown primary: Is there a real therapeutic benefit? Crit. Rev. Oncol. Hematol. 2020, 147, 102882.
- Dam, K.; Peeters, F.; Verhoeven, D.; Duwel, V. High-grade serous cancer of undetermined primary origin presenting as solitary inguinal lymph node enlargement. BMJ Case Rep. 2021, 14, e239185.
- Restaino, S.; Mauro, J.; Zermano, S.; Pellecchia, G.; Mariuzzi, L.; Orsaria, M.; Titone, F.; Biasioli, A.; Martina, M.D.; Andreetta, C.; et al. CUP-syndrome: Inguinal high grade serous ovarian carcinoma lymph node metastases with unknown primary origin—A case report and literature review. Front. Oncol. 2022, 12, 987169.
- Slomovitz, B.M.; Soslow, R.A.; Chang, R.C.; Golub, R.; Kuo, D.Y.S. Serous adenocarcinoma of the inguinal region arising from endometriosis followed by a successful pregnancy. Gynecol. Oncol. 2002, 87, 152–154.
- Dubeau, L. The cell of origin of ovarian epithelial tumours. Lancet Oncol. 2008, 9, 1191–1197.
- Lauchlan, S.C. The secondary Müllerian system. Obs. Gynecol. Surv. 1972, 27, 133–146.
- Dubeau, L. The cell of origin of ovarian epithelial tumors and the ovarian surface epithelium dogma: Does the emperor have no clothes? Gynecol. Oncol. 1999, 72, 437–442.
- Fujii, S. Secondary Müllerian system and endometriosis. Am. J. Obs. Gynecol. 1991, 165, 219–225.
- Lauchlan, S.C. The secondary Müllerian system revisited. Int. J. Gynecol. Pathol. 1994, 13, 73–79.
- Lewis, G.K.; Ghaith, S.; Craver, E.C.; Li, Z.; Wasson, M.N.; Burnett, T.L.; Carrubba, A.R. The association of endosalpingiosis with gynecologic malignancy. Gynecol. Oncol. 2022, 167, 81–88.
- Suda, K.; Nakaoka, H.; Yoshihara, K.; Ishiguro, T.; Tamura, R.; Mori, Y.; Yamawaki, K.; Adachi, S.; Takahashi, T.; Kase, H.; et al. Clonal Expansion and Diversification of Cancer-Associated Mutations in Endometriosis and Normal Endometrium. Cell Rep. 2018, 24, 1777.
- Hermens, M.; van Altena, A.M.; Bulten, J.; Siebers, A.G.; Bekkers, R.L.M. Increased association of ovarian cancer in women with histological proven endosalpingiosis. Cancer Epidemiol. 2020, 65, 101700.
- Koninckx, P.R.; Ussia, A.; Adamyan, L.; Wattiez, A.; Gomel, V.; Martin, D.C. Pathogenesis of endometriosis: The genetic/epigenetic theory. Fertil. Steril. 2019, 111, 327–340.
