Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
End-stage liver disease (ESLD) is associated with significant changes in a patient’s coagulation profile. These changes are unique in that they involve all branches of the coagulation system. The hypercoagulability is associated with significant endothelial dysfunction (ED) due to nitric oxide dysregulation.
- liver cirrhosis
- fibrinolysis
- liver and sepsis
- hemostasis monitoring
1. End-Stage Liver Disease and Venous Thromboembolism
End-stage liver disease (ESLD) can be associated with both severe bleeding and clotting. The majority of coagulation and anticoagulation factors are produced in the liver. Despite a reduction in the production of most of these factors in ESLD and defects in primary, secondary, and tertiary coagulation, the coagulation system is most often stable. Some of the coagulation factors produced are extrahepatic and this is one of the main reasons hepatic failure is not necessarily associated only with spontaneous unprovoked bleeding, but with clotting as well [1]. One of the first publications demonstrating that patients with ESLD are not naturally anticoagulated but prone to venous thromboembolism (VTE) was published in 2009 by Northup et al. [2]. The authors found that the incidence of VTE in hospitalized cirrhotic patients was 0.5%. Most of these patients also had a low serum albumin level (most likely a surrogate marker for circulating anticoagulants). In an evaluation (2009) based on the Danish National Register, Søgaard et al. demonstrated that both patients with cirrhosis and not-cirrhotic chronic liver disease had a high risk of developing VTE (relative risk for thromboses 2.06 and 2.10, respectively) in comparison to matched controls from the general population [3]. An association between chronic liver disease and VTE was later confirmed in several publications with an incidence of between 0.5% and 8% [4][5][6][7]. This wide range likely reflects the variability in published studies related to the population studied, particularly as it relates to severity and etiology of liver disease and the diagnostic criteria used. If patients with ESLD require LT, the concern for perioperative thrombotic or bleeding complications is even higher. In fact, different types of thromboses have been described during each stage of transplant surgery.
2. Types and Prevalence of Perioperative Thromboembolic Events
Portal vein thromboses (PVT) are more frequently seen preoperatively with a prevalence of between 1% and 16%, occurring more frequently in patients with decompensated disease [8][9]. An association between preoperative PVT and increased postoperative mortality has been demonstrated [10][11][12]. Like VTE, significant variability in the prevalence of PVT is most likely related to differences in the study populations and design. The vast majority of published studies are single-center and retrospective.
Intraoperative thrombotic complications with clinical presentation occur with a frequency of 1–6% [13][14]. However, transesophageal echocardiography is routinely used during surgery, and a variety of clots have been seen in almost half of all cases, with the majority not needing any treatment [15]. Symptomatic clots, in the form of pulmonary emboli (PE) or intracardiac thromboses, can occur at each stage of LT surgery, but are most frequently described at the time of graft reperfusion and are associated with significant hemodynamic instability and a high mortality rate [16].
Different types of thrombotic complications occur postoperatively. It has been demonstrated that preoperative PVT is associated with postoperative thrombotic complications [10][17][18]. Postoperative thromboses can manifest in the form of PVT (2%) [17], hepatic artery thromboses (HAT) (3–6% and over 8% in children) [19][20], and VTE (5–10%) [21]. Many of these complications are associated with increased mortality. The incidence of PE after LT is about 4% [16] with an associated one-year mortality rate as high as 12% [22]. Early (within 90 days after LT) HAT is associated with graft failure and requires re-transplantation with a rate above 50% for adults and above 60% in children [17][19]. The development of postoperative thromboses (especially HAT) is significantly affected by surgical technique and perioperative management.
3. Causes of Thromboembolism in Cirrhosis
Although the cause of hypercoagulability in ESLD is multifactorial, endothelial dysfunction (ED) is most likely the main driving mechanism of clotting in cirrhotic patients. The pressure gradient between the systemic and portal circulation results in increasing intravascular shear forces resulting in activation of nitric oxide (NO) production and the development of ED [23]. Increased NO levels lead to significant vasodilation, primarily in the portal circulation, resulting in a “steal effect” in the systemic circulation. Low systemic pressure is responsible for a dramatic decrease in perfusion of the intestines, which is associated with increased mucosal permeability, release of endotoxins, and secondary activation of the NO pathway, resulting in an even higher degree of systemic hypotension and ED [24]. Other factors contributing to the development of ED in cirrhotic patients are increased inflammatory and oxidative stress [25]. Endotoxemia itself is associated with increased thrombin generation [26], which is one of the major factors in hypercoagulability. ED in patients with ESLD is also associated with resistance to thrombomodulin (TM), a membrane protein expressed on the surface of endothelial cells, that serves as a co-factor for protein C activation with subsequent impairment of the anticoagulation pathway and increase in thrombin generation [27][28]. Additionally, both the hepatic production of proteins C and S, and antithrombin III (ATIII), and their activity are significantly reduced in ESLD [29]. Another ED-related factor contributing to hypercoagulability in cirrhosis is the significantly increased production of endothelium liver-independent coagulation or anticoagulation factors such as Factor (F) FVIII, von Willebrand factor (vWF), and plasminogen activator inhibitor 1 (PAI-1) [30][31][32]. vWF is likely one of the key components of hypercoagulability in cirrhosis. Despite thrombocytopenia and impaired platelet function in vitro [33], platelet function in vivo is likely normal or even increased due to a high concentration of vWF. This is not just because of increased production but also because of decreased destruction by cleaving protease ADAMTS13 synthetized in the liver [29][34].
FVIII is one of the targets of activated protein C. In ESLD, the ratio between FVIII and activated protein C (which indicates the severity of cirrhosis) can reach 5.0. This imbalance is an additional factor responsible for the impairment of thrombin generation inhibition [35][36].
In addition to primary and secondary coagulation, tertiary coagulation is significantly affected in cirrhosis. An increase in PAI-1 levels in combination with reduced levels of tissue plasminogen activator is responsible for decreased fibrinolysis in patients with ESLD [37][38]. It has been also shown that patients with ESLD have increased clot stability due to diminished permeability and reduced lysis [39][40] (Figure 1).
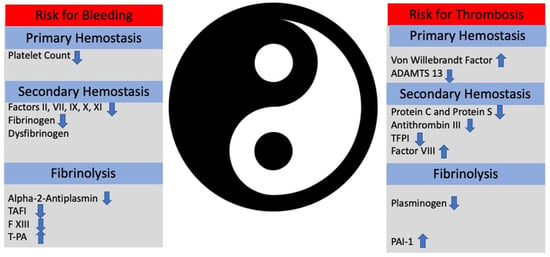
Figure 1. The Ying (bleeding) and the Yang (thrombosis) of hemostasis in patients with end-stage liver disease. Instable balance between thrombosis and bleeding illustrates the critical balance between pro- and anticoagulants. Depending on clinical scenario, patients can bleed or develop thrombosis. TAFI: tissue activable factor inhibitor. t-PA: tissue plasmin activator. PAI-1: plasminogen-activator inhibitor-1.
4. Subpopulations Susceptible to Thromboembolism
There are number of subpopulations of patients with ESLD predisposed to developing thromboses. It has been demonstrated that patients with nonalcoholic steatohepatitis (NASH) have an increased prevalence of deep vein thrombosis, PE, and PVT [41][42][43]. The reason for this is inflammation and increased oxidative stress that occurs with NASH at a higher degree than in patients with other types of ESLD [37][44]. Other subpopulations prone to thrombotic complications include patients with autoimmune conditions (due to chronic inflammation, cytokine release, and high fibrinogen concentration) [45][46] and patients with hepatitis C (due to chronic inflammation and production of autoantibodies such anticardiolipins and increased thrombin generation) [47][48].
Several genetic mutations associated with thromboses (mostly VTE and PVT) are frequently seen in patients with ESLD. These include FV Leiden [49], Prothrombin G20210A mutation (which leads to a high prothrombin level) [50], high plasma homocysteine level [51], a mutation in the methylenetetrahydrofolate reductase gene 51, JAK2V617F mutations [52], and myeloproliferative neoplasms (MPN) [53]. Due to chronic hypercoagulability associated with ESLD, these mutations make patients with cirrhosis more susceptible to thromboses than the general population.
This entry is adapted from the peer-reviewed paper 10.3390/jcm12175759
References
- Tripodi, A.; Salerno, F.; Chantarangkul, V.; Cletrici, M.; Calzzaniga, M.; Primignani, M.; Mannucci, P.M. Evidence of normal thrombin generation in cirrhosis despite abnormal conventional coagulation tests. Hepatology 2005, 41, 553–558.
- Northup, P.G.; McMahon, M.M.; Ruhl, A.P.; Altschuler, S.; Volk-Bednarz, A.; Caldwell, S.H.; Berg, C.L. Coagulopathy does not fully protect hospitalized cirrhosis patients from peripheral venous thromboembolism. Am. J. Gastroenterol. 2006, 101, 1524–1528, quiz 1680.
- Sogaard, K.K.; Horvath-Puho, E.; Gronbaek, H.; Jepsen, P.; Vilstrup, H.; Sorensen, H.T. Risk of venous thromboembolism in patients with liver disease: A nationwide population-based case-control study. Am. J. Gastroenterol. 2009, 104, 96–101.
- Sogaard, K.K.; Horvath-Puho, E.; Montomoli, J.; Vilstrup, H.; Sorensen, H.T. Cirrhosis is Associated with an Increased 30-Day Mortality After Venous Thromboembolism. Clin. Transl. Gastroenterol. 2015, 6, e97.
- Wu, H.; Nguyen, G.C. Liver cirrhosis is associated with venous thromboembolism among hospitalized patients in a nationwide US study. Clin. Gastroenterol. Hepatol. 2010, 8, 800–805.
- Dabbagh, O.; Oza, A.; Prakash, S.; Sunna, R.; Saettele, T.M. Coagulopathy does not protect against venous thromboembolism in hospitalized patients with chronic liver disease. Chest 2010, 137, 1145–1149.
- Gulley, D.; Teal, E.; Suvannasankha, A.; Chalasani, N.; Liangpunsakul, S. Deep vein thrombosis and pulmonary embolism in cirrhosis patients. Dig. Dis. Sci. 2008, 53, 3012–3017.
- Mantaka, A.; Augoustaki, A.; Kouroumalis, E.A.; Samonakis, D.N. Portal vein thrombosis in cirrhosis: Diagnosis, natural history, and therapeutic challenges. Ann. Gastroenterol. 2018, 31, 315–329.
- Zhang, Y.; Xu, B.Y.; Wang, X.B.; Zheng, X.; Huang, Y.; Chen, J.; Meng, Z.-J.; Gao, Y.-H.; Qian, Z.-P.; Liu, F.; et al. Prevalence and Clinical Significance of Portal Vein Thrombosis in Patients With Cirrhosis and Acute Decompensation. Clin. Gastroenterol. Hepatol. 2020, 18, 2564–2572.e1.
- Stine, J.G.; Pelletier, S.J.; Schmitt, T.M.; Porte, R.J.; Northup, P.G. Pre-transplant portal vein thrombosis is an independent risk factor for graft loss due to hepatic artery thrombosis in liver transplant recipients. HPB 2016, 18, 279–286.
- Stine, J.G.; Shah, P.M.; Cornella, S.L.; Rudnick, S.R.; Ghabril, M.S.; Stukenborg, G.J.; Northup, P.G. Portal vein thrombosis, mortality and hepatic decompensation in patients with cirrhosis: A meta-analysis. World J. Hepatol. 2015, 7, 2774–2780.
- Chardot, C.; Herrera, J.M.; Debray, D. Portal vein complications after liver transplantation for biliary atresia. Liver Transplant. Surg. 1997, 3, 351–358.
- Gologorsky, E.; De Wolf, A.M.; Scott, V.; Aggarwal, S.; Dishart, M.; Kang, Y. Intracardiac thrombus formation and pulmonary thromboembolism immediately after graft reperfusion in 7 patients undergoing liver transplantation. Liver Transpl. 2001, 7, 783–789.
- Lerner, A.B.; Sundar, E.; Mahmood, F.; Sarge, T.; Hanto, D.W.; Panzica, P.J. Four cases of cardiopulmonary thromboembolism during liver transplantation without the use of antifibrinolytic drugs. Anesth. Analg. 2005, 101, 1608–1612.
- Shillcutt, S.K.; Ringenberg, K.J.; Chacon, M.M.; Brakke, T.R.; Montzingo, C.R.; Lyden, E.R.; Schulte, T.E.; Porter, T.R.; Lisco, S.J. Liver Transplantation: Intraoperative Transesophageal Echocardiography Findings and Relationship to Major Postoperative Adverse Cardiac Events. J. Cardiothorac. Vasc. Anesth. 2016, 30, 107–114.
- Sakai, T.; Matsusaki, T.; Dai, F.; Tanaka, K.A.; Donaldson, J.B.; Hilmi, I.A.; Marsh, J.W.; Planinsic, R.M.; Humar, A. Pulmonary thromboembolism during adult liver transplantation: Incidence, clinical presentation, outcome, risk factors, and diagnostic predictors. Br. J. Anaesth. 2012, 108, 469–477.
- Duffy, J.P.; Hong, J.C.; Farmer, D.G.; Ghobrial, R.M.; Yersiz, H.; Hiatt, J.R.; Busuttil, R.W. Vascular complications of orthotopic liver transplantation: Experience in more than 4200 patients. J. Am. Coll. Surg. 2009, 208, 896–903, discussion 903–895.
- Bezinover, D.; Iskandarani, K.; Chinchilli, V.; McQuillan, P.; Saner, F.; Kadry, Z.; Riley, T.R.; Janicki, P.K. Autoimmune conditions are associated with perioperative thrombotic complications in liver transplant recipients: A UNOS database analysis. BMC Anesthesiol. 2016, 16, 26.
- Bekker, J.; Ploem, S.; de Jong, K.P. Early hepatic artery thrombosis after liver transplantation: A systematic review of the incidence, outcome and risk factors. Am. J. Transplant. 2009, 9, 746–757.
- Iida, T.; Kaido, T.; Yagi, S.; Hori, T.; Uchida, Y.; Jobara, K.; Tanaka, H.; Sakamoto, S.; Kasahara, M.; Ogawa, K.; et al. Hepatic arterial complications in adult living donor liver transplant recipients: A single-center experience of 673 cases. Clin. Transplant. 2014, 28, 1025–1030.
- Salami, A.; Qureshi, W.; Kuriakose, P.; Moonka, D.; Yoshida, A.; Abouljoud, M. Frequency and predictors of venous thromboembolism in orthotopic liver transplant recipients: A single-center retrospective review. Transplant. Proc. 2013, 45, 315–319.
- Naess, I.A.; Christiansen, S.C.; Romundstad, P.; Cannegieter, S.C.; Rosendaal, F.R.; Hammerstrom, J. Incidence and mortality of venous thrombosis: A population-based study. J. Thromb. Haemost. 2007, 5, 692–699.
- Mookerjee, R.P.; Vairappan, B.; Jalan, R. The puzzle of endothelial nitric oxide synthase dysfunction in portal hypertension: The missing piece? Hepatology 2007, 46, 943–946.
- Harrison, P.; Wendon, J.; Williams, R. Evidence of increased guanylate cyclase activation by acetylcysteine in fulminant hepatic failure. Hepatology 1996, 23, 1067–1072.
- Clapp, B.R.; Hingorani, A.D.; Kharbanda, R.K.; Mohamedali, V.; Stephens, J.W.; Vallance, P.; MacAllister, R.J. Inflammation-induced endothelial dysfunction involves reduced nitric oxide bioavailability and increased oxidant stress. Cardiovasc. Res. 2004, 64, 172–178.
- Violi, F.; Ferro, D.; Basili, S.; Lionetti, R.; Rossi, E.; Merli, M.; Riggio, O.; Bezzi, M.; Capocaccia, L. Ongoing prothrombotic state in the portal circulation of cirrhotic patients. Thromb. Haemost. 1997, 77, 44–47.
- Tripodi, A. Hemostasis in Acute and Chronic Liver Disease. Semin. Liver Dis. 2017, 37, 28–32.
- Tripodi, A.; Anstee, Q.M.; Sogaard, K.K.; Primignani, M.; Valla, D.C. Hypercoagulability in cirrhosis: Causes and consequences. J. Thromb. Haemost. 2011, 9, 1713–1723.
- Raparelli, V.; Basili, S.; Carnevale, R.; Napoleone, L.; Del Ben, M.; Nocella, C.; Bartimoccia, S.; Lucidi, C.; Talerico, G.; Riggio, O.; et al. Low-grade endotoxemia and platelet activation in cirrhosis. Hepatology 2017, 65, 571–581.
- Saner, F.H.; Gieseler, R.K.; Akiz, H.; Canbay, A.; Gorlinger, K. Delicate balance of bleeding and thrombosis in end-stage liver disease and liver transplantation. Digestion 2013, 88, 135–144.
- Hollestelle, M.J.; Geertzen, H.G.; Straatsburg, I.H.; van Gulik, T.M.; van Mourik, J.A. Factor VIII expression in liver disease. Thromb. Haemost. 2004, 91, 267–275.
- Tripodi, A.; Mannucci, P.M. The coagulopathy of chronic liver disease. N. Engl. J. Med. 2011, 365, 147–156.
- Laffi, G.; Cominelli, F.; Ruggiero, M.; Fedi, S.; Chiarugi, V.P.; La Villa, G.; Pinzani, M.; Gentilini, P. Altered platelet function in cirrhosis of the liver: Impairment of inositol lipid and arachidonic acid metabolism in response to agonists. Hepatology 1988, 8, 1620–1626.
- Lisman, T.; Bongers, T.N.; Adelmeijer, J.; Janssen, H.L.; de Maat, M.P.; de Groot, P.G.; Leebeek, F.W. Elevated levels of von Willebrand Factor in cirrhosis support platelet adhesion despite reduced functional capacity. Hepatology 2006, 44, 53–61.
- Tripodi, A.; Primignani, M.; Chantarangkul, V.; Dell’Era, A.; Clerici, M.; de Franchis, R.; Colombo, M.; Mannucci, P.M. An imbalance of pro- vs anti-coagulation factors in plasma from patients with cirrhosis. Gastroenterology 2009, 137, 2105–2111.
- Tripodi, A.; Primignani, M.; Lemma, L.; Chantarangkul, V.; Dell’Era, A.; Iannuzzi, F.; Aghemo, A.; Mannucci, P.M. Detection of the imbalance of procoagulant versus anticoagulant factors in cirrhosis by a simple laboratory method. Hepatology 2010, 52, 249–255.
- Kotronen, A.; Joutsi-Korhonen, L.; Sevastianova, K.; Bergholm, R.; Hakkarainen, A.; Pietiläinen, K.H.; Lundbom, N.; Rissanen, A.; Lassila, R.; Yki-Järvinen, H. Increased coagulation factor VIII, IX, XI and XII activities in non-alcoholic fatty liver disease. Liver Int. 2011, 31, 176–183.
- Cigolini, M.; Targher, G.; Agostino, G.; Tonoli, M.; Muggeo, M.; De Sandre, G. Liver steatosis and its relation to plasma haemostatic factors in apparently healthy men—Role of the metabolic syndrome. Thromb. Haemost. 1996, 76, 69–73.
- Hugenholtz, G.C.; Macrae, F.; Adelmeijer, J.; Dulfer, S.; Porte, R.J.; Lisman, T.; Ariëns, R.A.S. Procoagulant changes in fibrin clot structure in patients with cirrhosis are associated with oxidative modifications of fibrinogen. J. Thromb. Haemost. 2016, 14, 1054–1066.
- Undas, A.; Nowakowski, T.; Ciesla-Dul, M.; Sadowski, J. Abnormal plasma fibrin clot characteristics are associated with worse clinical outcome in patients with peripheral arterial disease and thromboangiitis obliterans. Atherosclerosis 2011, 215, 481–486.
- Stine, J.G.; Shah, N.L.; Argo, C.K.; Pelletier, S.J.; Caldwell, S.H.; Northup, P.G. Increased risk of portal vein thrombosis in patients with cirrhosis due to nonalcoholic steatohepatitis. Liver Transpl. 2015, 21, 1016–1021.
- Stine, J.G.; Argo, C.K.; Pelletier, S.J.; Maluf, D.G.; Caldwell, S.H.; Northup, P.G. Advanced non-alcoholic steatohepatitis cirrhosis: A high-risk population for pre-liver transplant portal vein thrombosis. World J. Hepatol. 2017, 9, 139–146.
- Stine, J.G.; Niccum, B.A.; Zimmet, A.N.; Intagliata, N.; Caldwell, S.H.; Argo, C.K.; Northup, P.G. Increased risk of venous thromboembolism in hospitalized patients with cirrhosis due to non-alcoholic steatohepatitis. Clin. Transl. Gastroenterol. 2018, 9, 140.
- Tripodi, A.; Fracanzani, A.L.; Primignani, M.; Chantarangkul, V.; Clerici, M.; Mannucci, P.M.; Peyvandi, F.; Bertelli, C.; Valenti, L.; Fargion, S. Procoagulant imbalance in patients with non-alcoholic fatty liver disease. J. Hepatol. 2014, 61, 148–154.
- Biagini, M.R.; Tozzi, A.; Marcucci, R.; Paniccia, R.; Fedi, S.; Milani, S.; Galli, A.; Ceni, E.; Capanni, M.; Manta, R.; et al. Hyperhomocysteinemia and hypercoagulability in primary biliary cirrhosis. World J. Gastroenterol. 2006, 12, 1607–1612.
- Zoller, B.; Li, X.; Sundquist, J.; Sundquist, K. Autoimmune diseases and venous thromboembolism: A review of the literature. Am. J. Cardiovasc. Dis. 2012, 2, 171–183.
- Prieto, J.; Yuste, J.R.; Beloqui, O.; Civeira, M.P.; Riezu, J.I.; Aguirre, B.; Sangro, B. Anticardiolipin antibodies in chronic hepatitis C: Implication of hepatitis C virus as the cause of the antiphospholipid syndrome. Hepatology 1996, 23, 199–204.
- Violi, F.; Ferro, D.; Basili, S.; Artini, M.; Valesini, G.; Levrero, M.; Cordova, C. Increased rate of thrombin generation in hepatitis C virus cirrhotic patients. Relationship to venous thrombosis. J. Investig. Med. 1995, 43, 550–554.
- Dahlback, B. Advances in understanding pathogenic mechanisms of thrombophilic disorders. Blood 2008, 112, 19–27.
- Walker, A.P. Portal vein thrombosis: What is the role of genetics? Eur. J. Gastroenterol. Hepatol. 2005, 17, 705–707.
- Amitrano, L.; Brancaccio, V.; Guardascione, M.A.; Margaglione, M.; Iannaccone, L.; D’Andrea, G.; Marmo, R.; Ames, P.R.; Balzano, A. Inherited coagulation disorders in cirrhotic patients with portal vein thrombosis. Hepatology 2000, 31, 345–348.
- Qi, X.; Yang, Z.; Bai, M.; Shi, X.; Han, G.; Fan, D. Meta-analysis: The significance of screening for JAK2V617F mutation in Budd-Chiari syndrome and portal venous system thrombosis. Aliment. Pharmacol. Ther. 2011, 33, 1087–1103.
- Qi, X.; Li, H.; Liu, X.; Yao, H.; Han, G.; Hu, F.; Shao, L.; Guo, X. Novel insights into the development of portal vein thrombosis in cirrhosis patients. Expert. Rev. Gastroenterol. Hepatol. 2015, 9, 1421–1432.
This entry is offline, you can click here to edit this entry!
