Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Critical Care Medicine
End-stage liver disease (ESLD) is associated with significant changes in a patient’s coagulation profile. These changes are unique in that they involve all branches of the coagulation system. The hypercoagulability is associated with significant endothelial dysfunction (ED) due to nitric oxide dysregulation.
- liver cirrhosis
- fibrinolysis
- liver and sepsis
- hemostasis monitoring
1. End-Stage Liver Disease and Venous Thromboembolism
End-stage liver disease (ESLD) can be associated with both severe bleeding and clotting. The majority of coagulation and anticoagulation factors are produced in the liver. Despite a reduction in the production of most of these factors in ESLD and defects in primary, secondary, and tertiary coagulation, the coagulation system is most often stable. Some of the coagulation factors produced are extrahepatic and this is one of the main reasons hepatic failure is not necessarily associated only with spontaneous unprovoked bleeding, but with clotting as well [1]. One of the first publications demonstrating that patients with ESLD are not naturally anticoagulated but prone to venous thromboembolism (VTE) was published in 2009 by Northup et al. [2]. The authors found that the incidence of VTE in hospitalized cirrhotic patients was 0.5%. Most of these patients also had a low serum albumin level (most likely a surrogate marker for circulating anticoagulants). In an evaluation (2009) based on the Danish National Register, Søgaard et al. demonstrated that both patients with cirrhosis and not-cirrhotic chronic liver disease had a high risk of developing VTE (relative risk for thromboses 2.06 and 2.10, respectively) in comparison to matched controls from the general population [3]. An association between chronic liver disease and VTE was later confirmed in several publications with an incidence of between 0.5% and 8% [4,5,6,7]. This wide range likely reflects the variability in published studies related to the population studied, particularly as it relates to severity and etiology of liver disease and the diagnostic criteria used. If patients with ESLD require LT, the concern for perioperative thrombotic or bleeding complications is even higher. In fact, different types of thromboses have been described during each stage of transplant surgery.
2. Types and Prevalence of Perioperative Thromboembolic Events
Portal vein thromboses (PVT) are more frequently seen preoperatively with a prevalence of between 1% and 16%, occurring more frequently in patients with decompensated disease [8,9]. An association between preoperative PVT and increased postoperative mortality has been demonstrated [10,11,12]. Like VTE, significant variability in the prevalence of PVT is most likely related to differences in the study populations and design. The vast majority of published studies are single-center and retrospective.
Intraoperative thrombotic complications with clinical presentation occur with a frequency of 1–6% [13,14]. However, transesophageal echocardiography is routinely used during surgery, and a variety of clots have been seen in almost half of all cases, with the majority not needing any treatment [15]. Symptomatic clots, in the form of pulmonary emboli (PE) or intracardiac thromboses, can occur at each stage of LT surgery, but are most frequently described at the time of graft reperfusion and are associated with significant hemodynamic instability and a high mortality rate [16].
Different types of thrombotic complications occur postoperatively. It has been demonstrated that preoperative PVT is associated with postoperative thrombotic complications [10,17,18]. Postoperative thromboses can manifest in the form of PVT (2%) [17], hepatic artery thromboses (HAT) (3–6% and over 8% in children) [19,20], and VTE (5–10%) [21]. Many of these complications are associated with increased mortality. The incidence of PE after LT is about 4% [16] with an associated one-year mortality rate as high as 12% [22]. Early (within 90 days after LT) HAT is associated with graft failure and requires re-transplantation with a rate above 50% for adults and above 60% in children [17,19]. The development of postoperative thromboses (especially HAT) is significantly affected by surgical technique and perioperative management.
3. Causes of Thromboembolism in Cirrhosis
Although the cause of hypercoagulability in ESLD is multifactorial, endothelial dysfunction (ED) is most likely the main driving mechanism of clotting in cirrhotic patients. The pressure gradient between the systemic and portal circulation results in increasing intravascular shear forces resulting in activation of nitric oxide (NO) production and the development of ED [23]. Increased NO levels lead to significant vasodilation, primarily in the portal circulation, resulting in a “steal effect” in the systemic circulation. Low systemic pressure is responsible for a dramatic decrease in perfusion of the intestines, which is associated with increased mucosal permeability, release of endotoxins, and secondary activation of the NO pathway, resulting in an even higher degree of systemic hypotension and ED [24]. Other factors contributing to the development of ED in cirrhotic patients are increased inflammatory and oxidative stress [25]. Endotoxemia itself is associated with increased thrombin generation [26], which is one of the major factors in hypercoagulability. ED in patients with ESLD is also associated with resistance to thrombomodulin (TM), a membrane protein expressed on the surface of endothelial cells, that serves as a co-factor for protein C activation with subsequent impairment of the anticoagulation pathway and increase in thrombin generation [27,28]. Additionally, both the hepatic production of proteins C and S, and antithrombin III (ATIII), and their activity are significantly reduced in ESLD [29]. Another ED-related factor contributing to hypercoagulability in cirrhosis is the significantly increased production of endothelium liver-independent coagulation or anticoagulation factors such as Factor (F) FVIII, von Willebrand factor (vWF), and plasminogen activator inhibitor 1 (PAI-1) [30,31,32]. vWF is likely one of the key components of hypercoagulability in cirrhosis. Despite thrombocytopenia and impaired platelet function in vitro [33], platelet function in vivo is likely normal or even increased due to a high concentration of vWF. This is not just because of increased production but also because of decreased destruction by cleaving protease ADAMTS13 synthetized in the liver [29,34].
FVIII is one of the targets of activated protein C. In ESLD, the ratio between FVIII and activated protein C (which indicates the severity of cirrhosis) can reach 5.0. This imbalance is an additional factor responsible for the impairment of thrombin generation inhibition [35,36].
In addition to primary and secondary coagulation, tertiary coagulation is significantly affected in cirrhosis. An increase in PAI-1 levels in combination with reduced levels of tissue plasminogen activator is responsible for decreased fibrinolysis in patients with ESLD [37,38]. It has been also shown that patients with ESLD have increased clot stability due to diminished permeability and reduced lysis [39,40] (Figure 1).
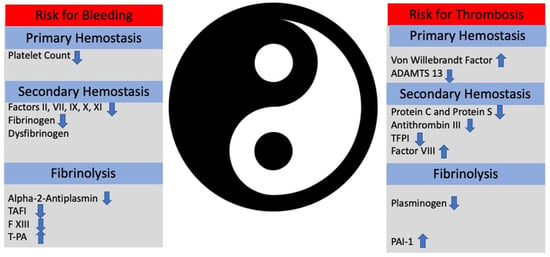
Figure 1. The Ying (bleeding) and the Yang (thrombosis) of hemostasis in patients with end-stage liver disease. Instable balance between thrombosis and bleeding illustrates the critical balance between pro- and anticoagulants. Depending on clinical scenario, patients can bleed or develop thrombosis. TAFI: tissue activable factor inhibitor. t-PA: tissue plasmin activator. PAI-1: plasminogen-activator inhibitor-1.
4. Subpopulations Susceptible to Thromboembolism
There are number of subpopulations of patients with ESLD predisposed to developing thromboses. It has been demonstrated that patients with nonalcoholic steatohepatitis (NASH) have an increased prevalence of deep vein thrombosis, PE, and PVT [41,42,43]. The reason for this is inflammation and increased oxidative stress that occurs with NASH at a higher degree than in patients with other types of ESLD [37,44]. Other subpopulations prone to thrombotic complications include patients with autoimmune conditions (due to chronic inflammation, cytokine release, and high fibrinogen concentration) [45,46] and patients with hepatitis C (due to chronic inflammation and production of autoantibodies such anticardiolipins and increased thrombin generation) [47,48].
Several genetic mutations associated with thromboses (mostly VTE and PVT) are frequently seen in patients with ESLD. These include FV Leiden [49], Prothrombin G20210A mutation (which leads to a high prothrombin level) [50], high plasma homocysteine level [51], a mutation in the methylenetetrahydrofolate reductase gene 51, JAK2V617F mutations [52], and myeloproliferative neoplasms (MPN) [53]. Due to chronic hypercoagulability associated with ESLD, these mutations make patients with cirrhosis more susceptible to thromboses than the general population.
This entry is adapted from the peer-reviewed paper 10.3390/jcm12175759
This entry is offline, you can click here to edit this entry!
