You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Non-alcoholic fatty liver disease (NAFLD) stands as an increasingly pressing global health challenge, underscoring the need for timely identification to facilitate effective treatment and prevent the progression of chronic liver disorders. Given the projected scarcity of specialized healthcare professionals, particularly hepatologists and gastroenterologists, the role of pharmacists emerges as pivotal in NAFLD management.
- NAFLD
- pharmacist
- roles
- hepatology
1. Introduction
Evaluating the health status of potential patients with NAFLD can be challenging for pharmacists, let alone developing a short- and long-term plan for improvement, particularly in outpatient or community pharmacies where pharmacists do not have access to their laboratory results. The simplest approach would be to create a questionnaire that encompasses the major factors previously shown to predict NAFLD. While researchers and physicians may have access to invasive measurements, pharmacists must carefully balance their choices by selecting non-invasive yet essential variables that can predict NAFLD with greater confidence. Given the practical challenges in outpatient or community pharmacies and the limitations pharmacists may face, presented below are some tools that can be utilized by them.
Once patients are suspected of having NAFLD, a report can be generated and sent to their primary care physicians for a detailed check-up. At this point, pharmacists should also take the opportunity to validate and compare their results with the more sophisticated and direct diagnostic methods used in physicians’ offices or hospitals.
2. Common Variables to Identify NAFLD
Numerous variables with proven predictive capabilities for NAFLD have been documented in the existing literature. Nevertheless, it is essential to acknowledge that, within a community pharmacy environment, it may not be feasible to employ all the variables. Consequently, it becomes imperative for pharmacists to discern the pharmacy’s resource limitations and identify suitable variables that can be efficiently and accurately measured.
In addition to the variables listed in Table 1, pharmacists should also aim to collect some of the non-invasive variables like anthropometrics and family history.
Table 1. Known factors and rationale for using them for NAFLD diagnosis.
| Variables | Rationale |
|---|---|
|
|
|
|
|
|
|
|
Anthropometrics and physical examination: In community settings, among the most prevalent and easily obtainable measurements are height, weight, waist, and hip measurements. Height and weight serve as the basis for calculating body mass index (BMI), while waist and hip measurements enable the computation of the waist-hip ratio. Both BMI and waist-hip ratio possess significant predictive value concerning metabolic syndrome, a commonly observed characteristic in NAFLD [1][2][3]. Pharmacists may also consider quantifying body fat percentage over BMI, since it has been shown to predict NAFLD [4]. While dual-energy X-ray absorptiometry is the gold standard, other less expensive tools have been validated to predict body fat percentage [5]. Lastly, while practically and legally not possible for pharmacists in many countries, some countries may allow pharmacists to physically examine patients. However, it is important to note that these examinations require additional resources that pharmacists should consider before offering such services at their pharmacy.
Moreover, when resources and technical expertise are available, indirect tools (e.g., bioelectrical impedance analysis, BIA [6]) can be employed by pharmacists to assess body composition, offering additional insights into an individual’s health status and potential risk factors. The adoption of these measurements and assessments can contribute to a more comprehensive evaluation of patients’ well-being and facilitate the early detection of health concerns related to NAFLD and metabolic syndrome.
Family history: Family history plays a crucial role in predicting susceptibility to non-alcoholic fatty liver disease (NAFLD). Inherited factors passed down through generations significantly influence an individual’s likelihood of developing NAFLD. A positive family history of metabolic disorders, obesity, type 2 diabetes, and dyslipidemia elevates the risk of NAFLD occurrence [7][8]. Accurate identification of familial predisposition enables pharmacists to proactively monitor individuals at higher risk. Therefore, understanding these hereditary factors and by incorporating a family history assessment with other pertinent risk factors and biomarkers, pharmacists can optimize personalized preventive strategies and enhance patient care for NAFLD.
Blood biomarkers: Based on the previous literature, 17 studies involving NAFLD patients were identified and evaluated for blood biomarkers [9][10][11][12][13][14][15][16][17][18][19][20][21][22][23]. A total of 19 blood biomarkers were recognized that were altered in the presence of NAFLD. These biomarkers are listed in Figure 1 in the order of their frequency. For example, alanine transaminase (ALT) was reported to be increased in NAFLD patients in 72% of the studies included in the analysis, whereas only 6% of the studies reported increases in alkaline phosphatase (ALP) and c-peptide. Although limited within the settings of a community pharmacy, these blood biomarkers offer valuable insights into potential NAFLD diagnoses. Pharmacists with access to patients’ medical records or connectivity to pathology labs can utilize this information for informed clinical decision making (i.e., potentially identifying underlying NAFLD).
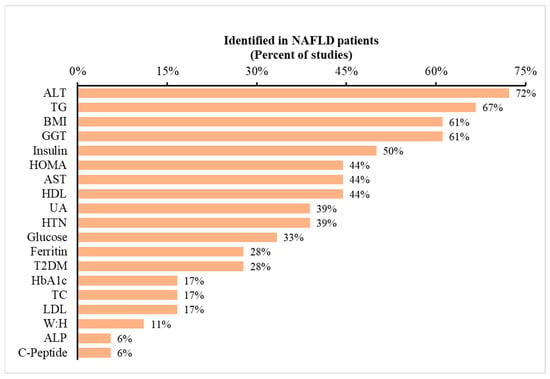
Figure 1. Occurrence of metabolic variables reported in prior studies of NAFLD patients. Legend: The dataset consists of 17 studies. The data depict the percentage of studies reporting specific metabolic variables listed on the x-axis. To illustrate, 72% of previous studies indicated ALT as a metabolic marker for predicting NAFLD. Abbreviations: ALT: alanine aminotransferase; BMI: body mass index; AST: aspartate aminotransferase; UA: uric acid; T2DM: type 2 diabetes mellitus; TC: total cholesterol; and W:H: waist-to-hip ratio.
3. Non-Invasive or Minimally Invasive Tools
Considering the invasiveness and technical requirements of several listed variables, pharmacists can explore non-invasive alternatives for assessing NAFLD risk within the community pharmacy setting. Utilizing portable devices or scientifically validated calculators offers a more practical approach, requiring minimal training and enabling quick assessments. While these non-invasive methods may not provide the same level of precision as laboratory-based measurements, they offer a convenient snapshot of a patient’s health status. By incorporating these tools into their practice, pharmacists can efficiently screen for NAFLD risk and enhance early detection in their patients.
Listed below are some examples of portable devices and calculators that can be utilized in community pharmacy settings:
Portable devices: The examples of portable devices mentioned here aim to broaden the pharmacist’s awareness of available resources. It is essential to acknowledge that there might be other validated options specifically designed for liver measurements.
Non-Invasive Liver Fat and Fibrosis Assessment: Devices such as FibroScan (Echosens, Paris, France) or elastography can assess and predict liver fat scores and fibrosis without the need for a liver biopsy [24]. FibroScan allows for the rapid and painless evaluation of liver health, offering valuable insights into disease progression. By using transient elastography, FibroScan measures liver stiffness, indicating fibrosis severity, and controlled attenuation parameter (CAP), which estimates liver fat content. FibroScan’s benefits include its non-invasive nature, quick assessments, and real-time results. However, it is essential to consider its limitations, such as operator dependency and potential inaccuracies in certain patient populations. Despite these considerations, FibroScan remains a valuable resource for non-invasive liver assessments and aids in enhancing patient care for liver-related conditions.
Portable Ultrasound: Similar to regular ultrasound, a portable device like the Vscan Extend Dual Probe by GE Healthcare (Chicago, IL, USA) can provide a non-invasive assessment of hepatic steatosis and liver health. This portable ultrasound device offers advantages such as portability, real-time imaging, non-invasiveness, quick assessments, and a user-friendly interface, requiring minimal training. However, pharmacists should consider the higher upfront costs, limited diagnostic accuracy compared to high-end machines, and operator dependency. Other factors to consider include the device’s limited depth penetration and image quality. Despite these limitations, portable ultrasound provides valuable insights into liver health, making it a potentially useful tool for community pharmacy settings.
Portable Blood Biomarker Testing Kits: Several blood biomarker portable and quick testing kits are available in the market for pharmacists to consider. The A1CNow+ by PTS Diagnostics (Indianapolis, IN, USA) measures hemoglobin A1c (HbA1c). The CardioChek Plus by Polymer Technology Systems (Indianapolis, IN, USA) allows for the rapid assessment of multiple parameters, including total cholesterol, HDL cholesterol, triglycerides, and glucose. The Nova StatStrip Glucose/Ketone by Nova Biomedical (Waltham, MA, USA) enables simultaneous measurements of blood glucose and ketones. While these testing kits can offer rapid results at the point of care, facilitating immediate insights into biomarker levels, their analytical accuracy may be slightly limited compared to sophisticated laboratory equipment, potentially leading to marginally less precise results. Despite this drawback, these kits can provide a valuable and convenient resource for pharmacists to swiftly assess biomarkers and aid in timely patient care and management.
Calculators: In addition to the direct measurements presented above, pharmacists may also utilize indirect predictors of NAFLD. The calculators presented below were based on studies in clinical settings, thus providing some confidence to the pharmacist. While not mandatory, pharmacists may choose to utilize one or more calculators in their practice; however, this necessitates measuring or collecting additional variables as required by each calculator. If a pharmacist can obtain all 17 variables, he or she can perform all the NAFLD-predicting calculations, encompassing age, sex, ethnicity, race, BMI, diabetes mellitus (DM) status, hypertension (HTN) status, metabolic syndrome (MetS), TG, glucose, fasting insulin, albumin, platelet count, AST, ALT, CAP, and liver stiffness measurement (LSM).
4. Feasibility of Assessment
Assessing NAFLD in community pharmacy settings presents certain challenges and opportunities. The feasibility of this assessment revolves around the availability of resources and the practicality of implementing non-invasive tools. While most community pharmacists lack access to specialized laboratory equipment, they can adopt alternative approaches to efficiently screen for NAFLD risk factors. For example, sophisticated devices like FibroScan cost tens of thousands of dollars, which most pharmacies cannot afford. Additionally, they also require expertise or training to operate the device. Therefore, only pharmacies with a larger budget can consider employing such devices. Alternatively, other devices like portable ultrasound or biomarker testing kits provide less expensive options for pharmacies to consider. Lastly, to enhance feasibility, pharmacists can employ a screening questionnaire that includes key risk factors and biomarkers associated with NAFLD. Although this approach may not encompass all variables, it allows for the identification of high-risk individuals, streamlining targeted assessments.
Non-invasive portable devices and calculators offer practical solutions for community pharmacy settings. Devices like FibroScan and portable ultrasounds provide rapid liver health evaluations, offering valuable insights into disease progression. While their diagnostic accuracy may differ from clinical and laboratory-based methods, these devices present convenient and timely assessments, complementing patient care. Additionally, portable blood biomarker testing kits can offer rapid results for glucose, lipids, and liver enzymes, providing valuable insights into potential NAFLD diagnoses. Pharmacists can collaborate with nearby healthcare facilities to access more comprehensive testing capabilities, optimizing diagnostic accuracy.
Overall, with the right approach and resource management, community pharmacists can make substantial contributions to NAFLD assessment, early detection, and improved patient care within their settings. Their proactive role in implementing non-invasive tools and targeted screening questionnaires demonstrates the potential for community pharmacies to play a crucial part in the early detection and management of NAFLD, ultimately enhancing patient outcomes and overall public health.
5. Limitations and Alternate Solutions
Limitations: The specific roles of pharmacists in NAFLD management might vary depending on the health system, the availability of resources, the extent of collaboration, and, in particular, the practice of pharmacy. Despite the potential for community pharmacists to play a significant role in NAFLD management, there are certain limitations to be acknowledged. One primary limitation lies in the lack of access to specialized laboratory equipment within community pharmacy settings. While non-invasive portable devices and calculators offer practical alternatives, they may not provide the same level of precision as laboratory-based assessments. Consequently, the diagnostic accuracy of NAFLD screening in community pharmacies may be marginally reduced compared to assessments conducted in specialized healthcare facilities.
Furthermore, the implementation of NAFLD assessment and management programs in community pharmacies may require additional resources and training for pharmacists. Time constraints within busy pharmacy environments may limit the extent to which pharmacists can conduct comprehensive assessments or patient education. Additionally, the availability of qualified personnel to operate portable devices and interpret results accurately may pose a challenge.
Moreover, community pharmacists may face limitations in directly diagnosing NAFLD, as a definitive diagnosis often requires specialized medical evaluation and advanced imaging techniques, which may not be available within the pharmacy setting. As a result, community pharmacists must emphasize the importance of timely referrals to primary care physicians, gastroenterologists, or hepatologists for further evaluation and definitive diagnosis.
Alternate Solutions: Collaborative Partnerships: Community pharmacists can establish collaborative partnerships with nearby healthcare facilities or laboratories to gain access to more comprehensive testing capabilities. By working together with these institutions, pharmacists can enhance the diagnostic accuracy of NAFLD assessments and ensure timely referrals for further evaluation and specialized care.
Patient Self-Assessment Tools: To overcome the limitations of time constraints and resource availability, community pharmacists can develop patient self-assessment tools or questionnaires that encompass key risk factors and biomarkers associated with NAFLD. Patients can complete these assessments in the pharmacy or at home, providing valuable insights that can guide pharmacists in identifying high-risk individuals and facilitating appropriate follow-up.
Telehealth Services: Incorporating telehealth services within community pharmacies can broaden the reach of NAFLD management. Pharmacists can collaborate with remote healthcare providers, including gastroenterologists and hepatologists, to conduct virtual assessments and consultations with patients, enabling timely diagnosis and personalized care plans.
Program’s Evaluation: Given the lack of studies conducted within a community pharmacy setting, it is prudent to consider the potential for leveraging the expertise of pharmacists in offering personalized consultations and guidance. While the predictive accuracy of existing tools might be uncertain in this context, community pharmacists could potentially play a role in utilizing their clinical judgment and collaborating with healthcare professionals to identify individuals at risk of NAFLD based on a holistic assessment of lifestyle factors, medical history, and relevant biomarkers. This approach could underscore the unique position of pharmacists in NAFLD identification, prevention, and management within their local communities. Additionally, it presents an opportunity to generate data for potential research studies aimed at evaluating the efficacy of such programs.
This entry is adapted from the peer-reviewed paper 10.3390/pharmacy11050151
References
- Younossi, Z.M.; Koenig, A.B.; Abdelatif, D.; Fazel, Y.; Henry, L.; Wymer, M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016, 64, 73–84.
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018, 67, 328–357.
- Sheng, G.; Xie, Q.; Wang, R.; Hu, C.; Zhong, M.; Zou, Y. Waist-to-height ratio and non-alcoholic fatty liver disease in adults. BMC Gastroenterol. 2021, 21, 239.
- Zaki, M.; Amin, D.; Mohamed, R. Body composition, phenotype and central obesity indices in Egyptian women with non-alcoholic fatty liver disease. J. Complement. Integr. Med. 2020, 18, 385–390.
- Syed-Abdul, M.M.; Soni, D.S.; Barnes, J.T.; Wagganer, J.D. Comparative analysis of BIA, IBC and DXA for determining body fat in American Football players. J. Sports Med. Phys. Fit. 2021, 61, 687–692.
- Sun, G.; French, C.R.; Martin, G.R.; Younghusband, B.; Green, R.C.; Xie, Y.-G.; Mathews, M.; Barron, J.R.; Fitzpatrick, D.G.; Gulliver, W.; et al. Comparison of multifrequency bioelectrical impedance analysis with dual-energy X-ray absorptiometry for assessment of percentage body fat in a large, healthy population. Am. J. Clin. Nutr. 2005, 81, 74–78.
- Ballestri, S.; Zona, S.; Targher, G.; Romagnoli, D.; Baldelli, E.; Nascimbeni, F.; Roverato, A.; Guaraldi, G.; Lonardo, A. Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2016, 31, 936–944.
- Romeo, S.; Kozlitina, J.; Xing, C.; Pertsemlidis, A.; Cox, D.; Pennacchio, L.A.; Boerwinkle, E.; Cohen, J.C.; Hobbs, H.H. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 2008, 40, 1461–1465.
- Boza, C.; Riquelme, A.; Ibanez, L.; Duarte, I.; Norero, E.; Viviani, P.; Soza, A.; Fernandez, J.I.; Raddatz, A.; Guzman, S.; et al. Predictors of nonalcoholic steatohepatitis (NASH) in obese patients undergoing gastric bypass. Obes. Surg. 2005, 15, 1148–1153.
- Chisholm, J.; Seki, Y.; Toouli, J.; Stahl, J.; Collins, J.; Kow, L. Serologic predictors of nonalcoholic steatohepatitis in a population undergoing bariatric surgery. Surg. Obes. Relat. Dis. 2012, 8, 416–422.
- Dixon, J.B.; Bhathal, P.S.; O’Brien, P.E. Nonalcoholic fatty liver disease: Predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology 2001, 121, 91–100.
- Gobato, A.O.; Vasques, A.C.J.; Yamada, R.M.; Zambon, M.P.; Barros-Filho, A.D.A.; Hessel, G. Biochemical, anthropometric and body composition indicators as predictors of hepatic steatosis in obese adolescents. Rev. Paul. Pediatr. 2014, 32, 230–236.
- Kabir, M.A.; Uddin, M.Z.; Siddiqui, N.I.; Robi, I.H.; Malek, M.S.; Islam, M.S.; Rahman, S.; Hossain, M.S.; Mahapatra, S.K.; Alam, M.J.; et al. Prevalence of Non-Alcoholic Fatty Liver Disease and Its Biochemical Predictors in Patients with Type-2 Diabetes Mellitus. Mymensingh Med. J. 2018, 27, 237–244.
- Kim, J.Y.; Cho, J.; Yang, H.R. Biochemical Predictors of Early Onset Non-Alcoholic Fatty Liver Disease in Young Children with Obesity. J. Korean Med. Sci. 2018, 33, e122.
- Li, Y.; Xu, C.; Yu, C.; Xu, L.; Miao, M. Association of serum uric acid level with non-alcoholic fatty liver disease: A cross-sectional study. J. Hepatol. 2009, 50, 1029–1034.
- Licata, A.; Nebbia, M.E.; Cabibbo, G.; Iacono, G.L.; Barbaria, F.; Brucato, V.; Alessi, N.; Porrovecchio, S.; Di Marco, V.; Craxi, A.; et al. Hyperferritinemia is a risk factor for steatosis in chronic liver disease. World J. Gastroenterol. 2009, 15, 2132–2138.
- Lonardo, A.; Loria, P.; Leonardi, F.; Borsatti, A.; Neri, P.; Pulvirenti, M.; Verrone, A.M.; Bagni, A.; Bertolotti, M.; Ganazzi, D.; et al. Fasting insulin and uric acid levels but not indices of iron metabolism are independent predictors of non-alcoholic fatty liver disease. A case-control study. Dig Liver Dis. 2002, 34, 204–211.
- Petta, S.; Camma, C.; Cabibi, D.; Di Marco, V.; Craxi, A. Hyperuricemia is associated with histological liver damage in patients with non-alcoholic fatty liver disease. Aliment. Pharmacol. Ther. 2011, 34, 757–766.
- Praveenraj, P.; Gomes, R.M.; Kumar, S.; Karthikeyan, P.; Shankar, A.; Parthasarathi, R.; Senthilnathan, P.; Rajapandian, S.; Palanivelu, C. Prevalence and Predictors of Non-Alcoholic Fatty Liver Disease in Morbidly Obese South Indian Patients Undergoing Bariatric Surgery. Obes. Surg. 2015, 25, 2078–2087.
- Puljiz, Z.; Stimac, D.; Kovac, D.; Puljiz, M.; Bratanic, A.; Kovacic, V.; Kardum, D.; Bonacin, D.; Hozo, I. Predictors of nonalcoholic steatohepatitis in patients with elevated alanine aminotransferase activity. Coll. Antropol. 2010, 34 (Suppl. S1), 33–37.
- Ryu, S.; Chang, Y.; Kim, S.G.; Cho, J.; Guallar, E. Serum uric acid levels predict incident nonalcoholic fatty liver disease in healthy Korean men. Metabolism 2011, 60, 860–866.
- Ulitsky, A.; Ananthakrishnan, A.N.; Komorowski, R.; Wallace, J.; Surapaneni, S.N.; Franco, J.; Saeian, K.; Gawrieh, S. A noninvasive clinical scoring model predicts risk of nonalcoholic steatohepatitis in morbidly obese patients. Obes. Surg. 2010, 20, 685–691.
- Sirota, J.C.; McFann, K.; Targher, G.; Johnson, R.J.; Chonchol, M.; Jalal, D.I. Elevated serum uric acid levels are associated with non-alcoholic fatty liver disease independently of metabolic syndrome features in the United States: Liver ultrasound data from the National Health and Nutrition Examination Survey. Metabolism 2013, 62, 392–399.
- Ali, A.H.; Al Juboori, A.; Petroski, G.F.; Diaz-Arias, A.A.; Syed-Abdul, M.M.; Wheeler, A.A.; Ganga, R.R.; Pitt, J.B.; Spencer, N.M.; Hammoud, G.M.; et al. The Utility and Diagnostic Accuracy of Transient Elastography in Adults with Morbid Obesity: A Prospective Study. J. Clin. Med. 2022, 11, 1201.
This entry is offline, you can click here to edit this entry!
