Alzheimer’s disease (AD) is a progressive neurodegenerative disorder and represents the leading cause of cognitive impairment and dementia in older individuals throughout the world. The main hallmarks of AD include brain atrophy, extracellular deposition of insoluble amyloid-β (Aβ) plaques, and the intracellular aggregation of protein tau in neurofibrillary tangles. These pathological modifications start many years prior to clinical manifestations of disease and the spectrum of AD progresses along a continuum from preclinical to clinical phases. Therefore, identifying specific biomarkers for detecting AD at early stages greatly improves clinical management. However, stable and non-invasive biomarkers are not currently available for the early detection of the disease. In the search for more reliable biomarkers, epigenetic mechanisms, able to mediate the interaction between the genome and the environment, are emerging as important players in AD pathogenesis.
- epigenetics
- Alzheimer’s disease
- biomarkers
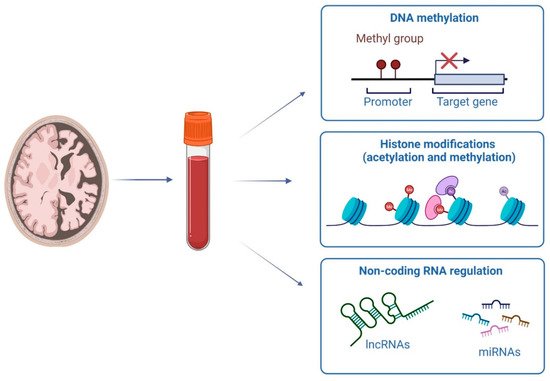
1. Overview of the Main Epigenetic Mechanisms
2. DNA Methylation Investigations in Early AD Stages
This entry is adapted from the peer-reviewed paper 10.3390/genes13081308
References
- Liu, X.; Jiao, B.; Shen, L. The Epigenetics of Alzheimer’s Disease: Factors and Therapeutic Implications. Front. Genet. 2018, 9, 579.
- Li, E.; Zhang, Y. DNA Methylation in Mammals. Cold Spring Harb. Perspect. Biol. 2014, 6, a019133.
- Christopher, M.A.; Kyle, S.M.; Katz, D.J. Neuroepigenetic mechanisms in disease. Epigenetics Chromatin 2017, 10, 47.
- Rots, M.G.; Mposhi, A.; van der Wijst, M.G.; Faber, K.N. Regulation of mitochondrial gene expression the epigenetic enigma. Front. Biosci. 2017, 22, 1099–1113.
- Patil, V.; Ward, R.; Hesson, L.B. The evidence for functional non-CpG methylation in mammalian cells. Epigenetics 2014, 9, 823–828.
- Boulias, K.; Greer, E.L. Means, mechanisms and consequences of adenine methylation in DNA. Nat. Rev. Genet. 2022, 23, 411–428.
- Cheng, Y.; Xie, N.; Jin, P.; Wang, T. DNA methylation and hydroxymethylation in stem cells. Cell Biochem. Funct. 2015, 33, 161–173.
- Bano, D.; Salomoni, P.; Ehninger, D.; Nicotera, P. The histone code in dementia: Transcriptional and chromatin plasticity fades away. Curr. Opin. Pharmacol. 2021, 60, 117–122.
- Stoccoro, A.; Coppedè, F. Role of epigenetics in Alzheimer’s disease pathogenesis. Neurodegener. Dis. Manag. 2018, 8, 181–193.
- O’Brien, J.; Hayder, H.; Zayed, Y.; Peng, C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018, 9, 402.
- Zhang, X.; Wang, W.; Zhu, W.; Dong, J.; Cheng, Y.; Yin, Z.; Shen, F. Mechanisms and Functions of Long Non-Coding RNAs at Multiple Regulatory Levels. Int. J. Mol. Sci. 2019, 20, 5573.
- Mirbahai, L.; Chipman, J.K. Epigenetic memory of environmental organisms: A reflection of lifetime stressor exposures. Mutat. Res. Toxicol. Environ. Mutagen. 2014, 764–765, 10–17.
- Berdasco, M.; Esteller, M. Clinical epigenetics: Seizing opportunities for translation. Nat. Rev. Genet. 2018, 20, 109–127.
- Plagg, B.; Ehrlich, D.; Kniewallner, K.; Marksteiner, J.; Humpel, C. Increased Acetylation of Histone H4 at Lysine 12 (H4K12) in Monocytes of Transgenic Alzheimer’s Mice and in Human Patients. Curr. Alzheimer Res. 2015, 12, 752–760.
- West, R.L.; Lee, J.M.; Maroun, L.E. Hypomethylation of the amyloid precursor protein gene in the brain of an alzheimer’s disease patient. J. Mol. Neurosci. 1995, 6, 141–146.
- Kurdyukov, S.; Bullock, M. DNA Methylation Analysis: Choosing the Right Method. Biology 2016, 5, 3.
- Merkel, A.; Esteller, M. Experimental and Bioinformatic Approaches to Studying DNA Methylation in Cancer. Cancers 2022, 14, 349.
- Lunnon, K.; Smith, R.G.; Cooper, I.; Greenbaum, L.; Mill, J.; Beeri, M.S. Blood methylomic signatures of presymptomatic dementia in elderly subjects with type 2 diabetes mellitus. Neurobiol. Aging 2014, 36, 1600.e1–1600.e4.
- De Jager, P.L.; Srivastava, G.; Lunnon, K.; Burgess, J.; Schalkwyk, L.C.; Yu, L.; Eaton, M.L.; Keenan, B.T.; Ernst, J.; McCabe, C.; et al. Alzheimer’s disease: Early alterations in brain DNA methylation at ANK1, BIN1, RHBDF2 and other loci. Nat. Neurosci. 2014, 17, 1156–1163.
- Lunnon, K.; Smith, R.; Hannon, E.; De Jager, P.L.; Srivastava, G.; Volta, M.; Troakes, C.; Al-Sarraj, S.; Burrage, J.; Macdonald, R.; et al. Methylomic profiling implicates cortical deregulation of ANK1 in Alzheimer’s disease. Nat. Neurosci. 2014, 17, 1164–1170.
- Luo, M.; Zhou, X.; Ji, H.; Ma, W.; Liu, G.; Dai, D.; Li, J.; Chang, L.; Xu, L.; Jiang, L.; et al. Population Difference in the Associations of KLOTH Promoter Methylation with Mild Cognitive Impairment in Xinjiang Uygur and Han Populations. PLoS ONE 2015, 10, e0132156.
- Ma, W.; Zhou, X.; Ji, H.; Luo, M.; Liu, G.; Li, J.; Wang, Q.; Duan, S. Population difference in the association of BDNF promoter methylation with mild cognitive impairment in the Xinjiang Uygur and Han populations. Psychiatry Res. 2015, 229, 926–932.
- Liu, G.; Ji, H.; Liu, J.; Xu, C.; Chang, L.; Cui, W.; Ye, C.; Hu, H.; Chen, Y.; Zhou, X.; et al. Association of OPRK1 and OPRM1 methylation with mild cognitive impairment in Xinjiang Han and Uygur populations. Neurosci. Lett. 2016, 636, 170–176.
- Zou, T.; Chen, W.; Zhou, X.; Duan, Y.; Ying, X.; Liu, G.; Zhu, M.; Pari, A.; Alimu, K.; Miao, H.; et al. Association of multiple candidate genes with mild cognitive impairment in an elderly Chinese Uygur population in Xinjiang. Psychogeriatrics 2019, 19, 574–583.
- Yu, Y.; Mingjiao, W.; Yang, X.; Sui, M.; Zhang, T.; Liang, J.; Gu, X.; Wang, X. Association between DNA methylation of SORL1 5′-flanking region and mild cognitive impairment in type 2 diabetes mellitus. Ann. D’endocrinologie 2016, 77, 625–632.
- Kobayashi, N.; Shinagawa, S.; Nagata, T.; Shimada, K.; Shibata, N.; Ohnuma, T.; Kasanuki, K.; Arai, H.; Yamada, H.; Nakayama, K.; et al. Development of Biomarkers Based on DNA Methylation in the NCAPH2/LMF2 Promoter Region for Diagnosis of Alzheimer’s Disease and Amnesic Mild Cognitive Impairment. PLoS ONE 2016, 11, e0146449.
- Shinagawa, S.; Kobayashi, N.; Nagata, T.; Kusaka, A.; Yamada, H.; Kondo, K.; Nakayama, K. DNA methylation in the NCAPH2/LMF2 promoter region is associated with hippocampal atrophy in Alzheimer’s disease and amnesic mild cognitive impairment patients. Neurosci. Lett. 2016, 629, 33–37.
- Kobayashi, N.; Shinagawa, S.; Nagata, T.; Shimada, K.; Shibata, N.; Ohnuma, T.; Kasanuki, K.; Arai, H.; Yamada, H.; Nakayama, K.; et al. Usefulness of DNA Methylation Levels in COASY and SPINT1 Gene Promoter Regions as Biomarkers in Diagnosis of Alzheimer’s Disease and Amnestic Mild Cognitive Impairment. PLoS ONE 2016, 11, e0168816.
- Kobayashi, N.; Shinagawa, S.; Niimura, H.; Kida, H.; Nagata, T.; Tagai, K.; Shimada, K.; Oka, N.; Shikimoto, R.; Noda, Y.; et al. Increased blood Coasy DNA methylation levels a potential biomarker for early pathology of Alzheimer’s disease. Sci. Rep. 2020, 10, 12217.
- Bednarska-Makaruk, M.; Graban, A.; Sobczyńska-Malefora, A.; Harrington, D.J.; Mitchell, M.; Voong, K.; Dai, L.; Łojkowska, W.; Bochyńska, A.; Ryglewicz, D.; et al. Homocysteine metabolism and the associations of global DNA methylation with selected gene polymorphisms and nutritional factors in patients with dementia. Exp. Gerontol. 2016, 81, 83–91.
- Sung, H.Y.; Choi, B.-O.; Jeong, J.H.; Kong, K.A.; Hwang, J.; Ahn, J.-H. Amyloid β-Mediated Hypomethylation of Heme Oxygenase 1 Correlates with Cognitive Impairment in Alzheimer’s Disease. PLoS ONE 2016, 11, e0153156.
- Xie, B.; Xu, Y.; Liu, Z.; Liu, W.; Jiang, L.; Zhang, R.; Cui, D.; Zhang, Q.; Xu, S. Elevation of Peripheral BDNF Promoter Methylation Predicts Conversion from Amnestic Mild Cognitive Impairment to Alzheimer’s Disease: A 5-Year Longitudinal Study. J. Alzheimer’s Dis. 2017, 56, 391–401.
- Xie, B.; Liu, Z.; Liu, W.; Jiang, L.; Zhang, R.; Cui, D.; Zhang, Q.; Xu, S. DNA Methylation and Tag SNPs of the BDNF Gene in Conversion of Amnestic Mild Cognitive Impairment into Alzheimer’s Disease: A Cross-Sectional Cohort Study. J. Alzheimer’s Dis. 2017, 58, 263–274.
- Fransquet, P.D.; Ritchie, K.; Januar, V.; Saffery, R.; Ancelin, M.-L.; Ryan, J. Is Peripheral BDNF Promoter Methylation a Preclinical Biomarker of Dementia? J. Alzheimer’s Dis. 2020, 73, 645–655.
- Fransquet, P.; Lacaze, P.; Saffery, R.; Phung, J.; Parker, E.; Shah, R.; Murray, A.; Woods, R.L.; Ryan, J. Blood DNA methylation signatures to detect dementia prior to overt clinical symptoms. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2020, 12, e12056.
- Fransquet, P.D.; Lacaze, P.; Saffery, R.; Phung, J.; Parker, E.; Shah, R.C.; Murray, A.; Woods, R.L.; Ryan, J. DNA methylation analysis of candidate genes associated with dementia in peripheral blood. Epigenomics 2020, 12, 2109–2123.
- Chouliaras, L.; Pishva, E.; Haapakoski, R.; Zsoldos, E.; Mahmood, A.; Filippini, N.; Burrage, J.; Mill, J.; Kivimäki, M.; Lunnon, K.; et al. Peripheral DNA methylation, cognitive decline and brain aging: Pilot findings from the Whitehall II imaging study. Epigenomics 2018, 10, 585–595.
- Bakulski, K.M.; Dolinoy, D.C.; Sartor, M.A.; Paulson, H.L.; Konen, J.R.; Lieberman, A.P.; Albin, R.L.; Hu, H.; Rozek, L.S. Genome-Wide DNA Methylation Differences Between Late-Onset Alzheimer’s Disease and Cognitively Normal Controls in Human Frontal Cortex. J. Alzheimer’s Dis. 2012, 29, 571–588.
- Parachikova, A.; Agadjanyan, M.; Cribbs, D.; Blurton-Jones, M.; Perreau, V.; Rogers, J.; Beach, T.; Cotman, C. Inflammatory changes parallel the early stages of Alzheimer disease. Neurobiol. Aging 2007, 28, 1821–1833.
- Pathak, G.A.; Silzer, T.K.; Sun, J.; Zhou, Z.; Daniel, A.A.; Johnson, L.; O’Bryant, S.; Phillips, N.R.; Barber, R.C. Genome-Wide Methylation of Mild Cognitive Impairment in Mexican Americans Highlights Genes Involved in Synaptic Transport, Alzheimer’s Disease-Precursor Phenotypes, and Metabolic Morbidities. J. Alzheimer’s Dis. 2019, 72, 733–749.
- An, Y.; Feng, L.; Zhang, X.; Wang, Y.; Wang, Y.; Tao, L.; Qin, Z.; Xiao, R. Dietary intakes and biomarker patterns of folate, vitamin B6, and vitamin B12 can be associated with cognitive impairment by hypermethylation of redox-related genes NUDT15 and TXNRD1. Clin. Epigenetics 2019, 11, 139.
- Lardenoije, R.; Roubroeks, J.A.Y.; Pishva, E.; Leber, M.; Wagner, H.; Iatrou, A.; Smith, A.; Smith, R.G.; Eijssen, L.M.T.; Kleineidam, L.; et al. Alzheimer’s disease-associated (hydroxy)methylomic changes in the brain and blood. Clin. Epigenetics 2019, 11, 164.
- Roubroeks, J.A.; Smith, A.R.; Smith, R.G.; Pishva, E.; Ibrahim, Z.; Sattlecker, M.; Hannon, E.J.; Kłoszewska, I.; Mecocci, P.; Soininen, H.; et al. An epigenome-wide association study of Alzheimer’s disease blood highlights robust DNA hypermethylation in the HOXB6 gene. Neurobiol. Aging 2020, 95, 26–45.
- Shao, Y.; Shaw, M.; Todd, K.; Khrestian, M.; D’Aleo, G.; Barnard, P.J.; Zahratka, J.; Pillai, J.; Yu, C.-E.; Keene, C.D.; et al. DNA methylation of TOMM40-APOE-APOC2 in Alzheimer’s disease. J. Hum. Genet. 2018, 63, 459–471.
- Mancera-Páez, O.; Estrada-Orozco, K.; Mahecha, M.F.; Cruz, F.; Bonilla-Vargas, K.; Sandoval, N.; Guerrero, E.; Salcedo-Tacuma, D.; Melgarejo, J.D.; Vega, E.; et al. Differential Methylation in APOE (Chr19; Exon Four; from 44,909,188 to 44,909,373/hg38) and Increased Apolipoprotein E Plasma Levels in Subjects with Mild Cognitive Impairment. Int. J. Mol. Sci. 2019, 20, 1394.
- Vasanthakumar, A.; Davis, J.W.; Idler, K.; Waring, J.F.; Asque, E.; Riley-Gillis, B.; Grosskurth, S.; Srivastava, G.; Kim, S.; Nho, K.; et al. Harnessing peripheral DNA methylation differences in the Alzheimer’s Disease Neuroimaging Initiative (ADNI) to reveal novel biomarkers of disease. Clin. Epigenetics 2020, 12, 84.
- Wang, Q.; Chen, Y.; Readhead, B.; Chen, K.; Su, Y.; Reiman, E.M.; Dudley, J.T. Longitudinal data in peripheral blood confirm that PM20D1 is a quantitative trait locus (QTL) for Alzheimer’s disease and implicate its dynamic role in disease progression. Clin. Epigenetics 2020, 12, 189.
- Li, Q.S.; Vasanthakumar, A.; Davis, J.W.; Idler, K.B.; Nho, K.; Waring, J.F.; Saykin, A.J. Association of peripheral blood DNA methylation level with Alzheimer’s disease progression. Clin. Epigenetics 2021, 13, 191.
- Pérez, R.F.; Alba-Linares, J.J.; Tejedor, J.R.; Fernández, A.F.; Calero, M.; Román-Domínguez, A.; Borrás, C.; Viña, J.; Ávila, J.; Medina, M.; et al. Blood DNA Methylation Patterns in Older Adults with Evolving Dementia. J. Gerontol. Ser. A 2022.
- Hu, H.; Tan, L.; Bi, Y.-L.; Xu, W.; Tan, L.; Shen, X.-N.; Hou, X.-H.; Ma, Y.-H.; Dong, Q.; Yu, J.-T. Association between methylation of BIN1 promoter in peripheral blood and preclinical Alzheimer’s disease. Transl. Psychiatry 2021, 11, 89.
- Yu, L.; Chibnik, L.B.; Srivastava, G.P.; Pochet, N.; Yang, J.; Xu, J.; Kozubek, J.; Obholzer, N.; Leurgans, S.E.; Schneider, J.A.; et al. Association of Brain DNA Methylation in SORL1, ABCA7, HLA-DRB5, SLC24A4, and BIN1 with Pathological Diagnosis of Alzheimer Disease. JAMA Neurol. 2015, 72, 15–24.
- Stoccoro, A.; Baldacci, F.; Ceravolo, R.; Giampietri, L.; Tognoni, G.; Siciliano, G.; Migliore, L.; Coppedè, F. Increase in Mitochondrial D-Loop Region Methylation Levels in Mild Cognitive Impairment Individuals. Int. J. Mol. Sci. 2022, 23, 5393.
- Sanchez-Mut, J.V.; Heyn, H.; Silva, B.A.; Dixsaut, L.; Esparcia, P.G.; Vidal, E.; Sayols, S.; Glauser, L.; Monteagudo-Sánchez, A.; Perez-Tur, J.; et al. PM20D1 is a quantitative trait locus associated with Alzheimer’s disease. Nat. Med. 2018, 24, 598–603.
- Sanchez-Mut, J.V.; Glauser, L.; Monk, D.; Gräff, J. Comprehensive analysis of PM20D1 QTL in Alzheimer’s disease. Clin. Epigenetics 2020, 12, 20.
- Coto-Vílchez, C.; Martínez-Magaña, J.J.; Mora-Villalobos, L.; Valerio, D.; Genis-Mendoza, A.D.; Silverman, J.M.; Nicolini, H.; Raventós, H.; Chavarria-Soley, G. Genome-wide DNA methylation profiling in nonagenarians suggests an effect of PM20D1 in late onset Alzheimer’s disease. CNS Spectr. 2021, 1–9.
