The term ‘cytokine storm’ (CS) applies to a pathological autoimmune reaction when the interactions that lead to cytokine production are destabilised and may even lead to death. CS may be induced by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. It is noteworthy that many of the criteria used to diagnose HLH are described as COVID-19 mortality predictors. Cytokine storms are considered to be an important cause of death in patients with the severe course of SARS-CoV-2 infection. Due to the fact that pregnant women are in an immunosuppressive state, viral pulmonary infections are more perilous for them—possible risks include miscarriage, intrauterine growth restriction or birth before the term; sometimes ventilation support is needed. HLH should be considered in pregnant and puerperal women suffering from moderately severe to severe COVID-19 and presenting with: fever unresponsive to antibiotic therapy, cytopenia, hepatitis and hyperferritinaemia.
1. Introduction
Pregnancy is a special time in a woman’s life. During this period, physiological changes take place not only in the endocrine system but in the immune system as well. Trophoblasts and the maternal immune system reach a consensus, and the immune response during pregnancy is a combination of the maternal systemic response and the local foetal-placental response. Scientific studies have shown that due to immune changes, also associated with altered cellular immunity, pregnant women are susceptible to severe infectious respiratory diseases [
1,
2]. Their response to microorganisms varies according to the type of pathogen and stage of pregnancy. Many pathologies developing during pregnancy, e.g., preeclampsia (PE), result from abnormal immune changes. An abnormal response of the maternal immune system to the placenta may be the first pathogenetic stage of PE, followed by a systemic inflammatory response [
3].
A cytokine storm (CS) is a form of uncontrolled systemic inflammatory response that may even lead to death. It can be caused by various factors, most often by an infection, systemic diseases (such as rheumatoid arthritis, systemic lupus erythematosus) and, though quite rarely, by anaphylaxis [
4]. A CS may also be triggered by medical interventions, such as transplantation or drug administration [
5], or induced by SARS-CoV-2 infection [
6].
2. Physiological Changes in the Immune System during Pregnancy
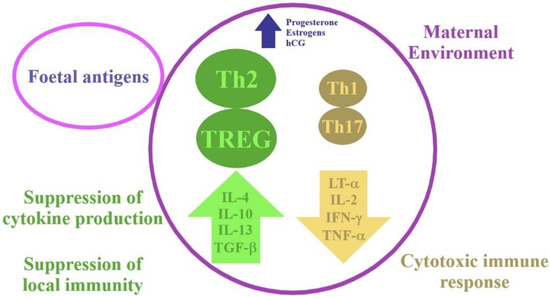
Pregnancy is a state in which there are temporary changes in the maternal immune response. These adaptations are made to protect the mother and the foetus from pathogens while avoiding a deleterious immune response against the foetus. Macrophages, dendritic cells, neutrophils and natural killer (NK) cells participate in a coordinated, controlled immune response in early pregnancy, which is needed for implantation and pregnancy progression. The maternal immune T-cell profile shifts from the type 1 T helper cells (Th1) dominance to the type 2 T helper cells (Th2) dominance, which is a physiological state (Figure 1).
Figure 1. Physiological changes in the immune system in early pregnancy. hCG-human chorionic gonadotropin; IFN-γ-interferon gamma; IL-2-interleukin 2; IL-4-interleukin 4; IL-10-interleukin 10; IL-13-interleukin 13; LT-α-lymphotoxin-alpha; TGF-β-transforming growth factor beta; Th1-type 1 T helper cells; Th2-type 2 T helper cells; Th17-T helper 17 cells; TNF-α-tumour necrosis factor; TREG-regulatory T cell.
3. Immunological Aspects in COVID-19 and HLH
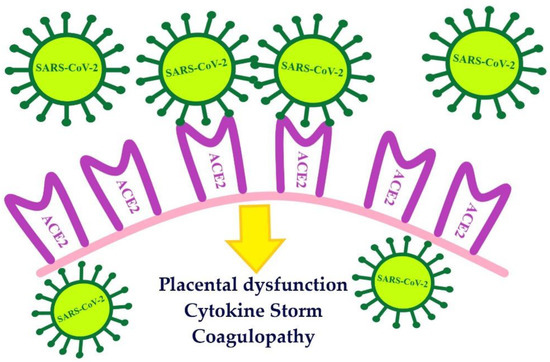
SARS-CoV-2 is a beta coronavirus most closely related to SARS-CoV. It is reported that the homology between the genome of the SARS-CoV-2 and SARS-CoV is 82% [
10]. In order to gain entry to the cells, both viruses use the angiotensin-converting enzyme-related carboxypeptidase (ACE2) receptor. The attachment of the virus with ACE2, as its cellular receptor, triggers internalisation of the complex into the target cell, leading to the down-regulation of the ACE2 [
11]. SARS-CoV-2 enters the cell through the ACE2 receptor, the activity of which is increased in normal pregnancy [
12] (
Figure 2).
Figure 2. The number of ACE2 receptors increases during early and mid-pregnancy. ACE2 are receptors for the entry of SARS-CoV-2 into placental cells. ACE2-angiotensin-converting enzyme-related carboxypeptidase; SARS-CoV-2-severe acute respiratory syndrome coronavirus 2.
The term ‘cytokine storm’ applies to a pathological autoimmune reaction when the interactions that lead to cytokine production are destabilised. The other cells of the immune system are affected by the positive feedback driven by the overproduced cytokines. It results in producing unrestrained inflammation within the tissues and key organs and induces an autoimmune system attack [
14]. The damage is usually removed due to regeneration; however, in a cytokine storm, more serious effects of inflammation are involved, including diffuse alveolar damage or wound fibrosis [
16]. Cytokine storms are associated with sepsis and septic shock, influenza, acute respiratory distress and a toxic response to medication. Cytokine storms are considered to be an important cause of death in patients with the severe course of SARS-CoV-2 infection [
14].
Patients suffering from COVID-19 have abnormal laboratory results, i.e., the levels of inflammatory cytokines-interleukin 6 (IL-6), interleukin 1β (IL-1β), TNF-α, procalcitonin, C-reactive protein (CRP) and angiotensin II are increased, highlighting the role of the inflammatory responses in the disease [
16]. Increased levels of several cytokines, especially interleukin IL-1β, interleukin 2 (IL-2), IL-6, interleukin 7 (IL-7), IL-10, TNFα and granulocyte colony-stimulating factor (G-CSF) were observed in patients with SARS-CoV-2. The number of total T, B and NK cells was significantly reduced in COVID-19 patients. Furthermore, the CD8+ T cells were skewing toward a senescent phenotype. As a consequence, the CD4+ T, CD8+ T and NK cells presented decreased antiviral cytokine productivity. Cytokines, such as interleukin 12 IL12, IL15 and IL21, which are important for NK-cell activity, were not discovered consistently. Reduced cytotoxic potential was discovered, especially in COVID-19 patients who required intensive care [
17,
18].
HLH is classified as one of the cytokine storm syndromes (CSS). HLH is a rare, life-threatening disorder. It may be provoked either by a primary genetic defect or associated with several diseases such as infection, haematologic malignancy, rheumatologic illness, immunodeficiency syndromes, autoimmune diseases and drugs. Most of the reported cases were associated with a viral infection, including Epstein-Barr virus (EBV), human immunodeficiency viruses, cytomegalovirus, herpes simplex virus, influenza virus, hepatitis-B-virus and parvovirus B19 [
20,
21,
22]. The methods by which viruses cause HLH have not yet been fully explained. Various factors may play a role. Viruses, particularly DNA viruses, have the ability to modulate the immune response. Herpes viruses, in particular, exploit this technique [
23]. They can enhance the host’s vulnerability to HLH by deliberately avoiding effector immune responses and causing a cytokine imbalance. Pathogenic microbes cause excessive T-cell and macrophage proliferation and activation, resulting in dysregulated cellular immunity and Th1/Th2 ratios, excessive Th1 cell activation, secretion of large amounts of cytokines that activate cytotoxic T cells (CTLs) and macrophages, proliferation of a large number of CTLs, and enhanced phagocytosis in macrophages [
24]. These pathogenic microbes also stimulate macrophages, DCs, NK cells, and CTLs, resulting in a cytokine storm that destroys target cells. CTLs will be continually activated by proliferative signals and release huge quantities of IFN, causing macrophages to secrete different cytokines and chemokines, culminating in a cascade of uncontrolled inflammatory reactions if immune cell activation is not halted [
24].
The immune mechanism of the COVID-19 cytokine storm may be related to virus-induced immunosuppression and NK cell dysfunction [
31]. NK cells responses are of enormous significance for antiviral immune responses. A recently published study of COVID-19 patients revealed that severe disease was associated with NKG2C+ NK cell prevalence. After the interaction between CD94/NKG2C and its cellular ligand HLA-E, cytotoxic NK cell responses are activated. As the result of that interaction, pro-inflammatory effector molecules of NKG2C+ cells are released against virus-infected cells [
31].
4. The Course of COVID-19 in Pregnant and Postpartum Women
Due to the fact that pregnant women are in an immunosuppressive state, viral pulmonary infections are more perilous for them than infections of bacterial origin, and they are particularly susceptible to respiratory pathogens and severe pneumonia. Physiologic adaptive changes during pregnancy, including diaphragm elevation, increased oxygen consumption and changes in the mucous membrane of the respiratory tract, render them intolerant to hypoxia. Pneumonia is a type of lung disease that can be very dangerous for pregnant women—possible risks include miscarriage, intrauterine growth restriction or birth before the term; sometimes ventilation support is needed [
35].
Among pregnant women with the COVID-19 symptoms, 4.99% were admitted to the ICU [
40]. Maternal mortality was 1–1.3%, and the rate of severe pneumonia ranged from 0 to 14% [
40,
41]. It has been found that COVID-19 increased the risk of several frequent pregnancy conditions, including PE and pulmonary embolism [
37]. A high body mass index, PE, and pre-existing diabetes have been associated with the severe course of COVID-19. Moreover, existing comorbidities in pregnant women were a major risk factor for ICU admission and mechanical ventilation. Furthermore, a severe coexisting disease was found to be the main cause of death in pregnant women infected with COVID-19 [
37,
39,
41].
Current specialist literature provides information that the majority of clinical manifestations are detected in the late third trimester. Thus, it may not be the mere virus causing severe condition but comorbidities as well. In light of this, it appears that physicians should be alert to the possibility of a severe course of COVID-19 in pregnant women who present risk factors linked to maternal morbidity. Therefore, a proper follow-up of such patients is necessary.
5. The Course of HLH in Pregnant and Postpartum Women
Pregnancy is a physiological process, and the HLH syndrome is rarely diagnosed in pregnant women. Cytotoxic T cells, macrophages and NK cells play an essential role in HLH. Excessive activation and proliferation of T-cells and macrophages, and secretion of large amounts of cytokines, may be responsible for multiple organ failure, including the liver, brain and bone marrow, which can be potentially fatal [47]. The levels of cytokines such as TNF-α, IL-1β, IL-6, IL-10, and IFN-γ increase in HLH [48].
In order to diagnose HLH, either molecular diagnostics consistent with HLH must be performed or five of the eight diagnostic criteria for HLH must be fulfilled, i.e., splenomegaly, fever, cytopenia (affecting two or more of three lineages in the peripheral blood), hypofibrinogenaemia and/or hypertriglyceridaemia, elevated levels of ferritin, haemophagocytosis in the bone marrow/spleen/lymph nodes, low or absent NK cell activity and increased levels of soluble CD25 (interleukin [IL]-2 receptor), or both [26].
HLH in the group of pregnant and postpartum women accounts for high morbidity and mortality among them. Therefore, effective treatment is needed in order to reduce mortality and prevent ICU admission in this population. For this reason, it is important to diagnose the disease timely and implement appropriate treatment promptly. No treatment scheme has been developed for pregnant women so far. However, the HLH-2004 protocol is usually used at the beginning of treatment. The protocol includes therapy with dexamethasone 10 mg/m
2 daily, etoposide 150 mg/m
2 twice a week and cyclosporine, followed by dexamethasone intravenous pulses [
54]. Steroids are used as the first line of treatment. The use of etoposide, which is a potential teratogenic drug, is controversial in the case of pregnant women. Etoposide might also induce secondary malignancies, especially acute myeloid leukaemia (the risk is estimated at 0.3 to 0.4%) [
55]. For these reasons, it is better to use steroids as the first line therapy and intravenous immunoglobulins or cyclosporine in steroids-resistant patients [
21,
26]. If the central nervous system is affected, intrathecal methotrexate infusions can be used [
54].
6. Associations between HLH and COVID-19
Recently, some similarity has been noticed between moderate and severe COVID-19 and HLH (Table 1).
Table 1. Moderately severe to severe COVID-19 as a form of sHLH. sHLH—secondary haemophagocytic lymphohistiocytosis; COVID-19—coronavirus disease 2019; HLH—haemophagocytic lymphohistiocytosis; IL-6—interleukin 6.
| Moderately Severe to Severe COVID-19 |
sHLH |
| prevalence in pregnant women—rarely diagnosed |
| aetiology |
| viral infection |
viral infection in most cases |
| hyperferritinaemia |
| marker of poor prognosis in COVID-19 patients |
the most characteristic laboratory result of HLH |
| treatment |
| treatment aimed at suppressing the cytokine storm |
| high mortality |
| increased levels of IL-6 |
Treatment of patients with the severe course of COVID-19 is difficult because the only treatment option available for ARDS is symptomatic treatment. The HLH-2004 protocol has been successfully used in HLH triggered by EBV, HBV and influenza A virus subtype (A/H1N1) infections [
55]. These observations suggest that this therapy could be effective in the treatment of COVID-19 patients with the severe course of the disease.
It is noteworthy that many of the criteria used to diagnose HLH are described as COVID-19 mortality predictors [
56]. A relationship has been observed between the median time from the onset of COVID-19 symptoms to ARDS (which was 8.0–14.0 days) and HLH development during A/H1N1 infection. Hamizi et al. suggest that moderately severe to severe COVID-19 might be a form of sHLH [
56]. A cytokine storm has been reported in the ICU patients suffering from SARS-CoV-2 infection [
57].
However, some research suggests that the use of HScore to identify the COVID-19 cytokine storm is of limited value [
59,
60].
Treatment with etoposide and dexamethasone is aimed at suppressing the cytokine storm, and therefore, it may be potentially effective in the treatment of patients with severe COVID-19. It has been shown that etoposide removes activated T lymphocytes and effectively suppresses a cytokine storm. However, no direct anti-inflammatory effect on macrophages or dendritic cells and no deletion of quiescent naive or memory T cells have been reported. Despite the risks associated with administration of etoposide, it could reduce mortality and the nervous system complications in patients with the severe course of COVID-19 [
56]. It is noteworthy that in the case of sHLH and sepsis, mortality is very high (66.7%) [
61]. The sHLH occurs in 3.7–4.3% of sepsis cases [
15]. Thus, its use in pregnant women in interdisciplinary teams should be carefully considered.
Severe COVID-19 cases may benefit from the IL-6 pathway inhibition, given the associated cytokine release syndrome (CRS) and sHLH-like serum cytokine elevations. The level of inflammatory cytokines and chemokines such as IL-1a/β, IP-10, MCP-1 is increased as well. Severe cases show elevation of TNFα, IL-1, IL-6, IL-18, IL-8, IL-10, MCP-1 and MIP-1A, which can lead to serious pulmonary tissue damage. Additionally, IL-1 has also been linked to the expression of thromboxane-A2 in COVID-19 patients, and as a result, platelet activation and aggregation are increased, which enhances the risk of thrombus development [
63]. Therapeutics based on suppressing CRS, such as tocilizumab, enter clinical trials before they are ready to fight COVID-19 [
20]. The immediate goal of IL-6 antagonism is to ameliorate severe COVID-19 cases so that requirements for advanced care are minimised [
13].
7. Conclusions
The complicated phenomenon of maternal immunological tolerance to foetal antigens enables the development of an antigenically foreign foetus in the uterus despite the existence of the maternal immune system capable of rejection. The maternal immune T-cell profile shifts from the Th1 dominance to the Th2 dominance. Pregnant women are more susceptible to infections, and viral infections may be very dangerous for them. It is important to clarify whether the cytokine storm present in the context of pregnancy promotes the development of HLH.
Pregnant women are more susceptible to infections, and viral infections may be very dangerous for them. The severity of the viral infection may be dependent on existing comorbidities as well (asthma, gestation diabetes, obesity). The severity of COVID-19 disease is an indication for cesarean section because of possible respiratory complications. Even though the mechanism of COVID-19 is not fully understood, a cytokine storm is held accountable for a more severe course of the disease. COVID-19 patients are reported to have frequently shown abnormal laboratory test results indicative of a cytokine storm, including elevated levels of serum ferritin and IL-6, which makes it possible to diagnose HLH as well. The major feature of HLH is hyperferritinaemia, which is also correlated with poor prognosis in COVID-19 patients. SARS-CoV-2 infection can be a trigger of the disorder, but not all patients suffering from COVID-19 develop HLH. The relationship between HLH and COVID-19 involves mortality predictors for COVID-19, used as criteria to diagnose HLH. The HLH disorder is rare and difficult to diagnose; however, its early detection could reduce patient mortality.
This entry is adapted from the peer-reviewed paper 10.3390/biom11081202