Multiple eye pathologies have serious and vision-altering effects that can greatly affect the patients' quality of life. Notably, retinal detachment occurs when the retina, which is the thin layer of tissue at the back of the eye responsible for detecting light and transmitting visual signals to the brain, becomes separated from its underlying supportive layers. This separation can disrupt the normal flow of nutrients and oxygen to the retina, leading to vision loss if not promptly treated. Glaucoma, on the other hand, refers to a group of eye conditions characterized by damage to the optic nerve, which is responsible for transmitting visual information from the eye to the brain. This damage is often associated with increased intraocular pressure (IOP) due to a buildup of fluid within the eye. Glaucoma is typically a progressive condition that can lead to permanent vision loss if left untreated. Finally, myopia is a common vision problem worldwide, and its prevalence has been increasing in recent years, especially in urbanized and highly educated populations. It affects the ability to see distant objects clearly. Suprachoroidal injection thus offers a novel approach to the treatment of these conditions.
- Pharmacological treatments
- SC injection
- Topical administration
- Bioavailability
- Systemic side effects
- Eye disease
- Dose-sparing
- Ophthalmology
Multiple eye pathologies have serious and vision-altering effects that can greatly affect the patients' quality of life. Notably, retinal detachment occurs when the retina, which is the thin layer of tissue at the back of the eye responsible for detecting light and transmitting visual signals to the brain, becomes separated from its underlying supportive layers. This separation can disrupt the normal flow of nutrients and oxygen to the retina, leading to vision loss if not promptly treated. Glaucoma, on the other hand, refers to a group of eye conditions characterized by damage to the optic nerve, which is responsible for transmitting visual information from the eye to the brain. This damage is often associated with increased intraocular pressure (IOP) due to a buildup of fluid within the eye. Glaucoma is typically a progressive condition that can lead to permanent vision loss if left untreated. Finally, myopia is a common vision problem worldwide, and its prevalence has been increasing in recent years, especially in urbanized and highly educated populations. It affects the ability to see distant objects clearly. Suprachoroidal injection thus offers a novel approach to the treatment of these conditions.
1. Retinal Detachment
Suprachoroidal triamcinoline acetonide (SCTA) has shown safety and efficacy in ocular diseases such as macular edema (ME), NIU-associated ME, and DME [166]. Surgical intervention has been the traditional approach for rhegmatogenous RD, but addressing the underlying inflammation is beneficial. Systemic and topical steroids have limitations due to comorbidities and inconsistent drug availability. IV corticosteroids raise IOP and increase cataract risk [166].
To overcome these challenges, SCTA injections have emerged as an alternative. Tabl et al. (2022) conducted a clinical trial using SC injections of SCTA for serous RD in Vogt-Koyanagi disease. Significant improvements in BCVA and central foveal thickness were observed at 1 and 3 months, with no significant difference in IOP [167]. Kohli et al. (2022) demonstrated the success of 4.0 mg SCTA as a preoperative treatment for serous choroidal detachment associated with rhegmatogenous RD, reducing fluid in 50% of eyes by day 3 and 20% by day 5 [166].
While preliminary studies show promise, larger comparative studies are needed to assess long-term outcomes and cost-effectiveness. Research should expand to other types of RD, and longer-term safety studies are necessary to evaluate AEs such as cataract progression and IOP elevation associated with SCTA use.
Studies have investigated non-pharmacological substances injected into the SCS as an alternative to scleral buckling for RD treatment. Gao et al. (2019) explored sodium hyaluronate injection into the SCS, achieving complete reattachment in 50% of eyes [168]. Mittl et al. (1987) demonstrated the short-lived buckling effect of sodium hyaluronate in rabbit models, but its presence in the SCS lasted for 10-14 days [169]. Smith (1952) reported successful retina repositioning with air injection into the SCS but with complications [170].
While sodium hyaluronate injection has shown efficacy in small clinical studies, larger comparative studies are needed to assess its superiority over current treatment alone. Optimization of the formulation for sustained treatment and longer buckling duration is also warranted. Limited follow-up research since 2019 may be due to advancements in SCTA. Further examination of functional and anatomical changes associated with improvements is crucial. Comparative clinical trials comparing SC sodium hyaluronate and SCTA against placebo could lead to improved treatment approaches for various types of RD.
2. Glaucoma
Pharmacological treatments for glaucoma often have low bioavailability when applied topically, requiring multiple daily eye drops and leading to poor adherence and systemic side effects [175-178]. Subconjunctival (SC) injection, with higher drug bioavailability at the ciliary body, has gained interest in glaucoma research. Kim et al. (2014) found that SC injection of Sulprostone and Brimonidine in rabbits reduced intraocular pressure (IOP) by up to 3 mmHg for 9 hours, demonstrating dose-sparing compared to topical administration [179]. Chiang et al. (2016) sustained Brimonidine levels in the SC space using microspheres for 1 month, reducing IOP by 6 mmHg initially and gradually thereafter, with manageable adverse events [180].
To assess the safety and efficacy of SC space for glaucoma treatment, further safety studies involving more animal models and comparisons with standard treatments are necessary. Chiang's study demonstrated the potential for sustained medication levels in the SC space for up to 1 month, highlighting the need for optimizing drug formulations, viscosities, particle suspensions, size, and characteristics for longer-lasting effects. High-viscosity formulations injected into the supraciliary zone minimize diffusion to posterior eye structures, enhancing therapeutic outcomes [180]. Future research should focus on optimizing treatment in the supraciliary zone of the SC space for extended glaucoma therapy.
The potential space between the sclera and choroid can be expanded without long-term adverse effects, as observed in animals and humans [66,173,181]. Chae et al. (2020) demonstrated that subconjunctival (SCS) expansion using an in situ-forming hydrogel reduced intraocular pressure (IOP) in rabbit models for 1 and 4 months, potentially by enhancing aqueous humor drainage through the uveovortex pathway [182] (Figure 1). Minor hemorrhage and fibrosis were observed at the injection site, but no adverse events were reported. Hao et al. (2022) confirmed these findings using a polyzwitterion polycarboxybetaine hydrogel, achieving IOP reduction for 6 weeks with minimal inflammatory reaction and evidence of SCS expansion [183]. SC injection as a non-pharmacological approach shows promising results in animal models, with minor adverse events such as local inflammatory reactions. Clinical trials assessing the safety and efficacy of SCS expansion for glaucoma management in humans have not yet been initiated. If proven safe and effective, combining SCS expansion with SC anti-glaucoma medications could potentially reduce blindness caused by glaucoma.
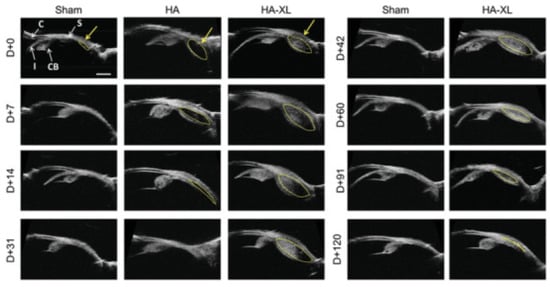
Figure 1. Ultrasound biomicroscopy imaging of hydrogel-injected eyes. Rabbit eyes were injected with Hanks’ Balanced Salt Solution (Sham), commercial hyaluronic acid hydrogel (HA), or in situ-forming hyaluronic acid hydrogel group (HA-XL) and imaged over time. The yellow arrow indicates the approximate injection site, and the yellow dashed line roughly outlines the expanded suprachoroidal space. Images are representative of seven eyes per group (HA-XL group), two eyes per group (Sham), or the only eye available from the HA group. Abbreviations—C: Cornea; CB: Ciliary Body; I: Iris; S: Sclera. D + 0 refers to day zero after injection; D + 7 to 7 days after, etc. Scale bar: 2 mm. Reproduced with permission [182].
3. Myopia
Limited animal and clinical studies exist on the use of subconjunctival (SC) injection for myopia treatment [190]. Venkatesh and Takkar (2017) suggested injecting biological cement into the SCS to address pathological elongation of the eyeball in myopia [190]. Pathological myopia, characterized by excessive axial length, can lead to complications like retinal detachment [14,191]. However, preclinical safety studies are needed before human trials can be initiated. The eye's aqueous environment may limit the therapeutic potential of cement injection, as elevated pressure could cause ocular complications and trauma. Considering the availability of non-invasive and effective myopia treatments like glasses and atropine, there may be limited motivation to explore SC injection for myopia treatment.
