Cervical cancer is the fourth most common malignancy in females worldwide, and a leading cause of death in the United Kingdom (UK). The human papillomavirus (HPV) is the strongest risk factor for developing cervical intraepithelial neoplasia and cancer. Across the UK, the national HPV immunisation programme, introduced in 2008, has been successful in protecting against HPV-related infections. Furthermore, the National Health Service (NHS) implemented the cytology-based cervical cancer screening service to all females aged 25 to 64, which has observed a decline in cervical cancer incidence. In the UK, there has been an overall decline in age-appropriate coverage since April 2010. In 2019, the COVID-19 pandemic disrupted NHS cancer screening and immunisation programmes, leading to a 6.8% decreased uptake of cervical cancer screening from the previous year. Engagement with screening has also been associated with social deprivation. In England, incidence rates of cervical cancer were reported to be 65% higher in the most deprived areas compared to the least, with lifestyle factors such as cigarette consumption contributing to 21% of cervical cancer cases.
- HPV
- cervical cancer
- epidemiology
- risk factors
- cervical cancer screening
- HPV vaccination
1. Epidemiology of Cervical Cancer
2. Introduction of HPV
2.1. HPV Subtypes
2.2. HPV Transmission
3. Pathophysiology of HPV-Related Malignancy
4. Other Risk Factors
4.1. Smoking
4.2. Oral Contraceptive Pill
4.3. Immunosuppression
4.4. Sexual Behavioural Factors
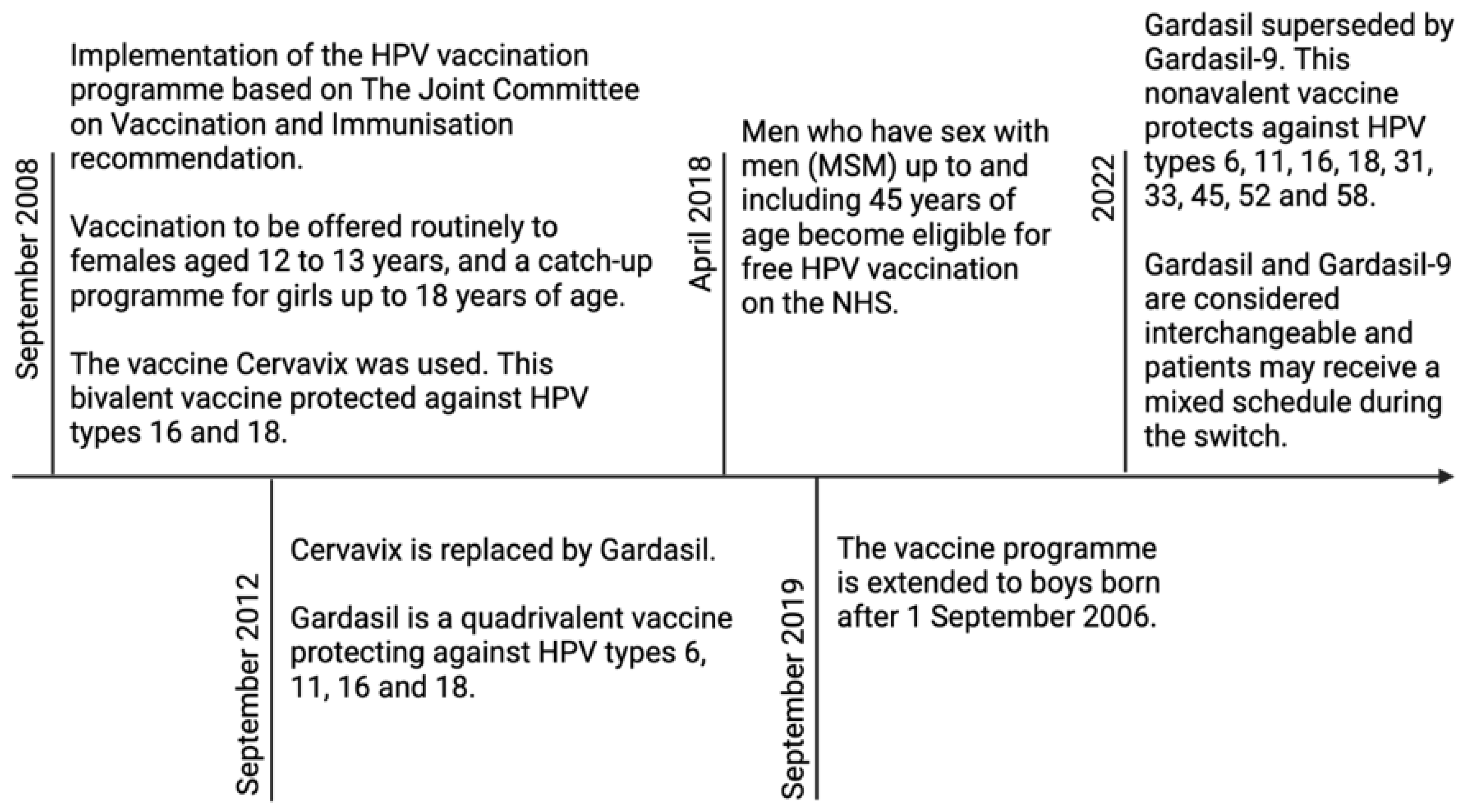
5. Current NHS Programmes—HPV Vaccination
References
- Zhang, S.; Xu, H.; Zhang, L.; Qiao, Y. Cervical cancer: Epidemiology, risk factors and screening. Chin. J. Cancer. Res. 2020, 32, 720–728.
- Green, J.; Berrington de Gonzalez, A.; Sweetland, S.; Beral, V.; Chilvers, C.; Crossley, B.; Deacon, J.; Hermon, C.; Jha, P.; Mant, D.; et al. Risk factors for adenocarcinoma and squamous cell carcinoma of the cervix in women aged 20-44 years: The UK National Case-Control Study of Cervical Cancer. Br. J. Cancer 2003, 89, 2078–2086.
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA. Cancer. J. Clin. 2021, 71, 209–249.
- World Health Organization. Cervical Cancer. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/cervical-cancer (accessed on 9 January 2023).
- Pesola, F.; Sasieni, P. Impact of screening on cervical cancer incidence in England: A time trend analysis. BMJ. Open. 2019, 9, e026292.
- Cervical Cancer Incidence Statistics. Cancer Research UK. 2015. Available online: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer/incidence (accessed on 19 December 2022).
- Tota, J.; Franco, E.L. Effectiveness of cervical cancer screening at different ages. Womens Health 2009, 5, 613–616.
- Cervical Screening: Programme Overview. GOV.UK. 2021. Available online: https://www.gov.uk/guidance/cervical-screening-programme-overview (accessed on 31 December 2022).
- Mendes, D.; Mesher, D.; Pista, A.; Baguelin, M.; Jit, M. Understanding differences in cervical cancer incidence in Western Europe: Comparing Portugal and England. Eur. J. Public Health 2018, 28, 343–347.
- Schiffman, M.H.; Castle, P. Epidemiologic Studies of a Necessary Causal Risk Factor: Human Papillomavirus Infection and Cervical Neoplasia. J. Natl. Cancer. Inst. 2003, 95, E2.
- Mesher, D.; Cuschieri, K.; Hibbitts, S.; Jamison, J.; Sargent, A.; Pollock, K.G.; Powell, N.; Wilson, R.; McCall, F.; Fiander, A.; et al. Type-specific HPV prevalence in invasive cervical cancer in the UK prior to national HPV immunisation programme: Baseline for monitoring the effects of immunisation. J. Clin. Pathol. 2015, 68, 135–140.
- Wang, X.; Huang, X.; Zhang, Y. Involvement of Human Papillomaviruses in Cervical Cancer. Front. Microbiol. 2018, 9, 2896.
- Dempsey, A.F. Human Papillomavirus: The Usefulness of Risk Factors in Determining Who Should Get Vaccinated. Rev. Obstet. Gynecol. 2008, 1, 122–128.
- Jayasinghe, Y.; Garland, S.M. Genital warts in children: What do they mean? Arch. Dis. Child. 2006, 91, 696–700.
- World Health Organization. Cervical Cancer Elimination Initiative. 2022. Available online: https://www.who.int/initiatives/cervical-cancer-elimination-initiative (accessed on 9 January 2023).
- Graham, S. Human papillomavirus: Gene expression, regulation and prospects for novel diagnostic methods and antiviral therapies. Future. Microbiol. 2010, 5, 1493–1506.
- Jendoubi-Ferchichi, M.; Satouri, L.; Ghoul, F.; Malek-Mellouli, M.; Derbel, A.M.; Makni, M.K.; Reziga, H.; Baba, A.; Zili, M.; Segondy, M.; et al. Phylogeny and Classification of Human Papillomavirus (HPV)16 and HPV18 Variants Based on E6 and L1 genes in Tunisian Women with Cervical Lesions. Asian Pac. J. Cancer Prev. 2018, 19, 3361–3366.
- Williams, V.M.; Filippova, M.; Soto, U.; Duerksen-Hughes, P.J. HPV-DNA integration and carcinogenesis: Putative roles for inflammation and oxidative stress. Future Virol. 2011, 6, 45–57.
- Burd, E.M. Human Papillomavirus and Cervical Cancer. Clin. Microbiol. Rev. 2003, 16, 1–17.
- Petca, A.; Borislavschi, A.; Zvanca, M.E.; Petca, R.C.; Sandru, F.; Dumitrascu, M.C. Non-sexual HPV transmission and role of vaccination for a better future (Review). Exp. Ther. Med. 2020, 20, 186.
- Manini, I.; Montomoli, E. Epidemiology and prevention of Human Papillomavirus. Ann. Ig. 2018, 30, 28–32.
- Sabeena, S.; Bhat, P.; Kamath, V.; Arunkumar, G. Possible non-sexual modes of transmission of human papilloma virus. J. Obstet. Gynaecol. Res. 2017, 43, 429–435.
- Louie, K.S.; de Sanjose, S.; Diaz, M.; Castellsagué, X.; Herrero, R.; Meijer, C.J.; Shah, K.; Franceschi, S.; Muñoz, N.; Bosch, F.X.; et al. Early age at first sexual intercourse and early pregnancy are risk factors for cervical cancer in developing countries. Br. J. Cancer 2009, 100, 1191–1197.
- Liu, Z.C.; Liu, W.D.; Liu, Y.H.; Ye, X.H.; Chen, S.D. Multiple Sexual Partners as a Potential Independent Risk Factor for Cervical Cancer: A Meta-analysis of Epidemiological Studies. Asian Pac. J. Cancer Prev. 2015, 16, 3893–3900.
- Chesson, H.W.; Dunne, E.F.; Hariri, S.; Markowitz, L.E. The Estimated Lifetime Probability of Acquiring Human Papillomavirus in the United States. Sex. Transm. Dis. 2014, 41, 660–664.
- Dugué, P.A.; Rebolj, M.; Hallas, J.; Garred, P.; Lynge, E. Risk of cervical cancer in women with autoimmune diseases, in relation with their use of immunosuppressants and screening: Population-based cohort study. Int. J. Cancer 2015, 136, E711–E719.
- Balasubramaniam, S.D.; Balakrishnan, V.; Oon, C.E.; Kaur, G. Key Molecular Events in Cervical Cancer Development. Medicina 2019, 55, 384.
- Song, D.; Li, H.; Li, H.; Dai, J. Effect of human papillomavirus infection on the immune system and its role in the course of cervical cancer. Oncol. Lett. 2015, 10, 600–606.
- Horvath, C.A.; Boulet, G.A.; Renoux, V.M.; Delvenne, P.O.; Bogers, J.P.J. Mechanisms of cell entry by human papillomaviruses: An overview. Virol. J. 2010, 7, 11.
- Richards, R.M.; Lowy, D.R.; Schiller, J.T.; Day, P.M. Cleavage of the papillomavirus minor capsid protein, L2, at a furin consensus site is necessary for infection. Proc. Natl. Acad. Sci. USA 2006, 103, 1522–1527.
- Crosbie, E.J.; Einstein, M.H.; Franceschi, S.; Kitchener, H.C. Human papillomavirus and cervical cancer. Lancet 2013, 382, 889–899.
- Shimada, M.; Yamashita, A.; Saito, M.; Ichino, M.; Kinjo, T.; Mizuki, N.; Klinman, D.M.; Okuda, K. The human papillomavirus E6 protein targets apoptosis-inducing factor (AIF) for degradation. Sci. Rep. 2020, 10, 14195.
- White, E.A.; Münger, K.; Howley, P.M. High-Risk Human Papillomavirus E7 Proteins Target PTPN14 for Degradation. mBio 2016, 7, e01530-16.
- Venuti, A.; Paolini, F.; Nasir, L.; Corteggio, A.; Roperto, S.; Campo, M.S.; Borzacchiello, G. Papillomavirus E5: The smallest oncoprotein with many functions. Mol. Cancer 2011, 10, 140.
- Graham, S.V. The human papillomavirus replication cycle, and its links to cancer progression: A comprehensive review. Clin. Sci. 2017, 131, 2201–2221.
- Fay, N.; Panté, N. Nuclear entry of DNA viruses. Front. Microbiol. 2015, 6, 467.
- Wang, J.W.; Roden, R.B.S. Virus-like particles for the prevention of human papillomavirus-associated malignancies. Expert. Rev. Vaccines 2013, 12, 129–141.
- Kirnbauer, R.; Booy, F.; Cheng, N.; Lowy, D.R.; Schiller, J.T. Papillomavirus L1 major capsid protein self-assembles into virus-like particles that are highly immunogenic. Proc. Natl. Acad. Sci. USA 1992, 89, 12180–12184.
- International Collaboration of Epidemiological Studies of Cervical Cancer; Appleby, P.; Beral, V.; Berrington de González, A.; Colin, D.; Franceschi, S.; Goodhill, A.; Green, J.; Peto, J.; Plummer, M.; et al. Carcinoma of the cervix and tobacco smoking: Collaborative reanalysis of individual data on 13,541 women with carcinoma of the cervix and 23,017 women without carcinoma of the cervix from 23 epidemiological studies. Int. J. Cancer 2006, 118, 1481–1495.
- Roura, E.; Castellsagué, X.; Pawlita, M.; Travier, N.; Waterboer, T.; Margall, N.; Bosch, F.X.; de Sanjosé, S.; Dillner, J.; Gram, I.T.; et al. Smoking as a major risk factor for cervical cancer and pre-cancer: Results from the EPIC cohort. Int. J. Cancer 2014, 135, 453–466.
- Vaccarella, S.; Herrero, R.; Snijders, P.J.; Dai, M.; Thomas, J.O.; Hieu, N.T.; Ferreccio, C.; Matos, E.; Posso, H.; de Sanjosé, S.; et al. IARC HPV Prevalence Surveys (IHPS) Study Group. Smoking and human papillomavirus infection: Pooled analysis of the International Agency for Research on Cancer HPV Prevalence Surveys. Int. J. Epidemiol. 2008, 37, 536–546.
- Xi, L.F.; Koutsky, L.A.; Castle, P.E.; Edelstein, Z.R.; Meyers, C.; Ho, J.; Schiffman, M. Relationship between cigarette smoking and human papillomavirus type 16 and 18 DNA load. Cancer. Epidemiol. Biomark. Prev. 2009, 18, 3490–3496.
- Koshiol, J.; Schroeder, J.; Jamieson, D.J.; Marshall, S.W.; Duerr, A.; Heilig, C.M.; Shah, K.V.; Klein, R.S.; Cu-Uvin, S.; Schuman, P.; et al. Smoking and Time to Clearance of Human Papillomavirus Infection in HIV-Seropositive and HIV-Seronegative Women. Am. J. Epidemiol. 2006, 164, 176–183.
- Alam, S.; Conway, M.J.; Chen, H.S.; Meyers, C. The Cigarette Smoke Carcinogen Benzopyrene Enhances Human Papillomavirus Synthesis. J. Virol. 2008, 82, 1053–1058.
- Wei, L.; Griego, A.M.; Chu, M.; Ozbun, M.A. Tobacco exposure results in increased E6 and E7 oncogene expression, DNA damage and mutation rates in cells maintaining episomal human papillomavirus 16 genomes. Carcinogenesis 2014, 35, 2373–2381.
- Alam, S.; Bowser, B.S.; Conway, M.J.; Israr, M.; Ryndock, E.J.; Xi, L.F.; Meyers, C. Downregulation of Cdc2/CDK1 kinase activity induces the synthesis of noninfectious human papillomavirus type 31b virions in organotypic tissues exposed to benzopyrene. J. Virol. 2010, 84, 4630–4645.
- Combined Pill. Your Contraception Guide. nhs.uk. 2020. Available online: https://www.nhs.uk/conditions/contraception/combined-contraceptive-pill/ (accessed on 10 January 2023).
- National Institute for Health and Care Excellence. Contraception—Combined Hormonal Methods: Scenario: Combined Oral Contraceptive. 2022. Available online: https://cks.nice.org.uk/topics/contraception-combined-hormonal-methods/management/combined-oral-contraceptive/ (accessed on 20 December 2022).
- Asthana, S.; Busa, V.; Labani, S. Oral contraceptives use and risk of cervical cancer-A systematic review & meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 247, 163–175.
- Peng, Y.; Wang, X.; Feng, H.; Yan, G. Is oral contraceptive use associated with an increased risk of cervical cancer? An evidence-based meta-analysis. J. Obstet. Gynaecol. Res. 2017, 43, 913–922.
- Anastasiou, E.; McCarthy, K.J.; Gollub, E.L.; Ralph, L.; van de Wijgert, J.H.H.M.; Jones, H.E. The relationship between hormonal contraception and cervical dysplasia/cancer controlling for human papillomavirus infection: A systematic review. Contraception 2022, 107, 1–9.
- International Collaboration of Epidemiological Studies of Cervical Cancer; Appleby, P.; Beral, V.; Berrington de González, A.; Colin, D.; Franceschi, S.; Goodhill, A.; Green, J.; Peto, J.; Plummer, M.; et al. Cervical cancer and hormonal contraceptives: Collaborative reanalysis of individual data for 16,573 women with cervical cancer and 35,509 women without cervical cancer from 24 epidemiological studies. Lancet 2007, 370, 1609–1621.
- Roura, E.; Travier, N.; Waterboer, T.; de Sanjosé, S.; Bosch, F.X.; Pawlita, M.; Pala, V.; Weiderpass, E.; Margall, N.; Dillner, J.; et al. The Influence of Hormonal Factors on the Risk of Developing Cervical Cancer and Pre-Cancer: Results from the EPIC Cohort. PLoS. ONE 2016, 11, e0147029.
- Ramachandran, B. Functional association of oestrogen receptors with HPV infection in cervical carcinogenesis. Endocr. Relat. Cancer 2017, 24, R99–R108.
- Munk, A.C.; Gudlaugsson, E.; Ovestad, I.T.; Lovslett, K.; Fiane, B.; Hidle, B.v.; Kruse, A.J.; Skaland, I.; Janssen, E.A.; Baak, J.P. Interaction of epithelial biomarkers, local immune response and condom use in cervical intraepithelial neoplasia 2-3 regression. Gynecol. Oncol. 2012, 127, 489–494.
- Hogewoning, C.J.; Bleeker, M.C.; van den Brule, A.J.; Voorhorst, F.J.; Snijders, P.J.; Berkhof, J.; Westenend, P.J.; Meijer, C.J. Condom use promotes regression of cervical intraepithelial neoplasia and clearance of human papillomavirus: A randomized clinical trial. Int. J. Cancer 2003, 107, 811–816.
- Winer, R.L.; Hughes, J.P.; Feng, Q.; O’Reilly, S.; Kiviat, N.B.; Holmes, K.K.; Koutsky, L.A. Condom use and the risk of genital human papillomavirus infection in young women. N. Engl. J. Med. 2006, 354, 2645–2654.
- Moreno, V.; Bosch, F.X.; Muñoz, N.; Meijer, C.J.; Shah, K.V.; Walboomers, J.M.; Herrero, R.; Franceschi, S.; International Agency for Research on Cancer. Multicentric Cervical Cancer Study Group. Effect of oral contraceptives on risk of cervical cancer in women with human papillomavirus infection: The IARC multicentric case-control study. Lancet 2002, 359, 1085–1092.
- Grulich, A.E.; van Leeuwen, M.T.; Falster, M.O.; Vajdic, C.M. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: A meta-analysis. Lancet 2007, 370, 59–67.
- Dugué, P.A.; Rebolj, M.; Garred, P.; Lynge, E. Immunosuppression and risk of cervical cancer. Expert. Rev. Anticancer. Ther. 2013, 13, 29–42.
- Hinten, F.; Meeuwis, K.A.; van Rossum, M.M.; de Hullu, J.A. HPV-related (pre)malignancies of the female anogenital tract in renal transplant recipients. Crit. Rev. Oncol. Hematol. 2012, 84, 161–180.
- Meeuwis, K.A.; van Rossum, M.M.; van de Kerkhof, P.C.; Hoitsma, A.J.; Massuger, L.F.; de Hullu, J.A. Skin cancer and (pre)malignancies of the female genital tract in renal transplant recipients. Transpl. Int. 2010, 23, 191–199.
- Klitzke, S.; Wender, I.O.; Salcedo, M.P.; Pessini, S.A. Cervical cancer screening abnormalities in immunosuppressed renal transplant women: Case-control study in Southern Brazil. Arch. Gynecol. Obstet. 2020, 302, 649–655.
- Chen, M.; Cui, Q.; Chen, M.; Xia, M.; Liu, D.; Chen, P.; Wang, C.; He, M. Risk of human papillomavirus infection and cervical intraepithelial lesions in Chinese renal transplant recipients. Front. Oncol. 2022, 12, 905548.
- Stelzle, D.; Tanaka, L.F.; Lee, K.K.; Ibrahim Khalil, A.; Baussano, I.; Shah, A.S.V.; McAllister, D.A.; Gottlieb, S.L.; Klug, S.J.; Winkler, A.S.; et al. Estimates of the global burden of cervical cancer associated with HIV. Lancet. Glob. Health 2021, 9, e161–e169.
- Massad, L.S.; Seaberg, E.C.; Wright, R.L.; Darragh, T.; Lee, Y.C.; Colie, C.; Burk, R.; Strickler, H.D.; Watts, D.H. Squamous cervical lesions in women with human immunodeficiency virus: Long-term follow-up. Obstet. Gynecol. 2008, 111, 1388–1393.
- Abraham, A.G.; D’Souza, G.; Jing, Y.; Gange, S.J.; Sterling, T.R.; Silverberg, M.J.; Saag, M.S.; Rourke, S.B.; Rachlis, A.; Napravnik, S.; et al. Invasive Cervical Cancer Risk Among HIV-Infected Women: A North American multicohort collaboration prospective study. J. Acquir. Immune. Defic. Syndr. 2013, 62, 405–413.
- Cervical Screening: Scenario: Cervical Screening. National Institute for Health and Care Excellence. 2022. Available online: https://cks.nice.org.uk/topics/cervical-screening/management/cervical-screening/ (accessed on 23 December 2022).
- International Collaboration of Epidemiological Studies of Cervical Cancer. Cervical carcinoma and sexual behavior: Collaborative reanalysis of individual data on 15,461 women with cervical carcinoma and 29,164 women without cervical carcinoma from 21 epidemiological studies. Cancer. Epidemiol. Biomarkers. Prev. 2009, 18, 1060–1069.
- Children and the Law. NSPCC Learning. 2022. Available online: https://learning.nspcc.org.uk/child-protection-system/children-the-law/ (accessed on 8 January 2023).
- Quabius, E.S.; Fazel, A.; Knieling, C.; Gebhardt, S.; Laudien, M.; Moore, C.; Kühnel, A.; Hoppe, F.; Mlynski, R.; Heinrichs, A.; et al. No association between HPV-status in tonsillar tissue and sexual behavior of the patients in a northern German population—Critical view of the link between HPV natural history and HPV-driven carcinogenesis. Papillomavirus. Res. 2020, 10, 100207.
- HPV Vaccine Overview. nhs.uk. 2019. Available online: https://www.nhs.uk/conditions/vaccinations/hpv-human-papillomavirus-vaccine/ (accessed on 8 January 2023).
- Bogaards, J.A.; Wallinga, J.; Brakenhoff, R.H.; Meijer, C.J.; Berkhof, J. Direct benefit of vaccinating boys along with girls against oncogenic human papillomavirus: Bayesian evidence synthesis. BMJ 2015, 350, h2016.
- HPV Vaccination Recommendations. Centers for Disease Control and Prevention. 2021. Available online: https://www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html (accessed on 10 January 2023).
- HPV Vaccine to Change in September 2012. GOV.UK. 2011. Available online: https://www.gov.uk/government/news/hpv-vaccine-to-change-in-september-2012 (accessed on 10 January 2023).
- Information on HPV Vaccination. GOV.UK. 2022. Available online: https://www.gov.uk/government/publications/hpv-vaccine-vaccination-guide-leaflet/information-on-hpv-vaccination (accessed on 10 January 2023).
- Joura, E.A.; Giuliano, A.R.; Iversen, O.E.; Bouchard, C.; Mao, C.; Mehlsen, J.; Moreira, E.D., Jr.; Ngan, Y.; Petersen, L.K.; Lazcano-Ponce, E.; et al. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. N. Engl. J. Med. 2015, 372, 711–723.
- Joura, E.A.; Garland, S.M.; Paavonen, J.; Ferris, D.G.; Perez, G.; Ault, K.A.; Huh, W.K.; Sings, H.L.; James, M.K.; Haupt, R.M.; et al. Effect of the human papillomavirus (HPV) quadrivalent vaccine in a subgroup of women with cervical and vulvar disease: Retrospective pooled analysis of trial data. BMJ 2012, 344, e1401.
- Human Papillomavirus (HPV): The Green Book, Chapter 18a. GOV.UK. 2022. Available online: https://www.gov.uk/government/publications/human-papillomavirus-hpv-the-green-book-chapter-18a (accessed on 10 January 2023).
- Shi, L.; Sings, H.L.; Bryan, J.T.; Wang, B.; Wang, Y.; Mach, H.; Kosinski, M.; Washabaugh, M.W.; Sitrin, R.; Barr, E. GARDASIL: Prophylactic human papillomavirus vaccine development--from bench top to bed-side. Clin. Pharmacol. Ther. 2007, 81, 259–264.
- Artemchuk, H.; Eriksson, T.; Poljak, M.; Surcel, H.M.; Dillner, J.; Lehtinen, M.; Faust, H. Long-term Antibody Response to Human Papillomavirus Vaccines: Up to 12 Years of Follow-up in the Finnish Maternity Cohort. J. Infect. Dis. 2019, 219, 582–589.
- Hoes, J.; Pasmans, H.; Schurink-van ’t Klooster, T.M.; van der Klis, F.R.M.; Donken, R.; Berkhof, J.; de Melker, H.E. Review of long-term immunogenicity following HPV vaccination: Gaps in current knowledge. Hum. Vaccin. Immunother. 2022, 18, 1908059.
- Petry, K.U.; Bollaerts, K.; Bonanni, P.; Stanley, M.; Drury, R.; Joura, E.; Kjaer, S.K.; Meijer, C.J.L.M.; Riethmuller, D.; Soubeyrand, B.; et al. Estimation of the individual residual risk of cervical cancer after vaccination with the nonavalent HPV vaccine. Hum. Vaccin. Immunother. 2018, 14, 1800–1806.
- Lei, J.; Ploner, A.; Elfström, K.M.; Wang, J.; Roth, A.; Fang, F.; Sundström, K.; Dillner, J.; Sparén, P. HPV Vaccination and the Risk of Invasive Cervical Cancer. N. Engl. J. Med. 2020, 383, 1340–1348.
