Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Isoflavones have gained popularity as an alternative treatment for menopausal symptoms for people who cannot or are unwilling to take hormone replacement therapy.
- isoflavone
- daidzein
- genistein
- equol
- menopause
1. Introduction
Menopause is a biological process that can cause various troublesome symptoms such as hot flashes and emotional changes, but can also increase mortality risk due to subsequent osteoporosis and reduced metabolism. Hormone replacement therapy (HRT) would be the most intuitive way to combat these changes; however, the 2002 Women’s Health Initiative (WHI) study showed that hormone replacement therapy increased the risk of breast cancer, stroke, and coronary heart disease in healthy postmenopausal women [1]. Since then, healthcare professionals and women have been seeking alternative therapies. In Canada for example, it has been found that 60% to 90% of women would consider taking complementary and/or alternative medicine (CAM) for menopausal symptoms, but are concerned about the efficacy and cost [2]. Many patients taking CAM choose not to tell their doctors because they feel doctors are not knowledgeable enough or are biased against CAM [3].
Vasomotor symptoms (VMS) such as hot flushes and sweating, are very common in menopausal populations and can cause physical and mental discomfort [4]. Estrogen remains the most effective therapy for hot flashes and is approved by the U.S. Food and Drug Administration (FDA) [5]. Although some women may prefer lifestyle modification, there is no evidence that lowering the room temperature, exercising, or avoiding triggers such as alcohol and spicy foods can improve hot flashes [5]. Currently, HRT is indicated for the prevention of osteoporosis and relief of the VMS and vulvovaginal atrophy associated with menopause. Moreover, HRT increases bone mineral density (BMD) and reduces the incidence of osteoporotic fractures [6]. Due to the serious side effects mentioned above, HRT should be given in the lowest effective doses for the shortest duration to meet the treatment goals. In fact, the FDA recommends that approved non-estrogen treatments can first be carefully considered before relying solely on HRT for osteoporosis prevention [7]. VMS seriously affects quality of life during menopause and the role of HRT is still fundamental. For affected women who cannot use HRT, evidence has shown that acupuncture, hypnosis, paced respiration, cognitive behavioral therapy, combined preparations of black cohosh, and omega-3 supplements may significantly reduce vasomotor symptoms [4].
2. Terminology
2.1. Isoflavones (Genistin, Daidzin), Genistein, Daidzein
The terms phytoestrogens (or plant estrogens), isoflavones, and soy are often used interchangeably in the literature, but they are not the same. More accurately, phytoestrogens are plant compounds that have estrogen-like effects and isoflavones such as genistin and daidzin are a type of bioflavonoids that are found in both plants and animals [8]. Isoflavones are abundant in foods including soybeans, red clover, and alfalfa. After isoflavone metabolization in the human gut, the precursors genistin and daidzin become the “aglycones” genistein and daidzein, respectively, through the effect of gastrointestinal enzymes [9] (Figure 1). Fermentation of soybeans (e.g., to make miso) concentrates isoflavones, while processing methods that remove fat, taste, and color tend to remove isoflavones [10].
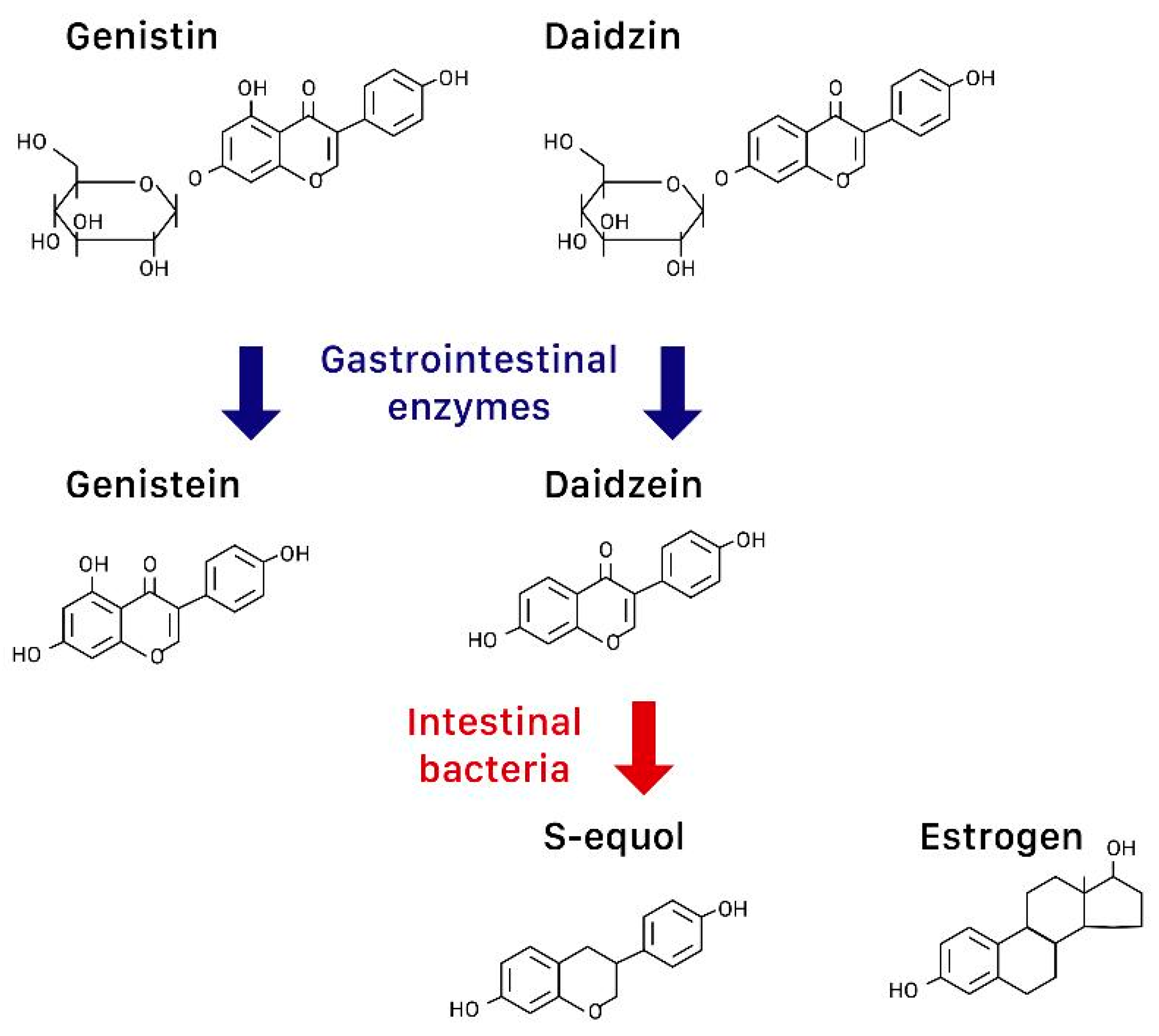
Figure 1. The chemical structures of genistein and its precursor genistin, daidzein and its precursor daidzin, s-equol, and estrogen.
2.2. Equol
In over 50% of Asians but less than 20% of Caucasians, their intestinal bacteria can further convert daidzein to S-equol, a compound structurally similar to estrogen [11] (Figure 1). S-equol also preferentially binds to ERβ, but has a higher transcriptional expression than isoflavones [10].
Research has found that for non-equol producers, even if they consume adequate daidzein, the efficacy of alleviating menopausal symptoms may still be limited [11]. In an observational study of 364 women, only equol-producers benefited from dietary daidzein in reducing vasomotor symptoms [12]. Ingesting probiotics has failed to stimulate S-equol production in some studies [13], while a recent randomized controlled trial (RCT) showed red clover extract with probiotics effectively reduced VMS [14]. From fecal cultures of equol-producing women, equol-producing bacteria such as Lactococcus garvieae has been isolated [13][15], and a Japanese RCT showed that equol supplementation in non-equol producers successfully alleviated mood-related symptoms [16].
3. Effects of Isoflavones on Menopausal Syndromes and Others
3.1. Hot Flashes
VMS (hot flashes and night sweats) are perhaps the most immediate and troublesome consequence of menopause, and one of the main reasons menopausal women seek medical help. However, as the frequency and severity of hot flashes are subjective and symptoms often resolve over time without treatment [9], VMS are difficult to quantify. A placebo effect is unavoidable, as illustrated in the 24-week study done by St. Germain et al. in 2001, which showed hot flash decline in all patients, whether they received isoflavone-rich soy, isoflavone-poor soy, or whey protein [17]. Tice et al. also found no difference in the frequency of hot flash after 12 weeks of treatment with either isoflavones or placebo [18].
In order to minimize subjectivity of the frequency and severity of hot flashes, skin conductance measurement has been used in some studies. Skin conductance quantifies the preceding small increase in core body temperature and subsequent sweat response [14]. Although Newton et al. found consistent results whether using a diary or a sternal skin conductance monitor [12], Lambert et al. found differences between subjective reporting of hot flashes using the Green Climacteric Scale and measuring hot flashes using 24 h ambulatory skin conductance [14]. In their study, red clover extract and probiotics significantly reduced hot flashes using the measurement of skin conductance but not Green Climacteric Scale, highlighting the need for an objective measure [14].
3.2. Bone Mineral Density
Another significant change that occurs during menopause is the loss of bone mineral density (BMD), causing osteoporosis. As there are high levels of ERβ in bone [8], isoflavones could theoretically prevent bone loss. Previous research has focused on ipriflavone, a synthetic isoflavone, but results have been inconclusive [9].
The spine in particular is thought to be the most sensitive to isoflavones because it has a higher content of trabecular bone compared to cortical bone. Trabecular bone has a higher expression of ERβ and a larger surface area for receptor binding [19]. The hip, on the other hand, contains a higher percentage of cortical bone, and is remodeled slower than the spine [20]. A meta-analysis showed significant attenuation of spinal bone loss after 6 months of over 90 mg/day of isoflavone supplement [20]. Amato et al. found that while 120 mg of isoflavones per day did not slow bone loss at regional bone sites, there was slowing of BMD loss [21]. A systematic review and meta-analysis published in 2017 reiterated that isoflavones attenuated BMD loss, but more so at the lumbar spine compared to the femoral neck, and isoflavones in aglycone form were more efficacious [19].
As bone remodeling takes around four to eight months, studies of longer duration could help elucidate more conclusive results [19]. In the meantime, even slight improvements in BMD may be beneficial for postmenopausal women who are not on hormone replacement therapy [9].
3.3. Cardiovascular Profile
Although there are many independent cardiovascular risks including age, the incidence of cardiovascular events in women also increases after menopause due to estrogen deficiency [22]. The lack of estrogen leads to a rise in low-density lipoprotein (LDL) cholesterol, endothelial dysfunction, and reduced carotid arterial pulsatility [23]. Isoflavones may be able to reduce cardiovascular risk by acting as estrogen substitutes.
As soy products do not contain cholesterol, they are generally regarded as healthy food, leading the United States Food and Drug Administration (FDA) to issue a statement saying soy protein may reduce the risk of heart disease [9]. However, habitual intake of soy in Western countries is low. A Dutch prospective study of 16,165 women followed up for a median of 75 months found no correlation between habitual phytoestrogen intake (including lignans and isoflavones) of the Western diet and cardiovascular disease risk, possibly due to the low overall isoflavone intake [22].
The mechanism of isoflavones in preventing cardiovascular events, if any, remains to be elucidated. Previous small-scale research has suggested that in perimenopausal and menopausal women, soy isoflavones may improve systemic arterial compliance, although they had no effect on plasma lipids [23]. A 2007 study similarly showed no difference in lipoprotein lipids after 12 weeks of treatment with 60 mg of isoflavones daily [24]. Therefore, isoflavones may exert their cardioprotective effects in ways other than lowering lipids [25].
It has been suggested that genistein and daidzein cause arterial relaxation through the release of nitric oxide [25]. However, Wong et al. found that 80 mg of soy isoflavones per day for six weeks had no significant effect on blood pressure [26]. In fact, in vessels with pre-existing atherosclerotic changes, animal studies have shown detrimental effects of soy and HRT. In ovariectomized and diet-induced atherosclerotic monkeys, neither soy nor HRT reduced myocardial ischemia/reperfusion injury, and the combination of both actually increased post-ischemic myocardial change [27]. Animal studies must be interpreted with caution however, and further research is required to reach a conclusion before advising women against consuming soy products once they experience a coronary event [25].
A recent RCT revealed that soy isoflavones reduce systolic blood pressure in early menopause. In women within two years of menopause, Sathyapalan et al. found that treatment with soy isoflavone supplements for six months reduced systolic blood pressure, though there were no changes in diastolic blood pressure or lipid parameters (total cholesterol, LDL, HDL, and triglycerides) [28]. The reduction in systolic blood pressure translated into reduced risk of cardiovascular disease using the Framingham equation [28]. According to the above findings, one can infer that the safest and most effective treatment window for cardiovascular disease would be early menopause, before critical atherosclerotic change.
It is also possible that isoflavones only play a small role in preventing cardiovascular events, and that the main benefits seen are from soy itself. Soy, in contrast to animal protein, contains minimal cholesterol and saturated fats [9], making it a more healthy way to meet daily protein requirements. Therefore, whether it is due to soy containing copious amounts of polyunsaturated fats, fiber, and vitamins [29], or simply because it displaces dietary animal protein intake [10], soy products are currently recommended by both the FDA and AHA (American Heart Association) for the benefit of cardiovascular and overall health [9][29].
3.4. Metabolic Syndrome
The slowing of metabolism after menopause leads to obesity, an important risk factor of cardiovascular diseases [29]. There has been evidence to suggest that isoflavones improve glycemic control and promote weight loss [30].
In obese menopausal women, research on the relationship of soy isoflavone supplement and weight loss has been limited. In a study that showed isoflavone and exercise led to a reduction of fat mass, the high drop-out rate and questionable compliance to treatment made interpretation of results difficult [29].
In vitro studies are more optimistic. Genistein, daidzein, and equol show binding affinity to and activation of peroxisome proliferator-activated receptor (PPAR)γ, a drug target for type 2 diabetes and other components of metabolic syndrome [30]. Compared to rosiglitazone, an established anti-diabetic drug, the maximal PPARγ activity of isoflavones ranged from 23% to 32% [30]. As red clover extracts do not cause weight gain like rosiglitazone does in human studies [30], isoflavones could potentially be used to treat metabolic syndrome through glycemic control without the side effect of weight gain.
3.5. Cancer Risk
Because isoflavones bind to estrogen receptors, there has been concern of isoflavones inducing estrogen-sensitive malignancies, particularly in women who are at high risk or survivors of breast cancer [29]. However, in vitro studies have shown that breast cancer proliferation is dependent on increased ERα activity, and ERβ seems to suppress ERα-induced cancer cell proliferation [31]. Therefore, it is postulated that isoflavones, by binding to ERβ, is cancer-protective. In addition, phytoestrogens have been found to lengthen the menstrual cycle, a possible mechanism that potentially protects against hormone-dependent cancers [9]. However, such a mechanism has not been demonstrated yet.
In studies with healthy women, isoflavones were associated with a decreased risk of estrogen-sensitive cancer. A case-control study in Japan found that the risk of breast cancer was inversely related to soy consumption in premenopausal women, but found no link in postmenopausal women [32]. Although soy isoflavones induced some benign clinical and non-significant ultrasonographic changes of the breast in one 12-week study, none of these changes warranted intervention or follow-up for at least three months after the study [33]. On the other hand, soy isoflavones did not seem to stimulate endometrial proliferation during short-term treatment [10]. On the contrary, a study conducted by Shike et al. has explored the effects of soy supplementation on gene expression in breast cancer. In this RCT, the authors found that gene expression associated with soy intake and high plasma genistein defines a signature characterized by overexpression of FGFR2 and genes that drive cell cycle and proliferation pathways. Therefore, they concluded that in a subset of women soy could adversely affect gene expression in breast cancer [34].
The limited research on breast cancer patients taking soy isoflavones after surgery has also been promising. Kang et al. found that in postmenopausal women with estrogen- and progesterone-receptor positive breast cancers receiving anastrazole therapy after surgery, a higher intake of soy isoflavone was associated with a lower risk of recurrence [35].
Finally, isoflavones have also been suggested to protect against colon cancer. Risk factors for colon cancer include obesity, high levels of cholesterol, and type 2 diabetes, all of which isoflavones potentially treat. Therefore, stating that isoflavones prevent colon cancer would be a reasonable hypothesis. A study in Korea found that high intake of soy foods or isoflavones was associated with an overall reduction of risk in colorectal cancer, although high intake of fermented soy paste seemed to increase the risk of colorectal cancer in men, possibly due to the high salt content [36]. Further research is required to increase the validity of this hypothesis. Soy fibers may also play a role is this prevention. A future comparison of soy vs. isoflavone rich extracts should highlight whether or not this is the case.
3.6. Female Urogenital Tract
Estrogen has been used to treat vaginal dryness and incontinence with varying degrees of success. ERα and ERβ have been identified in urogenital tissues (including bladder, urethra, levator ani, and vaginal mucosa) variably [37]. These tissues also contain the GPER that has a great affinity for genistein and daidzein, and the mechanism of continence remains unknown. Isoflavone treatment has been trialed on menopausal symptoms affecting the urogenital tract.
Reed et al. found no differences in the vaginal cytology of women taking black cohosh or dietary soy after one year [38], though the isoflavone content of the supplements was not clearly stated. A 10-year longitudinal study found that neither high nor low dietary isoflavone intake prevented stress or urge incontinence [37], though they did not take into account equol-producer status.
Burton and Wells pointed out in their study investigating phytoestrogens and the female genital tract that although there is no concrete evidence to date to suggest phytoestrogens affect the human female genital tract, this is due to the paucity of research rather than the lack of correlation, and urge further investigation into this matter [39].
Regarding the effects of nutraceuticals on the sexual function of menopausal women, one study was identified. This prospective, randomized, placebo-controlled, parallel-group study was conducted to evaluate the effect of a mixture of isoflavones, calcium vitamin D, and inulin in menopausal women. Before and after treatment, both the patients in the treatment group (taking oral preparations of isoflavones (40 mg), calcium (500 mg) vitamin D (300 UI) plus inulin (3 g)) and the control group (taking placebo) were assessed for quality of life and sexual function using the Menopause-Specific Quality of Life Questionnaire (MENQOL) and Female Sexual Function Index (FSFI) [40]. A significant reduction in MENQOL vasomotor, physical, and sexual domain scores and a significant increase in all FSFI domain scores were observed in the treatment group after 12 months. This study suggests that a combination of isoflavones, calcium, vitamin D, and inulin may exert favorable effects on menopausal symptoms, sexual function, and quality of life [40].
3.7. Cognition
Sparse research has been done on the effects of isoflavones on cognitive function in menopausal women, possibly because the natural aging process is an inevitable confounding factor. The North American Menopause Society concluded in 2011 that soy may benefit cognitive function in women younger than 65, but not older [10].
A 6-year longitudinal study found that among women of different ethnicities with varying amounts of isoflavone intake undergoing menopause, Asian women with high intake of isoflavone had better processing speed during perimenopause and postmenopause, but worse verbal memory during early perimenopause and postmenopause [41]. The overall cognitive effects were small, casting doubt over the significance of these findings. A systematic review of twelve RCTs suggested isoflavones and soy may improve cognition in postmenopausal women, but pointed out most of the available studies had serious methodological flaws [42].
3.8. Side Effects
Isoflavones were generally well-tolerated in all of the studies the researchers found. Side effects were mild and mostly gastrointestinal, including nausea, bloating, diarrhea, and constipation [1].
There has been concern over S-equol due to previous animal studies. Reproductive abnormalities were found in sheep ingesting red clover, and captive cheetahs fed soy-containing diets became infertile [13]. Ovariectomized Sprague-Dawley rats fed high-dose equol showed clear mammotropic effects after 3 months [43].
This entry is adapted from the peer-reviewed paper 10.3390/nu11112649
References
- Krebs, E.E.; Ensrud, K.E.; MacDonald, R.; Wilt, T.J. Phytoestrogens for treatment of menopausal symptoms: A systematic review. Obstet. Gynecol. 2004, 104, 824–836.
- Croden, J.; Ross, S.; Yuksel, N.; Sydora, B.C. A survey of the availability in Canadian pharmacy chains of over-the-counter natural health products for menopause symptoms. BMC Complement. Altern. Med. 2015, 15, 86.
- Russell, L.; Hicks, G.S.; Low, A.K.; Shepherd, J.M.; Brown, C.A. Phytoestrogens: A viable option? Am. J. Med. Sci. 2002, 324, 185–188.
- Guo, P.P.; Li, P.; Zhang, X.H.; Liu, N.; Wang, J.; Chen, D.D.; Sun, W.J.; Zhang, W. Complementary and alternative medicine for natural and treatment-induced vasomotor symptoms: An overview of systematic reviews and meta-analyses. Complement. Ther. Clin. Pract. 2019, 36, 181–194.
- Hill, D.A.; Crider, M.; Hill, S.R. Hormone therapy and other treatments for symptoms of menopause. Am. Fam. Physician 2016, 94, 884–889.
- Chen, L.R.; Ko, N.Y.; Chen, K.H. Medical Treatment for osteoporosis: From molecular to clinical opinions. Int. J. Mol. Sci. 2019, 20, 2213.
- National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis; National Osteoporosis Foundation: Washington, DC, USA, 2010.
- North American Menopause Society. The role of isoflavones in menopausal health: Consensus opinion of The North American Menopause Society. Menopause 2000, 7, 215–229.
- Tsourounis, C. Clinical effects of phytoestrogens. Clin. Obstet. Gynecol. 2001, 44, 836–842.
- North American Menopause Society. The role of soy isoflavones in menopausal health: Report of The North American Menopause Society/Wulf H. Utian Translational Science Symposium in Chicago, IL (October 2010). Menopause 2011, 18, 732–753.
- Jackson, R.L.; Greiwe, J.S.; Desai, P.B.; Schwen, R.J. Single-dose and steady-state pharmacokinetic studies of S-equol, a potent nonhormonal, estrogen receptor β-agonist being developed for the treatment of menopausal symptoms. Menopause 2011, 18, 185–193.
- Newton, K.M.; Reed, S.D.; Uchiyama, S.; Qu, C.; Ueno, T.; Iwashita, S.; Gunderson, G.; Fuller, S.; Lampe, J.W. A cross-sectional study of equol producer status and self-reported vasomotor symptoms. Menopause 2015, 22, 489–495.
- Setchell, K.D.R. The history and basic science development of soy isoflavones. Menopause 2017, 24, 1338–1350.
- Lambert, M.N.T.; Thorup, A.C.; Hansen, E.S.S.; Jeppesen, P.B. Combined Red Clover isoflavones and probiotics potently reduce menopausal vasomotor symptoms. PLoS ONE 2017, 12, e0176590.
- Guadamuro, L.; Dohrmann, A.B.; Tebbe, C.C.; Mayo, B.; Delgado, S. Bacterial communities and metabolic activity of faecal cultures from equol producer and non-producer menopausal women under treatment with soy isoflavones. BMC Microbiol. 2017, 17, 93.
- Ishiwata, N.; Melby, M.K.; Mizuno, S.; Watanabe, S. New equol supplement for relieving menopausal symptoms: Randomized, placebo-controlled trial of Japanese women. Menopause 2009, 16, 141–148.
- St Germain, A.; Peterson, C.T.; Robinson, J.G.; Alekel, D.L. Isoflavone-rich or isoflavone-poor soy protein does not reduce menopausal symptoms during 24 weeks of treatment. Menopause 2001, 8, 17–26.
- Tice, J.A.; Ettinger, B.; Ensrud, K.; Wallace, R.; Blackwell, T.; Cummings, S.R. Phytoestrogen supplements for the treatment of hot flashes: The Isoflavone Clover Extract (ICE) Study: A randomized controlled trial. JAMA 2003, 290, 207–214.
- Lambert, M.N.T.; Hu, L.M.; Jeppesen, P.B. A systematic review and meta-analysis of the effects of isoflavone formulations against estrogen-deficient bone resorption in peri- and postmenopausal women. Am. J. Clin. Nutr. 2017, 106, 801–811.
- Ma, D.-F.; Qin, L.-Q.; Wang, P.-Y.; Katoh, R. Soy isoflavone intake increases bone mineral density in the spine of menopausal women: Meta-analysis of randomized controlled trials. Clin. Nutr. 2008, 27, 57–64.
- Amato, P.; Young, R.L.; Steinberg, F.M.; Murray, M.J.; Lewis, R.D.; Cramer, M.A.; Barnes, S.; Ellis, K.J.; Shypailo, R.J.; Fraley, J.K.; et al. Effect of soy isoflavone supplementation on menopausal quality of life. Menopause 2013, 20, 443–447.
- Van der Schouw, Y.T.; Kreijkamp-Kaspers, S.; Peeters, P.H.M.; Keinan-Boker, L.; Rimm, E.B.; Grobbee, D.E. Prospective study on usual dietary phytoestrogen intake and cardiovascular disease risk in Western women. Circulation 2005, 111, 465–471.
- Nestel, P.J.; Yamashita, T.; Sasahara, T.; Pomeroy, S.; Dart, A.; Komesaroff, P.; Owen, A.; Abbey, M. Soy isoflavones improve systemic arterial compliance but not plasma lipids in menopausal and perimenopausal women. Arterioscler. Thromb. Vasc. Biol. 1997, 17, 3392–3398.
- Cheng, G.; Wilczek, B.; Warner, M.; Gustafsson, J.-A.; Landgren, B.M. Isoflavone treatment for acute menopausal symptoms. Menopause 2007, 14, 468–473.
- Brzezinski, A.; Danenberg, H.D. Sex hormones, soy, and myocardial injury. Menopause 2008, 15, 217–220.
- Wong, W.W.; Taylor, A.A.; Smith, E.O.; Barnes, S.; Hachey, D.L. Effect of soy isoflavone supplementation on nitric oxide metabolism and blood pressure in menopausal women. Am. J. Clin. Nutr. 2012, 95, 1487–1494.
- Suparto, I.H.; Williams, J.K.; Fox, J.L.; Yusuf, J.T.L.; Sajuthi, D. Effects of hormone therapy and dietary soy on myocardial ischemia/reperfusion injury in ovariectomized atherosclerotic monkeys. Menopause 2008, 15, 256–263.
- Sathyapalan, T.; Aye, M.; Rigby, A.S.; Thatcher, N.J.; Dargham, S.R.; Kilpatrick, E.S.; Atkin, S.L. Soy isoflavones improve cardiovascular disease risk markers in women during the early menopause. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 691–697.
- Stuenkel, C.A. Isoflavones and cardiovascular risk in postmenopausal women: No free lunch. Menopause 2007, 14, 606–608.
- Mueller, M.; Jungbauer, A. Red clover extract: A putative source for simultaneous treatment of menopausal disorders and the metabolic syndrome. Menopause 2008, 15, 1120–1131.
- Reiter, E.; Beck, V.; Medjakovic, S.; Mueller, M.; Jungbauer, A. Comparison of hormonal activity of isoflavone-containing supplements used to treat menopausal complaints. Menopause 2009, 16, 1049–1060.
- Hirose, K.; Imaeda, N.; Tokudome, Y.; Goto, C.; Wakai, K.; Matsuo, K.; Ito, H.; Toyama, T.; Iwata, H.; Tokudome, S.; et al. Soybean products and reduction of breast cancer risk: A case—Control study in Japan. Br. J. Cancer 2005, 93, 15–22.
- Alipour, S.; Afshar, S.; Moini, A.; Dastjerdi, M.; Saberi, A.; Bayani, L.; Eslami, B.; Hosseini, L. Clinical and ultrasonographic changes of the breast after use of soy isoflavones. APJCP 2012, 13, 6093–6095.
- Shike, M.; Doane, A.S.; Russo, L.; Cabal, R.; Reis-Filho, J.S.; Gerald, W.; Cody, H.; Khanin, R.; Bromberg, J.; Norton, L. The effects of soy supplementation on gene expression in breast cancer: A randomized placebo-controlled study. J. Natl. Cancer Inst. 2014, 106, dju189.
- Kang, X.; Zhang, Q.; Wang, S.; Huang, X.; Jin, S. Effect of soy isoflavones on breast cancer recurrence and death for patients receiving adjuvant endocrine therapy. CMAJ 2010, 182, 1857–1862.
- Shin, A.; Lee, J.; Lee, J.; Park, M.S.; Park, J.W.; Park, S.C.; Oh, J.H.; Kim, J. Isoflavone and soyfood intake and colorectal cancer risk: A case-control study in Korea. PLoS ONE 2015, 10, e0143228.
- Waetjen, L.E.; Leung, K.; Crawford, S.L.; Huang, M.-H.; Gold, E.B.; Greendale, G.A. Study of women’s health across the nation relationship between dietary phytoestrogens and development of urinary incontinence in midlife women. Menopause 2013, 20, 428–436.
- Reed, S.D.; Newton, K.M.; LaCroix, A.Z.; Grothaus, L.C.; Grieco, V.S.; Ehrlich, K. Vaginal, endometrial, and reproductive hormone findings: Randomized, placebo-controlled trial of black cohosh, multibotanical herbs, and dietary soy for vasomotor symptoms: The Herbal Alternatives for Menopause (HALT) Study. Menopause 2008, 15, 51–58.
- Burton, J.L.; Wells, M. The effect of phytoestrogens on the female genital tract. J. Clin. Pathol. 2002, 55, 401–407.
- Vitale, S.G.; Caruso, S.; Rapisarda, A.M.C.; Cianci, S.; Cianci, A. Isoflavones, calcium, vitamin D and inulin improve quality of life, sexual function, body composition and metabolic parameters in menopausal women: Result from a prospective, randomized, placebo-controlled, parallel-group study. Prz. Menopauzalny 2018, 17, 32–38.
- Greendale, G.A.; Huang, M.-H.; Leung, K.; Crawford, S.L.; Gold, E.B.; Wight, R.; Waetjen, E.; Karlamangla, A.S. Dietary phytoestrogen intakes and cognitive function during the menopausal transition: Results from the study of women’s health across the nation phytoestrogen Study. Menopause 2012, 19, 894–903.
- Clement, Y.N.; Onakpoya, I.; Hung, S.K.; Ernst, E. Effects of herbal and dietary supplements on cognition in menopause: A systematic review. Maturitas 2011, 68, 256–263.
- Rachoń, D.; Menche, A.; Vortherms, T.; Seidlová-Wuttke, D.; Wuttke, W. Effects of dietary equol administration on the mammary gland in ovariectomized Sprague-Dawley rats. Menopause 2008, 15, 340–345.
This entry is offline, you can click here to edit this entry!
