Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Advancements in modern medicine have bolstered the usage of home-based rehabilitation services for patients, particularly those recovering from diseases or conditions that necessitate a structured rehabilitation process. Understanding the technological factors that can influence the efficacy of home-based rehabilitation is crucial for optimizing patient outcomes. As technologies continue to evolve rapidly, it is imperative to document the current state-of-the-art and elucidate the key features of the hardware and software employed in these rehabilitation systems.
- home-based rehabilitation
- wearables
- robots
- exoskeletons
1. Introduction
The shoulder joint, renowned for its exceptional range of movement, plays a crucial role in enabling essential daily activities, such as reaching, lifting, or throwing [1]. Coordinated movement between the humerus, scapula, clavicle, thoracic wall, and thoracic spine is vital for optimal shoulder function, and injuries to these structures can significantly impair shoulder motion [2]. With advancing age, the incidence of common shoulder pathologies, including tendinopathy and osteoarthritis, rises progressively, affecting a substantial portion of individuals aged 65 and above [3][4][5]. Notably, rotator cuff tears pose a significant concern, afflicting approximately one-fifth of the global adult population and up to half of those aged 66 years and above [6]. The prevalence of upper limb pain among adults is striking, with 36% of the population reporting such pain and a substantial portion of these cases contributing to significant morbidity, healthcare resource consumption, and work productivity loss. Hence, the proper evaluation and treatment of shoulder pathologies assume paramount importance [7].
Recognized as an alternative or complementary approach to traditional care-unit-based therapy, home-based rehabilitation empowers patients by fostering autonomy and facilitating their recovery to regain their ability to perform daily tasks [8]. This approach offers numerous advantages for patients and healthcare organizations, including resource optimization, reduced travel time, flexible appointment scheduling, improved therapist availability, and prompt feedback delivery [9]. Consequently, home-based rehabilitation enables the transition of patients who would otherwise require in-patient care to an outpatient setting, where they actively engage in prescribed rehabilitation exercises at home, promoting adherence to the treatment regimen [10][11][12].
Maintaining high-quality healthcare services in a home-based rehabilitation setting necessitates the use of medical devices capable of monitoring patients, complemented with periodic supervisions from healthcare professionals [13]. Well-designed medical devices should ensure reliable clinical treatment, prioritize patient safety and well-being, and safeguard the caregivers and healthcare providers involved [14]. In recent years, advancements in remote monitoring technologies, particularly in e-health, have facilitated the migration of various devices from hospital settings to home-based paradigms. These devices, often managed by non-health professionals, are now designed to be more compact and smaller, ergonomic, and user friendly, catering to the needs of diverse users [15].
2. Technology Solutions for Home-Based Shoulder Rehabilitation
In the realm of medical advancements, numerous devices are currently under development, with many designed for use in clinical or hospital settings due to their inherent complexity. However, certain devices and technologies offer relative simplicity in their operation, making them well suited for home use and enabling patients to regain autonomy and independence in their rehabilitation journey [16]. Figure 1 presents an overview of these key technologies, categorized into the domains of physical and virtual applications, each playing a significant role in home-based rehabilitation. By exploring these technologies, researchers can better understand their potential impact and effectiveness in supporting patients’ rehabilitation progress.
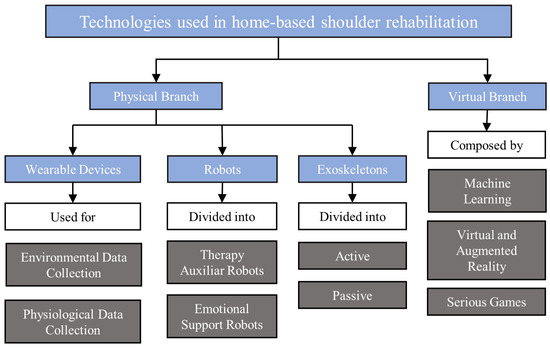
Figure 1. Technologies used for home-based shoulder rehabilitation.
Within the realm of physical technologies, wearable devices, also known as wearables, have emerged as a transformative tool in modern medicine. These devices incorporate sensors, which gather data from the patient and/or the surrounding environment, facilitating continuous monitoring outside traditional healthcare settings. Through the utilization of advanced computational algorithms, wearables enable event prediction, prevention, and intervention, thus revolutionizing the field [17]. Notably, wearable devices offer a promising avenue for long-term monitoring and follow-up in the context of home-based shoulder rehabilitation, as evidenced by recent scientific publications [18][19][20][21][22]. By harnessing the potential of wearables, healthcare providers can gather valuable insights and optimize the rehabilitation process to enhance patient outcomes and recovery.
The integration of rehabilitation robots has been a pivotal aspect of therapy since the 1990s, serving as a valuable aid in administering treatment to patients. These robots employ computerized interfaces to assist individuals in completing tasks, offering not only physical support but also emotional encouragement and motivation. Numerous studies have demonstrated the positive impact of robot-assisted training on arm function and overall ability in daily activities [23][24][25][26]. Additionally, exoskeletons, which are wearable robotic units designed to augment and enhance human physical capabilities, have gained prominence, particularly among individuals with reduced mobility [27]. The growing demand for upper limb exoskeletons has led to the development of new and advanced models in recent times [28][29][30][31]. By harnessing the potential of rehabilitation robots and exoskeletons, patients can benefit from enhanced therapy outcomes and improved quality of life.
In the realm of virtual approaches to home-based rehabilitation, the integration of machine learning has revolutionized the automation of processes by harnessing artificial intelligence and pattern recognition capabilities [32]. Through the analysis of empirical data collected from sensors embedded in modern smartphones and wearables, machine-learning algorithms can gather user and environmental information, enabling real-time adaptation to the prevailing conditions, as if the systems were continuously learning and evolving [32]. Deep learning, a subset of machine learning, has particularly contributed to remarkable advancements in image recognition and behavior prediction within the field of rehabilitation [33]. Over the years, deep learning has demonstrated its efficacy in shoulder rehabilitation, exemplified by numerous studies, which will be explored in this article [32][34][35][36]. By leveraging the power of machine learning and its subfield of deep learning, home-based rehabilitation can capitalize on sophisticated algorithms to optimize treatment outcomes and refine personalized interventions.
The increasing adoption of virtual and augmented reality systems in recent years indicates a shift toward a more e-health-focused approach in both medical and social rehabilitation [37]. These systems have the capability to simulate realistic scenes, providing valuable support to individuals with disabilities throughout the rehabilitation process. Notably, the literature showcases various examples where virtual and augmented reality technologies have been successfully employed to enhance rehabilitation outcomes [38][39][40][41][42]. By immersing users in interactive and lifelike environments, these technologies offer new avenues for therapeutic interventions and enable individuals to engage in meaningful and immersive rehabilitation experiences.
A compelling concept, which has emerged in the realm of physical rehabilitation, is the use of serious games. These games combine educational, informational, and rehabilitative aspects with the entertaining and enjoyable elements of video games [43]. The versatility of gamification in rehabilitation is vast, as it can leverage various technologies, such as virtual reality or robots [44][45][46][47]. By integrating game mechanics, challenges, and rewards, serious games provide an engaging and motivating platform for individuals undergoing rehabilitation, encouraging active participation and facilitating progress tracking. The integration of serious games into home-based rehabilitation programs has the potential to transform therapy into a more enjoyable and interactive experience, ultimately improving patient engagement and treatment outcomes.
With the foundational technologies discussed, the subsequent sections will delve deeper into their key features, providing illustrative examples and conducting in-depth analyses.
3. Considerations for Therapeutic Exercises in Home-Based Rehabilitation
Enhancing shoulder functionality through physical rehabilitation is a crucial aspect of achieving effective recovery following injury or surgery. This process entails engaging in appropriate rehabilitation exercises, which target various movement planes to enhance motor function [48]. By providing targeted stimuli, these exercises contribute to the improvement of patient fitness and functional ability, enabling them to achieve positive outcomes even when undertaking home-based rehabilitation or self-management without direct supervision from a healthcare professional [49].
4. Guidelines for Home-Based Rehabilitation Systems
Developing effective home-based rehabilitation systems requires adherence to specific guidelines to ensure optimal user experience, safety, and positive rehabilitation outcomes. Below, researchers propose a set of guidelines, which should be followed during the development process:
-
User-centric design: Prioritize user needs and preferences when designing the system interface. Create an intuitive and user-friendly interface, which accommodates individuals with varying technological proficiency, ensuring easy navigation and engagement during home-based rehabilitation sessions.
-
Accessibility and inclusivity: Ensure that the system is accessible to a diverse range of users, including those with physical disabilities, visual impairments, and cognitive limitations. Incorporate features such as adjustable font sizes, voice guidance, and alternative input methods to enhance accessibility for all patients.
-
Customization and adaptability: Provide options for customization and adaptation of the system to meet individual patients’ specific needs. Allow for adjustments in difficulty levels, exercise intensity, and duration based on the patient’s progress and capabilities.
-
Real-time feedback and guidance: Incorporate mechanisms to provide real-time feedback and guidance during exercises. Utilize visual cues, auditory signals, or haptic feedback to help patients perform exercises correctly and optimize their rehabilitation progress.
-
Comprehensive progress tracking: Develop a robust system for tracking and recording patients’ progress over time. Monitor metrics such as exercise completion rates, duration, intensity, and improvements in performance. Utilize these data to personalize future exercise plans and set realistic goals for patients.
-
Safety measures and risk mitigation: Prioritize patient safety by integrating safety measures into the system. Use technologies such as motion sensors to detect incorrect movements or provide warnings when patients exceed safe ranges of motion. Implement risk mitigation strategies to prevent injury during exercises.
-
Data privacy and security: Ensure that the system complies with data privacy regulations and incorporates robust security measures to protect patient information. Implement measures to safeguard sensitive data and provide patients with control over their data and their usage.
-
Seamless integration with healthcare professionals: Enable seamless communication and data exchange between the home-based rehabilitation system and healthcare professionals involved in the patients’ care. Facilitate remote monitoring, feedback, and the ability to make informed adjustments to the rehabilitation program based on professional expertise.
-
Artificial intelligence and machine-learning integration: Explore opportunities to integrate artificial intelligence or machine-learning algorithms into the home-based rehabilitation system. Leverage artificial intelligence capabilities to analyze patient data, identify patterns, and provide personalized recommendations for exercise progression, adapting the rehabilitation program based on individual needs and response to treatment.
-
Scalability and compatibility: Design the system to be scalable and compatible with various devices and platforms. Accommodate different technologies and future advancements, ensuring flexibility and long-term viability of the home-based rehabilitation system.
By adhering to these guidelines, researchers and developers can create effective home-based rehabilitation systems, which prioritize user needs, promote engagement, and improve rehabilitation outcomes. These systems contribute to the advancement of rehabilitation practices and enhance the overall well-being of patients undergoing home-based rehabilitation programs.
4.1. Ethical Concerns
As technology continues to advance in the field of home-based rehabilitation systems, it is crucial to address the ethical considerations associated with their use. The following ethical concerns should be taken into account when developing and implementing such systems:
-
Privacy and data security: Home-based rehabilitation systems often involve the collection and storage of sensitive personal health information. It is essential to ensure that robust data protection measures are in place to safeguard patient privacy and prevent unauthorized access or misuse of the data.
-
Informed consent: Patients participating in home-based rehabilitation programs should be adequately informed about the purpose, risks, benefits, and potential limitations of the technology being used. Informed consent should be obtained, outlining the scope of data collection, potential risks, and the patient’s right to withdraw from the program at any time.
-
Equity and accessibility: It is important to consider the equitable access and availability of home-based rehabilitation systems to ensure that all individuals, regardless of socioeconomic status or geographical location, have equal opportunities for rehabilitation and benefit from the technology.
-
User autonomy and empowerment: Home-based rehabilitation systems should be designed to empower patients and promote their active involvement in their own care. The technology should support patient autonomy, allowing them to make informed decisions about their treatment and providing them with tools for self-management.
-
Transparent and explainable AI: If machine-learning algorithms are integrated into the rehabilitation systems, there is a need for transparency and explainability. Patients should have a clear understanding of how AI is being used, what factors influence treatment recommendations, and the basis for any decisions made by the system.
-
Clinical oversight and human interaction: While home-based rehabilitation systems offer the advantage of remote monitoring and independent practice, it is essential to maintain a balance between technology-driven interventions and the involvement of healthcare professionals. Regular clinical oversight and human interaction should be incorporated into the system to ensure patient safety, address individual needs, and provide timely support or intervention when required.
Addressing these ethical concerns is paramount to fostering trust, protecting patient rights, and ensuring the responsible and ethical implementation of home-based rehabilitation systems. By considering these ethical considerations, developers and healthcare professionals can work together to create systems, which prioritize patient well-being, privacy, and equitable access to high-quality rehabilitation care.
This entry is adapted from the peer-reviewed paper 10.3390/s23167100
References
- Itoi, E. “On-Track” and “off-Track” Shoulder Lesions. EFORT Open Rev. 2017, 2, 343–351.
- Papalia, R.; Torre, G.; Papalia, G.; Baums, M.H.; Narbona, P.; Di Lazzaro, V.; Denaro, V. Frozen Shoulder or Shoulder Stiffness from Parkinson Disease? Musculoskelet. Surg. 2019, 103, 115–119.
- Heuberer, P.R.; Plachel, F.; Willinger, L.; Moroder, P.; Laky, B.; Pauzenberger, L.; Lomoschitz, F.; Anderl, W. Critical Shoulder Angle Combined with Age Predict Five Shoulder Pathologies: A Retrospective Analysis of 1000 Cases. BMC Musculoskelet. Disord. 2017, 18, 259.
- Carr, J.B.; Rodeo, S.A. The Role of Biologic Agents in the Management of Common Shoulder Pathologies: Current State and Future Directions. J. Shoulder Elbow Surg. 2019, 28, 2041–2052.
- Vocelle, A.R.; Weidig, G.; Bush, T.R. Shoulder Structure and Function: The Impact of Osteoarthritis and Rehabilitation Strategies. J. Hand Ther. 2022, 35, 377–387.
- Cvetanovich, G.L.; Waterman, B.R.; Verma, N.N.; Romeo, A.A. Management of the Irreparable Rotator Cuff Tear. J. Am. Acad. Orthop. Surg. 2019, 27, 909–917.
- Walker-Bone, K.; Palmer, K.T.; Reading, I.; Coggon, D.; Cooper, C. Prevalence and Impact of Musculoskeletal Disorders of the Upper Limb in the General Population. Arthritis Care Res. 2004, 51, 642–651.
- Greiner, J.J.; Drain, N.P.; Lesniak, B.P.; Lin, A.; Musahl, V.; Irrgang, J.J.; Popchak, A.J. Self-Reported Outcomes in Early Postoperative Management After Shoulder Surgery Using a Home-Based Strengthening and Stabilization System with Telehealth. Sports Health 2022, 15, 599–605.
- Chen, Y.; Abel, K.T.; Janecek, J.T.; Chen, Y.; Zheng, K.; Cramer, S.C. Home-Based Technologies for Stroke Rehabilitation—A Systematic Review. Int. J. Med. Inf. 2019, 123, 11–15.
- Dunn, J.; Runge, R.; Snyder, M. Wearables and the Medical Revolution. Pers. Med. 2018, 15, 429–448.
- Osgouei, R.H.; Soulsby, D.; Bello, F. Rehabilitation Exergames: Use of Motion Sensing and Machine Learning to Quantify Exercise Performance in Healthy Volunteers. JMIR Rehabil. Assist. Technol. 2020, 7, e17289.
- Cunha, B.; Gonçalves, L. An IoMT Architecture for Patient Rehabilitation Based on Low-Cost Hardware and Interoperability Standards. In Exploring the Convergence of Computer and Medical Science Through Cloud Healthcare; IGI Global: Hershey, PA, USA, 2023; pp. 37–59.
- Sfantou, D.F.; Laliotis, A.; Patelarou, A.E.; Sifaki-Pistolla, D.; Matalliotakis, M.; Patelarou, E. Importance of Leadership Style towards Quality of Care Measures in Healthcare Settings: A Systematic Review. Healthcare 2017, 5, 73.
- Kim, D.S.; Lee, H.J.; Lee, S.H.; Chang, W.H.; Jang, J.; Choi, B.O.; Ryu, G.H.; Kim, Y.H. A Wearable Hip-Assist Robot Reduces the Cardiopulmonary Metabolic Energy Expenditure during Stair Ascent in Elderly Adults: A Pilot Cross-Sectional Study. BMC Geriatr. 2018, 18, 230.
- Akbari, A.; Haghverd, F.; Behbahani, S. Robotic Home-Based Rehabilitation Systems Design: From a Literature Review to a Conceptual Framework for Community-Based Remote Therapy During COVID-19 Pandemic. Front. Robot. AI 2021, 8, 612331.
- Gallagher, J.F.; Sivan, M.; Levesley, M. Making Best Use of Home-Based Rehabilitation Robots. Appl. Sci. 2022, 12, 1996.
- Seneviratne, S.; Hu, Y.; Nguyen, T.; Lan, G.; Khalifa, S.; Thilakarathna, K.; Hassan, M.; Seneviratne, A. A Survey of Wearable Devices and Challenges. IEEE Commun. Surv. Tutor. 2017, 19, 2573–2620.
- Galiana, I.; Hammond, F.L.; Howe, R.D.; Popovic, M.B. Wearable Soft Robotic Device for Post-Stroke Shoulder Rehabilitation: Identifying Misalignments. In Proceedings of the 2012 IEEE/RSJ International Conference on Intelligent Robots and Systems, Vilamoura-Algarve, Portugal, 7–12 October 2012; pp. 317–322.
- Longo, U.G.; Risi Ambrogioni, L.; Berton, A.; Candela, V.; Carnevale, A.; Schena, E.; Gugliemelli, E.; Denaro, V. Physical Therapy and Precision Rehabilitation in Shoulder Rotator Cuff Disease. Int. Orthop. 2020, 44, 893–903.
- Majidi Fard Vatan, H.; Nefti-Meziani, S.; Davis, S.; Saffari, Z.; El-Hussieny, H. A Review: A Comprehensive Review of Soft and Rigid Wearable Rehabilitation and Assistive Devices with a Focus on the Shoulder Joint. J. Intell. Robot. Syst. Theory Appl. 2021, 102, 9.
- Kesner, S.B.; Jentoft, L.; Hammond, F.; Howe, R.D.; Popovic, M. Design Considerations for an Active Soft Orthotic System for Shoulder Rehabilitation. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; pp. 8130–8134.
- Chen, Y.P.; Lin, C.Y.; Tsai, M.J.; Chuang, T.Y.; Lee, O.K.S. Wearable Motion Sensor Device to Facilitate Rehabilitation in Patients with Shoulder Adhesive Capsulitis: Pilot Study to Assess Feasibility. J. Med. Internet Res. 2020, 22, e17032.
- Niyetkaliyev, A.S.; Hussain, S.; Ghayesh, M.H.; Alici, G. Review on Design and Control Aspects of Robotic Shoulder Rehabilitation Orthoses. IEEE Trans. Hum.-Mach. Syst. 2017, 47, 1134–1145.
- Ball, S.J.; Brown, I.E.; Scott, S.H. MEDARM: A Rehabilitation Robot with 5DOF at the Shoulder Complex. In Proceedings of the 2007 IEEE/ASME International Conference on Advanced Intelligent Mechatronics, Zurich, Switzerland, 4–7 September 2007; pp. 1–6.
- Tucan, P.; Vaida, C.; Ulinici, I.; Banica, A.; Burz, A.; Pop, N.; Birlescu, I.; Gherman, B.; Plitea, N.; Antal, T.; et al. Optimization of the ASPIRE Spherical Parallel Rehabilitation Robot Based on Its Clinical Evaluation. Int. J. Environ. Res. Public. Health 2021, 18, 3281.
- Zimmermann, Y.D.; Forino, A.; Riener, R.; Hutter, M. ANYexo: A Versatile and Dynamic Upper-Limb Rehabilitation Robot. IEEE Robot. Autom. Lett. 2019, 4, 3649–3656.
- Gull, M.A.; Bai, S.; Bak, T. A Review on Design of Upper Limb Exoskeletons. Robotics 2020, 9, 16.
- Soltani-zarrin, R.; Zeiaee, A.; Langari, R.; Tafreshi, R. Challenges and Opportunities in Exoskeleton-Based Rehabilitation. arXiv 2017, arXiv:1711.09523.
- Li, N.; Yang, T.; Yang, Y.; Chen, W.; Yu, P.; Zhang, C.; Xi, N.; Zhao, Y. Designing Unpowered Shoulder Complex Exoskeleton via Contralateral Drive for Self-Rehabilitation of Post-Stroke Hemiparesis. J. Bionic Eng. 2022, 20, 992–1007.
- Trigili, E.; Crea, S.; Moise, M.; Baldoni, A.; Cempini, M.; Ercolini, G.; Marconi, D.; Posteraro, F.; Carrozza, M.C.; Vitiello, N. Design and Experimental Characterization of a Shoulder-Elbow Exoskeleton with Compliant Joints for Post-Stroke Rehabilitation. EEEASME Trans. Mechatron. 2019, 24, 1485–1496.
- Meng, Q.; Xu, R.; Xie, Q.; Mahmutjan, B.; Li, S.; Yu, H. Bionic Design to Reduce Driving Power for a Portable Elbow Exoskeleton Based on Gravity—Balancing Coupled Model. J. Bionic Eng. 2022, 20, 146–157.
- Ramkumar, P.N.; Haeberle, H.S.; Navarro, S.M.; Sultan, A.A.; Mont, M.A.; Ricchetti, E.T.; Schickendantz, M.S.; Iannotti, J.P. Mobile Technology and Telemedicine for Shoulder Range of Motion: Validation of a Motion-Based Machine-Learning Software Development Kit. J. Shoulder Elbow Surg. 2018, 27, 1198–1204.
- Ren, J.L.; Chien, Y.H.; Chia, E.Y.; Fu, L.C.; Lai, J.S. Deep Learning Based Motion Prediction for Exoskeleton Robot Control in Upper Limb Rehabilitation. In Proceedings of the 2019 International Conference on Robotics and Automation (ICRA), Montreal, QC, Canada, 20–24 May 2019; pp. 5076–5082.
- Ongvisatepaiboon, K.; Chan, J.H.; Vanijja, V. Smartphone-Based Tele-Rehabilitation System for Frozen Shoulder Using a Machine Learning Approach. In Proceedings of the 2015 IEEE Symposium Series on Computational Intelligence, Cape Town, South Africa, 7–10 December 2015; pp. 811–815.
- Jiang, Y.; Chen, C.; Zhang, X.; Chen, C.; Zhou, Y.; Ni, G.; Muh, S.; Lemos, S. Shoulder Muscle Activation Pattern Recognition Based on SEMG and Machine Learning Algorithms. Comput. Methods Programs Biomed. 2020, 197, 105721.
- Chae, S.H.; Kim, Y.; Lee, K.S.; Park, H.S. Development and Clinical Evaluation of a Web-Based Upper Limb Home Rehabilitation System Using a Smartwatch and Machine Learning Model for Chronic Stroke Survivors: Prospective Comparative Study. JMIR MHealth UHealth 2020, 8, e17216.
- Kolsanov, A.; Chaplygin, S.; Rovnov, S.; Ivaschenko, A. Augmented Reality Application for Hand Motor Skills Rehabilitation. Int. J. Adv. Comput. Sci. Appl. 2020, 11, 51–57.
- Powell, M.O.; Elor, A.; Robbins, A.; Kurniawan, S.; Teodorescu, M. Predictive Shoulder Kinematics of Rehabilitation Exercises Through Immersive Virtual Reality. IEEE Access 2022, 10, 25621–25632.
- Condino, S.; Turini, G.; Viglialoro, R.; Gesi, M.; Ferrari, V. Wearable Augmented Reality Application for Shoulder Rehabilitation. Electronics 2019, 8, 1178.
- Aung, Y.M.; Al-Jumaily, A. Augmented Reality-Based RehaBio System for Shoulder Rehabilitation. Int. J. Mechatron. Autom. 2014, 4, 52–62.
- Carnevale, A.; Mannocchi, I.; Sassi, M.S.H.; Carli, M.; De Luca, G.; Longo, U.G.; Denaro, V.; Schena, E. Virtual Reality for Shoulder Rehabilitation: Accuracy Evaluation of Oculus Quest 2. Sensors 2022, 22, 5511.
- Funao, H.; Tsujikawa, M.; Momosaki, R.; Shimaoka, M. Virtual Reality Applied to Home-Visit Rehabilitation for Hemiplegic Shoulder Pain in a Stroke Patient: A Case Report. J. Rural Med. 2021, 16, 174–178.
- Al Fatta, H.; Maksom, Z.; Zakaria, M.H. Game-Based Learning and Gamification: Searching for Definitions. Int. J. Simul. Syst. Sci. Technol. 2018, 19, 41.1–41.5.
- Morando, M.; Serena, P.; Ferrara, E.; Dellepiane, S. Definition of Motion and Biophysical Indicators for Home-Based Rehabilitation through Serious Games. Information 2018, 9, 105.
- Guillén-Climent, S.; Garzo, A.; Muñoz-Alcaraz, M.N.; Casado-Adam, P.; Arcas-Ruiz-Ruano, J.; Mejías-Ruiz, M.; Mayordomo-Riera, F.J. A Usability Study in Patients with Stroke Using MERLIN, a Robotic System Based on Serious Games for Upper Limb Rehabilitation in the Home Setting. J. NeuroEng. Rehabil. 2021, 18, 41.
- Ventura, R.B.; Hughes, K.S.; Nov, O.; Raghavan, P.; Marín, M.R.; Porfiri, M. Data-Driven Classification of Human Movements in Virtual Reality-Based Serious Games: Preclinical Rehabilitation Study in Citizen Science. JMIR Serious Games 2022, 10, e27597.
- Alarcón-Aldana, A.C.; Callejas-Cuervo, M.; Bo, A.P.L. Upper Limb Physical Rehabilitation Using Serious Videogames and Motion Capture Systems: A Systematic Review. Sensors 2020, 20, 5989.
- Lee, S.H.; Yeh, S.C.; Chan, R.C.; Chen, S.; Yang, G.; Zheng, L.R. Motor Ingredients Derived from a Wearable Sensor-Based Virtual Reality System for Frozen Shoulder Rehabilitation. BioMed Res. Int. 2016, 2016, 7075464.
- Bollen, J.C.; Dean, S.G.; Siegert, R.J.; Howe, T.E.; Goodwin, V.A. A Systematic Review of Measures of Self-Reported Adherence to Unsupervised Home-Based Rehabilitation Exercise Programmes, and Their Psychometric Properties. BMJ Open 2014, 4, e005044.
This entry is offline, you can click here to edit this entry!
