Spinal cord injury (SCI) is a catastrophic condition associated with significant neurological deficit and social and financial burdens. The advancements in biomaterial technology, combined with stem cell therapy or other regenerative therapy, can now accelerate the progress of promising novel therapeutic strategies from bench to bedside. Various types of approaches to regeneration therapy for SCI have been combined with the use of supportive biomaterial scaffolds as a drug and cell delivery system to facilitate favorable cell–material interactions and the supportive effect of neuroprotection.
1. Introduction
Spinal cord injuries (SCIs) are a serious problem for those affected. The physical, emotional and economic problems caused by SCI generally considerably limit an individual’s functionality and are a burden on society. One recent survey reported an annual incidence of SCI of approximately 54 cases per one million people [
1,
2], with an estimated yearly incidence worldwide of 250,000–500,000 cases [
3]. The spinal cord has very little ability to spontaneously or functionally regenerate itself, thus resulting in serious and often permanent disabilities. Unfortunately, 95% of patients with SCI are in the chronic phase [
4]. The cause of SCI is triggered by several types of physical impacts, including traffic accidents, falls and sports injuries, etc., in which spinal vertebrae, facet joints, disks and ligamentous structures are injured and lose stability. The impact load is therefore transferred to the spinal cord and injures it. The external insult is reflected in primary spinal tissue damage and neural cell death in the acute phase, while a subsequential secondary cascade of degenerative events is started [
5] (
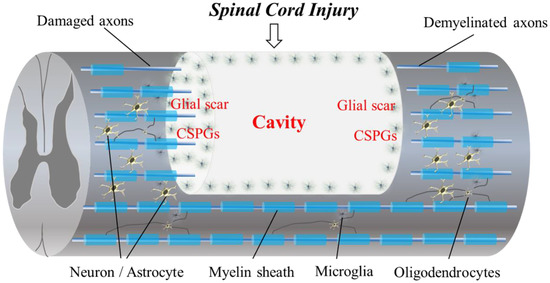
Figure 1).
Figure 1. The diagram shows the pathophysiological events in SCI. Progressive demyelination results in the degeneration of axonal fibers. A cavitation occurs in the epicenter. Hypertrophic astrocytes with very long processes over the tips of non-regenerating fibers form a barrier known as a glial wall around the cavitation. In response to injury, microglial cells transform into active phagocytic microglia and exhibit chemotaxis. The presence of CSPGs creates an inhibitory environment for axonal regeneration. In addition, CSPG also inhibits the migration and differentiation of oligodendrocyte progenitor cells.
Spinal surgery is often necessary to reduce the cervical dislocation and to remove fragments of bones, herniated disks, foreign objects or fractured vertebrae that appear to be compressing the spinal cord and cervical nerve roots. Surgery might also be needed to stabilize the spine to prevent future pain or deformity. Unfortunately, there is no way to reverse damage to the original spinal cord [
1,
2,
3,
4,
5,
6].
Recent progress in medicine, biology and biomaterials engineering in neurosurgery, biomaterial development, cell culture and tissue engineering has allowed for new therapies in SCI. This has contributed to the possibility of healing traumatic SCI and preventing further neurodegeneration [
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17,
18,
19]. It remains a severe clinical challenge to effectively treat SCI due to the poor regenerative capacity and complex anatomy of the spinal cord. Several biomaterials that act as scaffolds for axonal growth, cells and neurotrophic factors have become excellent candidates to support the regeneration of the spinal cord.
Recent review articles in new treatments for SCI have mentioned the possibility of clinical applications and the progression of a new regenerative therapy for SCI, including the most recent preclinical results and clinical trials [
5,
6,
18,
19,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29,
30,
31,
32]. However, there have been few review articles in SCI that have mentioned the status of the use of recent biomaterial scaffolds for regenerative therapy and summarized the strategies with simplified results data. In this context, therefore, particular attention has been drawn to biomaterials and nanotechnology-enabled products for the controlled delivery and sustained release of various moieties, including drugs, bioactive molecules and cells [
5].
2. Barriers to Regeneration and the Pathophysiology of SCI
The regeneration of the adult mammalian central nervous system (CNS) and spinal cord is difficult due to its limited plasticity [
1,
6,
14,
15,
16]. Cavitation occurs in the epicenter of a CNS lesion, with this becoming surrounded by connective scar tissue containing cerebrospinal fluid. Reactive astrocytes transform into scar-forming astrocytes that slow the crossing of regenerating axons into the lesion. Certain inflammatory immune cells also remain around the lesion epicenter at the site of the SCI [
1,
6,
14,
15,
16,
17,
18,
19]. Following SCI, astrocytes are activated, and they proliferate and migrate to the perilesional region to form processes in a dense interwoven network, depositing chondroitin sulfate proteoglycans (CSPGs) into the extracellular matrix (ECM). Dystrophic axons surround the epicenter of the injury and are trapped in the dense meshwork of scar tissue [
15,
17]. Biomaterial scaffolds that generate specific microenvironmental cues in a three-dimensional (3D), controlled fashion to enhance the survival, infiltration and differentiation of cells [
18] are used for spinal cord regeneration following injury.
3. Categories of Biomaterial Scaffolds Applied in Regeneration Therapy for SCI
The biomaterial scaffolds used in spinal cord regeneration can be classified according to the required structure and physical and biological properties of the prospective tissue construct applied in SCI. The categories of the biomaterial scaffolds used in spinal cord regeneration include hydrogels, biodegradable scaffolds, the use of micro/nanofibers as instructive biomaterials and drug-delivering biomaterials [
29,
30,
31,
32].
3.1. Hydrogels
Hydrogels are one of the most appealing and frequently engineered scaffolds. They are made up of 3D cross-linked biocompatible polymeric macroporous networks that supply the permissive microenvironment and guidance cues necessary for axonal growth [
7,
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
49,
50,
51,
52,
53,
54,
55,
56,
57,
58,
59,
60,
61,
62]. Hydrogels are hydrated networks that mimic the ECM of soft tissues [
30,
31]. Natural hydrogels usually contain fibrillar proteins within a hydrated glycosaminoglycan network that can enhance cell adhesion and migration in the lesion site. The natural polymers used for nerve tissue engineering include agarose, alginate, chitosan, collagen, fibrin, fibronectin, hyaluronic acid (HA) and Matrigel™ [
30,
31]. Natural polymers deliver excellent biomimicking, but synthetic hydrogels have also attracted attention because they can potentially control their rate of degradation and for their mechanical properties [
30,
31].
Researchers reviewed the effects of hydrogel scaffolds on pathophysiologiocal events and motor functional recovery [
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
49,
50,
51,
52,
53,
54,
55,
56,
57,
58,
59,
60,
61,
62]. Several types of hydrogels have been reported to date [
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
49,
50,
51,
52,
53,
54,
55,
56,
57,
58,
59,
60,
61,
62]. Biopolymer-based hydrogel scaffolds are categorized into natural polymers, synthetic polymers and self-assembling peptides according to the origin of the biomaterial used [
7,
63]. Twenty-nine articles revealed axonal growth into an implanted biomaterial scaffold [
33,
34,
35,
36,
37,
38,
39,
40,
41,
42,
43,
44,
45,
46,
47,
48,
49,
50,
51,
52,
53,
54,
55,
56,
57,
58,
60,
61,
62], and thirteen papers showed motor functional recovery following scaffold implant in in vivo studies [
33,
36,
37,
38,
43,
48,
50,
53,
56,
57,
58,
60]. Several articles revealed an anti-inflammatory effect [
38,
46,
48,
50,
54,
59] and angiogenesis [
45,
54,
55,
56,
57,
58] following the implantation of the biomaterial scaffold in the spinal cord.
3.2. Biodegradable Scaffolds
The biodegradable polymers currently used in devices approved by the US Food and Drug Administration provide attractive building blocks for synthetic tissue scaffolds because their biocompatibility has already been established and the regulatory approval process is simple. The biodegradable scaffolds used to treat SCI can be combined with hydrogels. Among the most widely used biodegradable polymers are hydrophobic polyesters such as poly (lactic acid) (PLA), poly (lacticco-glycolic acid) (PLGA) and poly (ε-caprolactone) (PCL). These polymers have been used in sutures and resorbable orthopedic fixation devices because their synthetic fibers provide good mechanical properties and adjustability [
53,
54]. PLA is a biocompatible lactic acid polymer. The neatly arranged PLA microfibers in transplants promoted the regeneration of CNS tissues [
64]. As a product of the reaction between PGA and PLA, which are biodegradable and synthetic polymers, PLGA co-polymer scaffolds show good porosity, hydrophilicity and biodegradability and are usable as drug carriers. One drug delivery device takes the form of a PLGA-based nerve conduit used to control the local delivery of nerve growth factor (NGF) and is applied at the site of the peripheral nerve gap injury [
64]. Biocompatible and biodegradable aliphatic polyester make up PCL scaffolds, and this polyester has been used widely in many biomedical applications including bioactive drug delivery for spinal cord regeneration. Other important biomaterials used in SCI include chitosan and gelatin [
64]. These are frequently implanted surgically into lesions and are synthesized via electrospinning techniques to decrease organic solvent use [
64]. QL6, a biodegradable peptide which self-assembles into nanofiber scaffolds when injected into the spinal cord cavity, has been shown to reduce apoptosis, inflammation and astrogliosis, leading to electrophysiological and behavioral improvements [
7,
65]. Furthermore, when co-transplanted with NPCs, QL6 enhanced graft survival and promoted differentiation towards neuronal and oligodendroglial cell fates [
7,
65]. In another type of biodegradable scaffold, functional sequence SIKVAV-modified PA hydrogels implanted into a rat model of SCI improved histological and functional recovery [
66].
Researchers reviewed the effects of biodegradable scaffolds on pathophysiologiocal events and motor functional recovery when applied for SCI treatment [
66,
67,
68,
69,
70,
71,
72,
73,
74,
75,
76,
77,
78,
79,
80,
81,
82,
83,
84,
85,
86]. Most articles revealed axonal growth into implanted biodegradable scaffolds [
66,
67,
68,
69,
70,
71,
72,
73,
74,
75,
77,
79,
81,
82,
83,
84,
85,
86]. Seven papers showed motor functional recovery following scaffold implantation in in vivo studies [
69,
71,
79,
81,
83,
84,
85]. Several articles revealed an anti-inflammatory effect [
81,
84,
85] and angiogenesis [
66,
71,
72,
82,
84,
85] following the implantation of the biodegradable scaffold in the spinal cord.
3.3. Nano- and Micro-Scale Scaffolds as Instructive Biomaterials for SCI
The recent development of various nanomaterials is offering promising new ways to treat SCI by crossing the blood–spinal cord barrier to deliver therapeutics. Several articles revealed the development of nanomaterials that can modulate inflammatory signals, target inhibitory factors within a lesion and promote axonal regeneration following SCI [
87,
88,
89,
90,
91,
92,
93,
94,
95,
96,
97,
98,
99,
100,
101,
102,
103,
104].
Experimental models for SCI treatment are increasingly being used to study nanoparticles. The extremely diverse composition of nanoparticles includes polymers, metals and metal oxides, silica and biological molecules [
87]. The biocompatibility of polymeric nanoparticles has allowed them to become the most extensively used means of delivering drugs to the spinal cord. Unlike with drugs, topographical cues in the implanted scaffolds at the lesion site can physically guide the extension of new axons [
87,
88,
89,
90,
91]. The electrospinning of nanofibers is advantageous because it permits the production of highly porous 3D scaffolds with a large surface area that aids in cell adhesion [
87]. Spontaneous self-assembling peptides can also form nanofibrous hydrogels that are composed of natural amino acid sequences, rendering them nonimmunogenic, nontoxic and biodegradable [
86,
87]. Self-assembling peptides have an additional advantage in that they can undergo gelation in physiological conditions, and their morphology mimics in vivo ECM [
7,
91]. The ionic complementarity of many common self-assembling peptides allows them to form nanofibrous structures. Several articles reported using other materials for nanoscale scaffolds [
87,
88,
89]. Because of their size, which closely mimics that of ECM proteins, and their high surface area, carbon nanotube nanostructures have shown promising effects in neural regeneration applications. Electrospinning produces micro- and nanofibers that can simulate collagen fibers in the ECM [
88]. RADA16-I hydrogels were used in an experimental SCI model, which proved that self-assembling peptide hydrogels could promote recovery from SCI [
91]. Further development produced functionalized RADA16-I hydrogels with a bone marrow-homing motif (BMHP1) [
91,
99]. These researchers inserted a 4-glycine-spacer into the hydrogels to facilitate scaffold stability and expose more bi motifs. Their results showed that RADA16-I hydrogels can increase cell infiltration, basement membrane deposition and axon regeneration in SCI [
104].
These kinds of nanoscale scaffolds and nanofibers were mainly used for drug delivery systems (DDSs). Therefore, there were only a small number of studies on nanoscale scaffolds applied to SCI treatment [
89,
90,
91,
92,
93,
94,
95,
96,
97,
98,
99,
100,
101,
102,
103,
104]. Researchers reviewed the effects of nanoscale or microscale biomaterial scaffolds on pathophysiological events and motor functional recovery [
89,
90,
91,
92,
93,
94,
95,
96,
97,
98,
99,
100,
101,
102,
103].
4. Biomaterial Scaffolds in Combinatory Treatment Used for DDSs in SCI Treatment
The effects of biomaterial scaffolds in combinatory treatments as DDSs applied for SCI treatment on pathophysiological events and motor functional recovery data are summarized in Table 4.
Table 4. Summary of the included studies and the effect of biomaterial scaffolds in combinatory treatment for SCI.
| |
|
|
|
|
Effect on Pathophysiological Events |
|
| Author, Year |
Location of Injury |
Species |
Combinatory Agent |
Biomaterial Scaffold |
Anti-Inflammation |
Scar/Cavity |
Axon Growth |
Angiogenesis |
Facilitation of Cell Migration |
Motor Functional Recovery |
Furuya T, et al.,
2013 [105] |
Thoracic |
Rat |
bFGF |
Gelatin hydrogel |
NA |
NA |
NA |
NA |
NA |
NA |
Chantal SA, et al.,
2008 [106] |
Thoracic |
Rat |
Methylprednisolone |
Biodegradable PLGA-based nanoparticles |
+ |
+ |
NA |
NA |
+ |
NA |
Jain A, et al.,
2011 [108] |
Thoracic |
Rat |
Constitutively active Cdc42,
Rac1, BDNF |
Microtubule-mediated slow release of BDNF |
+ |
+ |
+ |
NA |
+ |
NA |
Wen Y et al.,
2016 [109] |
Thoracic |
Rat |
Anti-Nogo receptor antibody |
PLGA microspheres
containing BDNF and VEGF |
+ |
+ |
+ |
+ |
+ |
+ |
Chen B, et al.,
2015 [110] |
Thoracic |
Rat |
bFGF |
HEMA-MOETACL hydrogel |
NA |
+ |
+ |
NA |
NA |
+ |
Lin J, et al.,
2019 [114] |
Thoracic |
Rat |
Rehabilitation |
Hybrid fiber-hydrogel scaffold |
+ |
+ |
+ |
NA |
+ |
+ |
Shi Q, et al.,
2014 [115] |
Thoracic |
Rat |
bFGF |
Collagen scaffold |
NA |
+ |
+ |
NA |
+ |
+ |
Wang X, et al.,
2013 [116] |
Thoracic |
Rat |
NT-3 |
Chitosan-based tube scaffold |
NA |
+ |
+ |
NA |
+ |
+ |
Li G, et al.,
2016 [117] |
Thoracic |
Rat and canine |
NT-3 |
Fibrin-coated gelatin sponge scaffold |
+ |
+ |
+ |
NA |
+ |
+ |
Wei YT, et al.,
2010 [118] |
Thoracic |
Rat |
Nogo-66 receptor antibody |
Hyaluronic acid -based hydrogels modified with poly-L-lysine (PLL) |
+ |
+ |
+ |
+ |
+ |
NA |
Bighinati A, et al.,
2020 [119] |
Thoracic |
Rat |
Ibuprofen and triiodothyronine |
PLLA |
+ |
+ |
+ |
NA |
+ |
+ |
Ehsanipour A, et al.,
2021 [120] |
Thoracic |
Mouse |
BDNF |
Hyaluronic acid (HA)-based, spherical microparticle |
+ |
+ |
+ |
NA |
+ |
+ |
Xie J, et al.,
2022 [121] |
Thoracic |
Mouse |
Sonic hedgehog (Shh)
and retinoic acid (RA) |
Magnesium oxide (MgO)/
poly (l-lactide-co-ε-caprolactone) (PLCL) scaffold |
+ |
+ |
+ |
NA |
+ |
NA |
Xi K, et al.,
2020 [122] |
Thoracic |
Rat |
NGF |
Microenvironment-responsive
immunoregulatory electrospun fibers |
+ |
+ |
+ |
NA |
+ |
+ |
Rooney GE, et al.,
2011 [123] |
Thoracic |
Rat |
Dibutyryl cyclic adenosine monophosphate (dbcAMP) |
Oligo [(polyethylene glycol) fumarate] (OPF) hydrogel scaffolds |
NA |
NA |
+ |
NA |
NA |
NA |
Stropkovská A, et al.,
2022 [124] |
Thoracic |
Rat |
Rho-A-kinase inhibitor |
Chitosan/collagen porous scaffold |
+ |
+ |
+ |
NA |
+ |
NA |
Man W, et al.,
2021 [72] |
Thoracic |
Rat |
Hierarchically aligned fibrin hydrogel |
Functionalized self-assembling peptides
(fSAP) |
+ |
+ |
+ |
+ |
+ |
+ |
Smith DR, et al.,
2020 [128] |
Cervical |
Mouse |
IL-10 and NT-3 |
Multiple channel PLG |
+ |
NA |
+ |
NA |
+ |
+ |
Breen BA, et al.,
2017 [130] |
Thoracic |
Rat |
NT-3 |
Injectable collagen scaffold |
NA |
+ |
+ |
NA |
+ |
+ |
Wen Y et al.,
2016 [109] |
Thoracic |
Rat |
AntiNogo, BDNF
and vascular endothelial growth factor |
Hyaluronic acid (HA) hydrogel |
+ |
+ |
+ |
+ |
+ |
+ |
Jain A, et al.,
2006 [129] |
Thoracic |
Rat |
BDNF |
Gelling agarose hydrogels |
NA |
+ |
+ |
NA |
+ |
NA |
This entry is adapted from the peer-reviewed paper 10.3390/ijms24032528