Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Cardiac & Cardiovascular Systems
Obesity is defined when the body mass index (BMI) exceeds a value of 30 kg/m2. It is implicated in slowing improved life expectancy and increasing cardiovascular (CV) risk.
- obesity
- cardiovascular risk
- cardiometabolic complications
- lifestyle interventions
1. Introduction
Obesity is defined when the body mass index (BMI) exceeds a value of 30 kg/m2 [1]. This condition is a growing public health epidemic across the world. Accordingly, the available data suggest that the global burden of obesity has more than tripled since 1975 [2], not only in first-world countries; indeed, recent evidence shows that obesity is spreading in low-and middle-income countries [3]. Specifically, around 42% of adults in the US are obese, while prevalence has increased to about 25% in the United Kingdom [4]. Italy follows this trend with an increase of almost 30% in the adult obese population in the last three decades [5].
2. Relationship between Obesity and Cardiovascular Disease
Obesity is a multifactorial condition influenced by a range of social and environmental factors. While individual behaviors, such as diet and physical activity, play a role in obesity development, broader determinants related to society and the environment also significantly contribute.
The social and environmental determinants of obesity include various aspects.
First, lower socioeconomic status is associated with a higher prevalence of obesity. Factors such as limited access to healthy food options, higher levels of food insecurity, and reduced opportunities for physical activity contribute to the higher obesity rates observed in disadvantaged populations. Socioeconomic disparities can influence dietary choices, availability of resources, and overall health-related behaviors [6].
Another important factor includes the food environment, which consists of the availability and accessibility to healthy food options in communities. Areas characterized by a high density of fast-food outlets, limited access to grocery stores offering fresh produce, and a lack of affordable healthy food options are associated with higher obesity rates. These “food deserts” make it challenging for individuals to make nutritious choices, leading to a higher consumption of energy-dense, nutrient-poor foods [7,8].
Cultural norms and social norms influence and play a role in shaping dietary preferences and behaviors. Societal norms that prioritize large portion sizes, frequent consumption of high-calorie foods, and sedentary lifestyles can contribute to the development of obesity. Additionally, social networks and peer influence can impact food choices and physical activity patterns [9].
Limited education and low health literacy levels can hinder individuals’ understanding of nutrition and the importance of a healthy lifestyle. Insufficient knowledge about healthy food choices, portion sizes, and the benefits of regular physical activity can contribute to obesity. Educational interventions and improving health literacy can empower individuals to make informed decisions and adopt healthier behaviors [10].
Environmental determinants of obesity include the built environment, such as the design and layout of neighborhoods and urban spaces that can affect physical activity levels. Accessible sidewalks, bike lanes, parks, and recreational facilities can promote active lifestyles. Conversely, neighborhoods lacking these features, characterized by limited safety and opportunities for physical activity, can discourage exercise and contribute to sedentary behaviors [11].
Moreover, transportation infrastructure in terms of availability and quality of public transportation systems influence physical activity levels. Communities with inadequate public transportation options may rely more on sedentary modes of transportation, such as cars, leading to reduced opportunities for physical activity [12].
In modern society, advertising and marketing and, in particular, aggressive marketing of unhealthy foods, especially towards children, can contribute to poor dietary choices and increased consumption of energy-dense foods. Exposure to advertisements promoting sugary beverages, fast food, and unhealthy snacks can influence eating behaviors and contribute to obesity [13].
Finally, the work environment, including occupational factors, such as sedentary work environments and long working hours, can limit opportunities for physical activity and contribute to a sedentary lifestyle. Workplace policies and environments that promote physical activity, such as standing desks or workplace wellness programs, can help mitigate the impact of sedentary jobs [14].
Obesity is implicated in recent slowing in improved life expectancy [15] and increases the risk of several chronic diseases (diabetes, hypertension, coronary heart disease) [16,17,18,19]. On average, in the populations studied (largely Caucasians), obesity class III (BMI ≥ 40 kg/m2) shortens life expectancy by approximately 10 years, and obesity class I (BMI 30–34.9 kg/m2) reduces life duration by around 3 years, relative to normal weight, with the number of years lost varying according to age, sex, and severity of obesity [1,20,21]. Specifically, the metabolic syndrome, a concurrence of disturbed glucose and insulin metabolism, overweight and abdominal fat distribution, mild dyslipidemia, and hypertension, is most important because of its association with cardiovascular disease (CVD) [22,23]. More precisely, CV risk is high/very high with obesity class I, very high with class II, and extremely high with class III in Caucasian populations [1]. However, BMI indicates the overall excess body weight, while waist circumference better defines fat distribution and abdominal body fat [24,25]. Additionally, BMI is inadequate for defining body composition and the difference between fat mass and fat-free mass; specifically, the CV risk differs according to the type of ectopic deposition [1,24,26,27]. Specifically, the distribution of adipose tissue has clinical importance, because central adiposity, especially visceral obesity, is more deleterious, while lower body fat deposition may be actually protective [28]. However, the implementation of fat distribution assessment in clinical practice remains a challenge: the instruments used have a high acquisition cost and specialized professionals are needed to use them [29].
Genetic and population-based cohort analysis has revealed a direct relationship between adiposity and other high-risk CV traits, including aortic diseases, HF, deep vein thrombosis, hypertensive heart disease, peripheral artery diseases, and atrial fibrillation (AF) [26,30]. Indeed, several obesity-related mechanisms drive structural, functional, humoral, and hemodynamic alterations believed to underpin the development of CVD (Figure 1) [1]. Specifically, there is a causal association between adipose tissue and CVD: obesity is the causal pathway of several traditional CV risk factors such as atherogenic dyslipidemia, hypertension and diabetes; moreover, obesity-related OSA contributes to CVD risk with the promotion of hypoxia, cardiac dysrhythmias, insulin resistance, and hypertension [31,32,33,34]. Obesity often leads to a deterioration of adipose tissue plasticity, which is linked to fibrosis, inflammation, progenitor cell senescence, and catecholamine resistance [35]. On the other hand, obesity may indirectly cause CVD, mediated through different obesity-associated comorbidities: an excessive increase in body weight prejudices mobility and physical activity and/or worsens musculoskeletal comorbidities and subsequently reduces energy expenditure, resulting in a vicious cycle of weight gain and rising CV risk [36,37,38]; moreover, total blood volume and cardiac output are higher in people with overweight/obesity, contributing to structural and functional changes to the heart and vascular system (left ventricular hypertrophy (LVH), left ventricular diastolic dysfunction and predisposition to HF [37,38,39,40]).
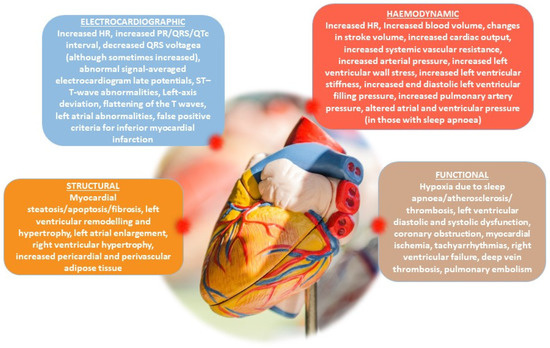
Figure 1. The key electrocardiographic, hemodynamic, structural and functional changes associated with obesity.
These obesity-associated changes in cardiac function have been described as the “cardiomyopathy of obesity” [41]. Sensitive measures of contractile function, such as left ventricular fractional shortening, systolic velocity, and myocardial strain (circumferential and longitudinal), are impaired in the setting of obesity and/or metabolic syndrome [42,43,44,45]. Notably, cardiac functional responses to physiologic perturbations (e.g., exercise), pathologic conditions (e.g., myocardial ischemia) [46,47,48], or pharmacologic stimuli (e.g., catecholamines, glucagon-like-peptide-1 mimetics) [49] are also known to be significantly influenced by an obese/metabolic syndrome phenotype. Investigators in this field have identified relevant and important molecular pathways linking obesity to CV continuum and cardiac dysfunction; in particular, alterations in myocardial Ca2+ handling via changes in the functional expression of SERCA2A and ryanodine (RyR2) receptors [50,51] have been of interest. Also of note is a growing interest in modifications in the regulation of myocardial titin (which influences the passive and restoring force of the cardiac sarcomere and can contribute to hypertrophic signaling) as a potential target or mediator of obesity-associated cardiac dysfunction [50,52,53]. Moreover, it has been reported that weight loss through lifestyle interventions in obese patients with heart failure may result in improvements in the New York Heart Association classification, quality of life and exercise capacity [54].
One added possibility is that progressive vascular disease further influences these heart changes through mechanisms specific to the atherosclerotic process or microvascular dysfunction, independent of the obese state [55,56,57].
There is a growing recognition of the importance of population-level interventions, and individualized care plans with a multidisciplinary approach are recommended [25,58,59]; indeed, the multidisciplinary interventions describe major changes in body composition, and the recurring pattern in clinical trials is an energy reduction and control in the percentage of intake of macronutrients along with the performance of regularly structured exercise [60].
This entry is adapted from the peer-reviewed paper 10.3390/jcdd10080327
This entry is offline, you can click here to edit this entry!
