Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
In animals undergoing veterinary treatment, including therapeutic, quarantine and preventative medicine, their physiology and behaviour are derailed from their normal states and the animal’s choices and comfort are de facto limited. Traditional paradigms of animal welfare do not apply perfectly to animals under veterinary care, including quarantine and preventative medicine. A paradigm separating animal wellbeing from animal welfare is proposed in order to instil much needed clarity of thought and to guide actions in regard to the welfare of animals under human care.
- preventative medicine
- animal welfare
- animal wellbeing
- operant conditioning
1. Reframing the Paradigm to Differentiate Welfare from Wellbeing
The fundamentals of captive animal welfare find their origins in Brambell’s early work introducing the “five freedoms” [1]. This evolved further into the “Five Domains”, aimed at facilitating the systematic, comprehensive and coherent assessment of animal welfare [2][3][4][5]. Over time, models that included the length and complexity of animals’ lives and the role of the caretakers also contributed to give more substance to the topic [6][7][8]. With every attempt at refining the animal welfare models, the definition of welfare widens and the number of criteria used to assess it increases [5][9][10][11][12][13]. To provide adequate welfare under captive conditions many components must be considered, delivered and evaluated. As mentioned by Fraser [14][15], some of these components may be at odds and attempts to improve welfare in one area may diminish it in other areas. Regardless of which models and concepts are adopted, all unequivocally agree that good health is a necessary condition in order for the claim of good animal welfare to be made [14][15][16][17].
Disease processes adversely disrupt the mental and physiological state of the patient. To diagnose and treat diseases or to perform preventative medicine examinations, procedures that are physically and psychologically intrusive and may cause some degree of discomfort, including stress, fear, pain, temporary confinement, various drug effects and side effects, are often necessary. That is why caveats such as “veterinary discretion applies” or “excluding animals under veterinary treatment” are often included, and invariably implied, in documents pertinent to animal welfare, such as husbandry manuals, minimum dimension requirements, etc.
The widely accepted animal welfare framework outlined above, though useful, is not always relatable to animals in zoological collections and even less so to animals undergoing veterinary treatments. These models imply that the welfare of sick animals and even of animals undergoing preventative care is inevitably deficient. This view is not conducive to systemic improvements, and we must move past it to appreciate the importance of preventative medicine programs in animal welfare. Discussions on the welfare of zoo animals are complex and can often lead to intellectual or conversational impasses [12][14][15][18][19][20]. Perhaps this can be traced to the loose interchangeability and the implied equivalence, both in the literature and in the vernacular, of the terms (animal) “welfare” and (animal) “wellbeing” [4][5][9][10][13][15][16][21][22]. Researchers propose to use distinct definitions of animal welfare and animal wellbeing as shown in Table 1.
Table 1. Definitions of animal wellbeing and animal welfare used herein.
| Wellbeing: The Puget Sound Institute [23] conclusions about the nature of human wellbeing can be paraphrased into a suitable working definition of animal wellbeing. | Animal wellbeing includes many aspects of an animal’s everyday life. It encompasses physical comfort, relationships with enclosure mates and caretakers and emotional and physical health. It is a state internal to the animal that is a complex individual response to many internal factors, including demographics, physical health, mental health, emotional health, social grouping dynamics, relationship with other species and staff, sex, age and external factors, such as season, weather, exhibit design, management practices. |
| Welfare: In this paradigm, welfare is external to the animal and is not equivalent to wellbeing nor is it a measure of the animal’s wellbeing and is analogous to human welfare [24] | Animal welfare is the sum total of the management systems in place to mitigate all inevitable negative effects of captivity and to maximize all potential benefits of human care. Animal welfare fulfils moral, ethical and legal duties of those people and organization who have control over many aspects of the lives of the animals under their care |
2. The Role of Preventative Medicine Programs in Improving Animal Welfare Optimizing Animal Wellbeing
By adopting a paradigm that distinguishes between animal welfare and animal wellbeing we can discuss further and with more clarity the role of veterinary medicine in both the animal wellbeing and its welfare. In doing so, preventative medicine emerges as a pillar of zoo animal welfare.
The overall objective of a preventative medicine program is to minimize the chances of health problems developing by preventing their occurrence through the maximization of the chances of detecting health problems early or through averting devastating health outcomes [25] and mitigating complications resulting from the onset of disease [25][26].
Preventative medicine programs are relatively easy to cost, thereby aiding budgeting exercises, fundraising and allocation of funds. A comprehensive preventative medicine program allows for an efficient use of veterinary services, ensuring that there are resources to spare for ad hoc clinical treatments, staff training, exhibit upgrades, broader collection management and other matters that further contribute to animal welfare and to the animals’ wellbeing [8][16][17] in ways that best benefit the animals and the zoological institution. Preventative medicine addresses the needs of the animals and are tailored to the institution’s collection plan, exhibit designs, financial resources and staff expertise, while also weighing other influences, such as political, societal, ethical, cultural and religious values [27]. It is therefore not surprising that preventative medicine programs vary between institutions and are living documents that must be updated on a regular basis to incorporate current and future trends to advance the wellbeing of the collection.
Four broad positive outcomes are expected of a good preventative medicine program. Firstly, the prevention of avoidable diseases, through vaccination programs, regular deworming, balanced species-specific diets, harmonious social grouping and the monitoring of physiological data to detect predictors or prodromic signs of disease. Secondly, the early detection of morbid or degenerative processes that can be corrected to restore health. These include reversible organ systems impairment, dental pathologies, cataracts, benign neoplasia, nutritional imbalances, abnormal development issues, etc. Thirdly, as age advances or if premature diseases occur, preventative medicine programs are also tasked with designing and dispensing treatments to lessen the burden of morbid or degenerative processes that cannot be corrected fully. These include irreversible organ systems impairment, malignancies, age-related skeletal pathologies, etc. [25][26]. Lastly, euthanasia, practised to prevent prolonged suffering on the way to unavoidable death.
The financial, human and technical resources invested in order to maximise the outcomes must balance cost and the expected benefits relative to the risks [26][27].
Figure 1 shows a selection of preventative medicine procedures presented within a frame with four quadrants outlined by a vertical axis representing increasing cost or risk and a horizontal axis representing increasing potential benefits. Planned preventative measures can be positioned amongst the four quadrants. For obvious reasons there would be very few procedures with an expected low benefit regardless of risks or cost. Investigations that are able to yield a large benefit are the most desirable. Managerial efforts (animal welfare) devoted to reducing the risks and cost of veterinary procedures, such as new technologies, staff training and training animals for voluntary medical procedures (see more on this below), will improve the wellbeing of the animals [8][19].
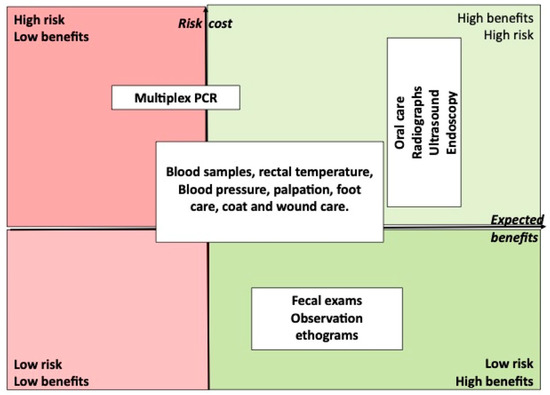
Figure 1. Selected procedures for the purpose of preventative medicine can be positioned within four quadrants to visualize the risk/benefit and cost benefit ratios. The technique used to carry out a procedure affects its safety and cost. The same procedure may have different benefits in different species. Therefore, the same procedure may occupy more than one quadrant. Most procedures should have a high potential benefit.
Procedures planned as part of the preventative medicine program reflect the institutional commitment to and understanding of an animal’s needs. Planned procedures should detect reliable predictors or indicators of disease, leading to appropriate veterinary or management decisions, and they must be worth the inherent risks or cost [26]. Ambiguous and inaccurate test results can lead caretakers down the wrong path. Tests performed on apparently healthy individuals for the purpose of the early identification of underlying diseases are of variable utility, depending on the species or situation. As an example, a routine complete blood count (CBC) and biochemistry offers much insight in dolphins but that is seldom the case in tortoises. Diagnostic imaging should also be used judiciously, especially when restraint or anaesthesia is required. For example, chest and abdominal radiographs are very informative in small and medium-sized patients but in large patients they can be misleading, and they are best used as special examinations during clinical investigations in symptomatic animals rather than performed routinely on apparently healthy ones.
Manual or chemical restraint is often needed to carry out preventative medicine examinations. These inherently carry a risk of injury or death that are higher in some species than others, such as giraffes or pinnipeds. The risks are also influenced by other circumstances, such as having to dart an animal on a tall tree versus injecting it in a squeeze cage, or the technical expertise and experience of the staff. These risks need careful consideration and decisions must be justified based on evidence and consensus. The following example illustrates this: A zoo’s veterinary records reveal that, over the last two decades, two elephant seals of over eighteen years of age have succumbed to hepatic malignant neoplasia, from a total of 10 deaths during that same period. The same records reveal that the anaesthetic death rate for elephant seals of all ages is 8%. Contrast computerised tomography (CT) may allow the detection of small masses at a stage where a curative intervention may still be possible. A meeting between caretakers, veterinarians and higher management is arranged. The high risk of anaesthetic deaths, the low incidence of tumours in young animals, the real benefits of early detection and the cost of CT are discussed. Ultimately the preventative medicine program of the elephant seals is expanded with three items: a contrast computerised tomography (CT) scan under general anaesthesia every alternate year for all seals over the age of 16 years; a target for all elephant seals to voluntarily allow liver ultrasound by the age of 8 years and a review of the outcome of the changes to the elephant seals’ preventive medicine program after 3 years. The expansion of the preventive medicine is an immediate improvement of the animal welfare that is expected to present all the seals with a better opportunity to thrive and do well. External to the animals, but with the animal wellbeing in mind, using a combination of factual data and suppositions, the managers decided to improve animal welfare balancing risks, costs and expected benefits to the animals.
The considerable and ongoing advances made in the last four decades in the chemical immobilization of zoo and wildlife species have made both routine and ad hoc examinations safer for many individuals of many species. This progress has contributed significantly to improved husbandry and better veterinary practices in both the clinical and the preventative medicine fields. Preventative medicine programs require veterinary staff to spend more time with caretakers and healthy animals, multiplying the opportunities for mutual learning and positive interactions, creating deeper bonds and trust.
Table formats are well suited to scheduling the species-specific and individuals-specific requirements that must feature in the preventative medicine program. Table 2 offers an example for kinkajous, a subsection of the carnivorous mammals section of a preventative table format used by the authors.
Table 2. Example of a working document capturing the scope and schedule of a preventative medicine program for a group of two males and one female Kinkajou (Potos flavus).
| Prophylactic Plan 2023 | Procedure | Remarks | Vet’s Comments/Follow up Action |
|---|---|---|---|
| Kinkajous: 2 males 1 female |
GA for CT and general exam every 3 years | Voluntary, lying immobile in transparent box | Due in mid-2023 |
| Distemper, FRCPV and Rabies vaccination every 3 years. | All tolerate vaccines well; all are stable for voluntary injection | FRCPV and Rabies for all three due January 2023 | |
| KJ23 only: suprelorin implant in June and January (4.7 mg) | Last implant in June 2022 | Due in January 2023. To be confirmed, advise surgical neuter if no plan for breeding | |
| Heartworm prevention | Monthly oral Ivermectin | ||
| Faecal sample | Once a year for parasitology | Last quarter 2023 | |
| Full body X ray under training ad hoc | Behaviour already acquired for all, to be maintained | Quarterly animal training on site with vet staff | |
| Abdominal ultrasound | KJ20 and KJ25 voluntary. KJ23 not fully trained | Quarterly animal training for KJ20 and KJ25, monthly for KJ23. Obtain at least one good yearly examination | |
| Dental visual exam under training | Voluntary, all stable to open mouth on command | January and June 2023 |
This entry is adapted from the peer-reviewed paper 10.3390/ani13142299
References
- Brambell, F.W.R. Report of the technical committee to enquire into the welfare of animals kept under intensive livestock husbandry systems. 1965. Brambell Committee. In Report of the Technical Committee to Enquire into the Welfare of Livestock Kept under Intensive Conditions; Command Paper 2836; Her Majesty’s Stationery Office: London, UK, 1965.
- Webster, J. Animal Welfare: A Cool Eye Towards Eden; Assessment of animal welfare: The five freedoms; Blackwell Science: Oxford, UK, 1994; pp. 10–14. ISBN 978-0-632-03928-9.
- Mellor, D.J.; Reid, C.S.W. Improving the Well-Being of Animals in the Research Environment; Australian and New Zealand Council for the Care of Animals in Research and Teaching (ANZCCART): Adelaide, Australia, 1994; ISBN 0646181165.
- Ryder, R.D. Measuring Animal Welfare. J. Appl. Anim. Welf. Sci. 1998, 1, 75–80.
- Mellor, D.J.; Beausoleil, N.J.; Littlewood, K.E.; McLean, A.N.; McGreevy, P.D.; Jones, B.; Wilkins, C. The 2020 Five Domains Model: Including Human–Animal Interactions in Assessments of Animal Welfare. Animals 2020, 10, 1870.
- Whitham, J.C.; Wielebnowski, N. Animal-based welfare monitoring: Using keeper ratings as an assessment tool. Zoo Biol. 2009, 28, 545–560.
- Brando, S.; Buchanan-Smith, H.M. The 24/7 approach to promoting optimal welfare for captive wild animals. Behav. Process. 2018, 156, 83–95.
- Cole, J.; Fraser, D. Zoo Animal Welfare: The Human Dimension. J. Appl. Anim. Welf. Sci. 2018, 21, 49–58.
- Mellor, D.J.; Beausoleil, N.J. Extending the ‘Five Domains’ model for animal welfare assessment to incorporate positive welfare states. Anim. Welfare 2015, 24, 241–253.
- Green, T.C.; Mellor, D.J. Extending ideas about animal welfare assessment to include ‘quality of life’ and related concepts. New Zealand Vet. J. 2011, 59, 316–324.
- Mellor, D.J. Updating Animal Welfare Thinking: Moving beyond the “Five Freedoms” towards “A Life Worth Living”. Animals 2016, 6, 21.
- Mellor, D.J. Operational details of the five domains model and its key applications to the assessment and management of animal welfare. Animals 2017, 7, 60.
- Keeling, L.J. Indicators of good welfare. Encyclopedia of Animal Behavior; Choe, J.C., Ed.; Elsevier Academic Press: Amsterdam, The Netherlands, 2019; pp. 134–140.
- Fraser, D. Understanding animal welfare. Acta Vet. Scand. 2008, 50 (Suppl. 1), S1.
- Fraser, D. Assessing animal welfare: Different philosophies, different scientific approaches. Zoo Biol. 2009, 28, 507–518.
- Kagan, R.; Carter, S.; Allard, S. A Universal Animal Welfare Framework for Zoos. J. Appl. Anim. Welf. Sci. 2015, 18 (Suppl. 1), S1–S10.
- Greggor, A.L.; Vicino, G.A.; Swaisgood, R.R.; Fidgett, A.; Brenner, D.; Kinney, M.E.; Farabaugh, S.; Masuda, B.; Lamberski, N. Animal welfare in conservation breeding: Applications and challenges. Front. Vet. Sci. 2018, 5, 323.
- Maple, T.L. Toward a science of welfare for animals in the zoo. J. Appl. Anim. Welf. Sci. 2007, 10, 63–70.
- Brando, S.; Broom, D.M.; Acasuso-Rivero, C.; Clark, F. Optimal marine mammal welfare under human care: Current efforts and future directions. Behav. Processes 2018, 156, 16–36.
- Paul-Murphy, J.; Molter, C. Overview of animal welfare in zoos. In Fowler’s Zoo and Wild Animal Medicine; Elsevier Inc.: Amsterdam, The Netherlands, 2019; Volume 9, pp. 64–72.
- Fisher, M.W. Defining animal welfare—Does consistency matter? New Zealand Vet. J. 2009, 57, 71–73.
- Bloomsmith, M.A. Measuring zoo animal welfare. J. Appl. Anim. Welf. Sci. 2009, 12, 273–275.
- Puget Sound Science Review. Puget Sound Institute, Univeristy of Washington, Ed Conway-Cranos T & Skewgar, E. Available online: https://www.eopugetsound.org/science-review/section-3-nature-human-well-being (accessed on 15 April 2023).
- BRIGGS, A.S.A. The Welfare State in Historical Perspective. Eur. J. Sociol. Arch. Eur. Sociol. Eur. Arch. Soziologie 1961, 2, 221–258.
- Crittenden, F.; Fang, C. Preventive Medicine, introduction. YJBM 2021, 94, 1–3.
- Goodell, S.; Cohen, J.; Neuman, P. Cost savings and cost-effectiveness of clinical preventive care. Synth. Project. Res. Synth. Rep. 2009, 18, 48508.
- Maciosek, M.V.; Edwards, N.M.; Coffield, A.B.; Flottemesch, T.J.; Nelson, W.W.; Goodman, M.J.; Solberg, L.I. Priorities among effective clinical preventive services: Methods. Am. J. Prev. Med. 2006, 31, 90–96.
This entry is offline, you can click here to edit this entry!
