Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Indoor air pollution can be treated with techniques such as chemical purification, ventilation, isolation, and removing pollutions by plants (phytoremediation). Indoor air pollution can be treated with techniques such as chemical purification, ventilation, isolation, and removing pollutions by plants (phytoremediation).
- environmental technology
- biofiltration
- phytoremediation
- indoor air pollution
- VOC
1. Introduction
Air pollution is one of the major issues in urban areas, especially in developing countries [1]. The human population in urban areas is expected to reach 8.5 billion by 2030 and 9.7 billion by 2050 [2]. The critical factors in increasing the air pollution level include heavy traffic, industrialization, and combustion of fossil fuels for heating [3][4]. Another source of air pollution is chemical complexes used in pesticides such as insecticides, fungicides, household cleaning materials, fabrics, paints, sofa and etc., which are common all over the world [5]. Waste treatment plants (WTP) can be a cause of pollution in the atmosphere and are insalubrious and reduce personal well-being. Formaldehyde and volatile organic compounds (VOC) are among the pollutants from WTP [6][7]. These pollutants could be either in water, soil, or in the air, but they should be considered as important atmospheric pollutant sources as eventually they partially evaporate into the air [5]. Global Health Observatory (GHO) data suggest that more than 50% of the people in 2014 lived in cities, and this percentage will increase in the future. In Europe, urban areas continue to grow fast and broaden into the surrounding regions [8][9].
Usually, indoor air pollution is worse than outdoor air pollution, especially in industrialized areas, both in terms of concentration of pollutants as well as their effects on health [3][10][11].
CO, NO2, SO2, PM2.5, ozone as well other VOC such as BTEX (benzene, toluene, ethylbenzene and xylene) are in the scope of indoor air pollutants. These pollutants can be in much higher concentrations indoors, especially when there is no air conditioning in a building. The studies reviewed are from different part of the world, including low-income households in Europe [11] and recent United States Environmental Protection Agency (EPA) studies on USA schools [12].
One might ask why CO2 is considered and studied as indoor air pollution while it is hardly concerned as a health problem in itself. Although an indoor CO2 level of 600 ppm provides adequate air quality, a 1000 ppm indicates poor air quality [13]. A study by [13] shows that even at low and moderate CO2 levels (1000 and 2500 ppm), significant decrements occur in decision-making performance. Furthermore, the level of indoor CO2 can be considered as a reasonable indicator of the effectiveness of the air conditioning system. In other words, high CO2 concentrations can be linked to higher concentrations of other indoor contaminants, which result from poor ventilation [14].
Generally, the concentration of indoor pollution is up to 5 times more than outdoor and in some cases reaches up to 100 times [15][16]. For example, Vasile et al. [17] showed that the concentration of CO2 in the kitchen and bedrooms of the housing sector in Central and Eastern Europe could be three times higher indoors than those outdoors. Another example is the work of Cheng et al. [18], showing that the indoor CO2, formaldehyde and Total volatile organic compounds (TVOCs) concentration is higher than the outdoor concentration in multi-story department store buildings in seven cities of China.
In 2012, the World Health Organization (WHO) reported 4.3 million premature deaths due to indoor air pollution [19][20][21]. Nowadays, people spend most of their times indoors, such as in the home, office, and laboratory. In the case of elders, this is very significant [19][21]. For example, in North America, elders spend approximately 90% of their living in the indoors area [22][23][24]. Segalin et al. [25] investigated the life of older adults who spend most of their time in the indoor environment and showed that there is a high exposure to particulate matter [26], especially fine particles.
As the price of cooling and heating is increasing due to increasing prices of energy in many countries [4][23][27] most people attempt to build their houses and offices more airtight to make a saving in the energy bills [22][27], which could result in accumulation of indoor air pollutants. The air that circulates in our homes, schools, and offices, which have low ventilation rate can be more polluted than the outdoor air and is becoming a principal health threat [3][22][28]. The associated time spent indoors against outdoors will influence the intake of indoor pollutants [29][30][31].
The concentrations of indoor air pollutants depend on both indoor and outdoor discharge rate of pollutant sources (Figure 1). To be more specific, the following parameters affect the indoor air quality: rate of air infiltration, ventilation type (mechanical vs. natural), building position and direction, number of covering walls and windows, surrounding space and boundary, the speed and direction of wind, indoor-outdoor temperature gradient, and air-conditioning system type (e.g., heating, ventilation, air-conditioning system) [32][33][34].
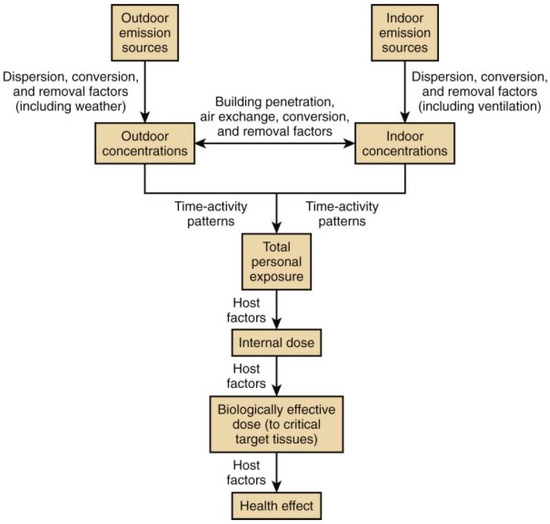
Figure 1. Relations between outdoor and indoor air pollution and health effects [30].
2. Indoor Air Pollution: Sources and Their Health Effects
Indoor air pollutants include a wide variety of materials, including organic and inorganic pollutants [3], and particulate matter (PM) [28][35][36]. Some of the more important pollutants are briefly discussed below.
2.1. Inorganic Pollutants
Nitrogen oxides are combustion by-products, produced by the burning of natural gas or oil in oxygen-rich environments such as kitchen stoves and ovens, furnaces, and unventilated gas and kerosene heaters. When a fireplace or wood stove is used, some of these pollutants will enter the room. Cracks in the stovepipe, downdrafts, or wood spillage from a fireplace can worsen the condition [3][37]. A recent study shows that nitrogen dioxide (NO2) in kitchens with a gas cooker were three times higher than outdoors [22]. Adverse effects of NO2 exposure are breathing symptoms, bronchoconstriction, growing of bronchial reactivity, airway painfulness, and reduced immune protection leading to increased susceptibility to respiratory infection [9]. High levels of NO2 are linked to an increased sequence of respiratory symptoms and poorer respiratory action in asthmatic children [38].
Trace elements: generally, toxic trace elements are related to PM and are Fe, Al, Mg, Zn, Co, As, Cr, Cd, Mn, Cu, Ni, and Pb. Trace elements such as Mg, Fe, and Al are greatly released from crustal sources such as parent rocks, metallic minerals, seas, and oceans. Fossil fuel combustion, forest and biomass burning and metal processing are also sources releasing many trace elements [28]. These toxic pollutants either are ingressed from outside of the buildings or generated inside because of fossil fuel combustion.
Mercury (Hg) is a persistent, poisonous, and bio-accumulative heavy metal. It can discharge into the atmosphere from a diversity of anthropogenic and natural sources. A substantial amount of observed mercury is transmitted from the burning process of fuels (36%) and biomass (33%) [39][40].
Ozone can cause the muscles in the airways to constrict, trapping air in the alveoli. This leads to wheezing and shortness of breath. Ozone has a strong, pungent odor. The source of ozone in a building is electrostatic copying devices, mercury-raised light bulbs, and electrostatic air cleaners [3][41][42].
Inhalable particulate matter is classified into three groups according to their sizes: coarse particles (2.5 < dp < 10 μm), fine particles (≤2.5 μm) and ultrafine particles (UFP, <0.1 μm) [43][44]. Fine particles are more potent when inhaled in comparison to the coarse fraction since they can penetrate more into the lungs. UFP can penetrate alveoli and enter the blood, which can be very harmful. Numerous epidemiological and clinical research works exist that establish the relationship between particulate matter [26] exposure and different health effects and references therein [45]. The Department for Environment, Food and Rural Affairs (Defra, UK) estimated that the health costs incurred by particulate matter (PM10) pollution in the UK is in the range of £9.1 and £21.4 billion per year [45][46][47]. Sources that can increase the PM10 concentration are Earth’s crust elements that are the result of oil burning and human activities, and motor vehicles [48]. An increase in the exposure to PM leads to increased hospital admissions, certainly in the sensitive group cohorts such as the old and individual with cardiopulmonary and respiratory illness. PM concentration inside a building is basically governed by indoor sources of fine particles, outside PM concentration, the rate of air circulation, and the particles’ depositional speed [45]. Bozlaker et al. [49] and Mohammadyan et al. [50] studied the relation between indoor and outdoor particulate materials. The result shows the indoor concentration PM2.5 is usually higher than outdoor [45].
Asbestos exposure for an extended period of time could lead to lung cancer known as mesothelioma and asbestosis. Insulation and other building materials such as floor tiles, drywall compounds, and reinforced plasters are sources of asbestos [51].
2.2. Organic Pollutants
VOCs
VOCs are chemicals that mostly vaporized easily at room temperature, and their concentration is higher than other pollutants in the indoor air. Aerosols, cleaning agents, polishes, varnishes, paints, pressed-wood products, and pesticides are some of the VOC sources at homes and offices [3][52][53].
Toluene and ethylbenzene: toluene exists in many materials such as gasoline, paints, and fingernail polish. Ethylbenzene is also present in paints, lacquers, and insecticides. These compounds are a hazard for human health and can have adverse effects on the nerve, liver, kidneys, and respiratory system [9][54].
Formaldehyde is a class of aldehydes that is a colorless gas. The source of formaldehyde is different building materials, household products, or combustion processes. Indoor sources include pressed-wood products, including particleboard, paneling, fiberboard, resins, and wallboard as well as textiles, such as carpet backings, drapes, and upholstery fabrics, linens, and clothing; urea–formaldehyde foam insulation; adhesives; paints; coatings; and carpet shampoos plus tobacco smoke. Decreasing ventilation rate will increase the level of formaldehyde [53][55][56]. Formaldehyde enters the body via the respiratory system, skin, or gastrointestinal tract. Formaldehyde absorbed in the respiratory tract is rapidly metabolized. Formaldehyde exposure could cause respiratory symptoms, reductions in lung function, headaches, and asthma, and it can affect the nervous system [53].
Carbon dioxide and carbon monoxide result from poorly ventilated kitchens, rooms over garages, and unvented combustion appliances (stoves, ovens, heaters, and the presence of tobacco smoke) [10]. Sneezing, coughing, and minor eye irritation are symptoms of exposure [51].
Acetaldehyde is toxic to the cilia of respiratory epithelia and may interfere with respiratory clearance mechanisms. Acetaldehyde is also a central nervous system depressant and a proven carcinogen in animals, and a potential carcinogen in humans. The acetaldehyde source of indoor is construction materials, furnishing materials such as vinyl, polyvinyl chloride (PVC) and rubber floorings, nylon carpets, particleboard furniture, plywood, fiberboard, flooring adhesives, wood paneling, caulking, paint removers, and other consumer products. Also, it emitted by printers and photocopiers [9][57].
Acrolein is a very potent eye irritant, causing lacrimation at concentrations of approximately 2 mg/m3. At high concentrations, acrolein can cause significant lung injury, including dyspnea, asthma, congestion, edema, and persistent respiratory insufficiency with decreased lung function [9].
Naphthalene is a volatile white solid. It is an aromatic hydrocarbon, including a fused pair of benzene rings [9]. Naphthalene is mostly used in toilet deodorant and also as moth repellents. Extended exposure to a large amount of naphthalene may damage or destroy some of the red blood cells; 10 parts per million (ppm) for the level of naphthalene in workplace air over an 8 h workday is the limit set by the Occupational Safety and Health Administration (OSHA) [58].
Trichloroethylene (TCE) is a clear, non-flammable liquid used mainly for vapor degreasing and cold cleaning of manufactured metal parts and to a less degree as a solvent for a variety of organic materials. The primary sources of TCE in the indoor air include varnishes, finishes, lubricants, adhesives, wood stains, paint removers, cleaning liquids containing TCE, and contaminated food and water [9]. The EPA classified the TCE as carcinogenic to humans [59]. TCE can affect the central nervous system (CNS), eyes, kidney, liver, lungs, mucous membranes, and skin [60].
Tetrachloroethylene (PCE) is a colorless liquid mostly used for dry cleaning fabrics, as a solvent for organic materials, and to degrease metal parts in the automotive and other metalworking industries. Another source of PCE is dry cleaned clothes. Exposure to PCE vapor could cause damage to the following organs: kidneys, liver, the peripheral nervous system [9], upper respiratory tract, skin, the central nervous system (CNS) [61].
The WHO has categorized indoor VOCs into various classes, as seen in Table 1. Based on the available literature, some of the major sources of VOCs are listed in Table 2 in which a guideline for the maximum exposure is provided. It should be noted that the concentration of TVOC should not exceed 300 μg/m3 [9][62]. Furthermore, there is no safe level of exposure for some of these pollutants (asbestos and radon).
Table 1. World Health Organization (WHO) classification of volatile organic compounds (VOCs) adapted from [63].
| Category Description | Acronym | Boiling Point Range, °C |
|---|---|---|
| Very volatile (gaseous) organic compounds | VVOCs | <0 to 50 |
| Volatile organic compounds | VOCs | 50 to 240 |
| Semi-volatile organic compounds | SVOCs | 240 to 380 |
| Organic compounds associated with particulate matter: Particle-bound organic compounds | POCs | >380 |
Table 2. Common indoor sources of volatile organic compounds adapted from the WHO [64].
| Class | Name | Maximum Exposure Guidelines | |
|---|---|---|---|
| Organic pollutant | Carbon monoxide | 100 mg/m3 | 15 min |
| 60 mg/m3 | 30 min | ||
| 30 mg/m3 | 1 h | ||
| 10 mg/m3 | 8 h | ||
| Organic pollutant | Formaldehyde | 0.1 mg/m3 | 30 min |
| Organic pollutant | Tetrichloroethylene (TCE) | 0.25 mg/m3 | Annual |
| Organic pollutant | Tetrachloroethylene (PCE) | 100 ppm | 3 h |
| Organic pollutant | Toluene | 0.26 mg/m3 | 1 week |
| Inorganic pollutant | Asbestos | 500 F*/m3 b | -- |
| Radioactive pollutant | Radon | >1 Becquerel/m3 c | -- |
| Classical pollutant | Nitrogen dioxide | 200 μg/m3 | 1 h |
| 40 μg/m3 | Annual | ||
| 53 ppb a | Annual | ||
| Ozone | 120 μg/m3 | 8 h | |
| 0.08 ppm a | 1 h | ||
Polybrominated diphenyl ethers (PBDEs) include materials such as plastics, television sets, textiles, synthetic building materials, computers, and cars. Human exposure to PBDEs includes food consumption and ingestion of polluted air and house dust. Studies show that computer clerks have higher PBDE levels in their blood than others. It should be noted that exposure to PBDEs via inhalation is of minor importance [66]. PBDEs are toxins that disrupt developing fetuses and infants. PBDEs can act as endocrine disruptors by the change of thyroid hormones homeostasis [67][68].
Insecticide affects the environment, depending on their physical and chemical properties [5]. For example, each year, malaria is responsible for 584,000 deaths worldwide. Hence, indoor residual spraying (IRS) is an important source of Insecticide indoor pollution [69].
Radon (222Rn) is a radioactive gas that is odorless and colorless. It is the result of the radioactive decay of radium-226. The soil and rock in the building can be the primary source of radon in indoor air. Another source of indoor radon is groundwater—Rn concentration changes with seasonal and daily variation [70]. A high concentration of radon leads to lung cancer [71].
Tobacco smoke is the largest source of air pollutant in indoor environments. It has more than 4000 chemical compositions, which could lead to pneumonia and bronchitis in childhood [9][72][73].
Biomass fuels and coal are a source of energy for cooking and heating. Almost 3 billion people use biomass (wood, charcoal, crop residues, and animal dung) and coal worldwide as their primary and other household needs [74]. The CO2 and NO2, arsenic, fluorine and organic matter such as polycyclic aromatic hydrocarbons emit from biomass and coal combustion. Chronic obstructive pulmonary disease, asthma, respiratory infections, lung cancer and eye diseases are the exposure effects of biomass and coal [75][76].
This entry is adapted from the peer-reviewed paper 10.3390/atmos12040473
References
- Kumar, P.; Hama, S.; Omidvarborna, H.; Sharma, A.; Sahani, J.; Abhijith, K.; Debele, S.E.; Zavala-Reyes, J.C.; Barwise, Y.; Tiwari, A. Temporary reduction in fine particulate matter due to ‘anthropogenic emissions switch-off’ during COVID-19 lockdown in Indian cities. Sustain. Cities Soc. 2020, 62, 102382.
- Saha, S.; Monroe, A.; Day, M.R. Growth, yield, plant quality and nutrition of basil (Ocimum basilicum L.) under soilless agricultural systems. Ann. Agric. Sci. 2016, 61, 181–186.
- Aller, M. Environmental Laws and Regulations. In Library of Congress Cataloging; CRC Press LLC: Boca Raton, FL, USA, 1999.
- Pandey, A.K.; Pandey, M.; Tripathi, B. Air Pollution Tolerance Index of climber plant species to develop Vertical Greenery Systems in a polluted tropical city. Landsc. Urban. Plan. 2015, 144, 119–127.
- Sanjuán-Herráez, D.; Rodríguez-Carrasco, Y.; Juan-Peiró, L.; Pastor, A.; De la Guardia, M. Determination of indoor air quality of a phytosanitary plant. Anal. Chim. Acta 2011, 694, 67–74.
- Gallego, E.; Roca, F.J.; Perales, J.F.; Guardino, X.; Gadea, E.; Garrote, P. Impact of formaldehyde and VOCs fromwaste treatment plants upon the ambient air nearby an urban area. Sci. Total Environ. 2016, 568, 369–380.
- Marć, M. Problems and challenges associated with estimating the emissions of organic compounds from indoor materials. Trac Trends Anal. Chem. 2017, 97, 297–308.
- Sriprapat, W.; Thiravetyan, P. Efficacy of ornamental plants for benzene removal from contaminated air and water: Effect of plant associated bacteria. Int. Biodeterior. Biodegrad. 2016, 113, 262–268.
- Schwela, P.D. Indoor Air; Kotzias, D., Ed.; Wiley Online Library: Hoboken, NJ, USA, 2005; Volume 3, pp. 475–489.
- Schwela, D. Pollution, Indoor Air A2—Wexler, Philip. In Encyclopedia of Toxicology, 3rd ed.; Oxford University Press: Oxford, UK, 2014; pp. 1003–1017.
- Kolokotsa, D.; Santamouris, M. Review of the indoor environmental quality and energy consumption studies for low income households in Europe. Sci. Total Environ. 2015, 536, 316–330.
- EPA. Why Indoor Air Quality Is Important to Schools. Available online: https://www.epa.gov/iaq-schools/why-indoor-air-quality-important-schools (accessed on 5 March 2021).
- Satish, U.; Mendell, M.J.; Shekhar, K.; Hotchi, T.; Sullivan, D.; Streufert, S.; Fisk, W.J. Is CO2an Indoor Pollutant? Direct Effects of Low-to-Moderate CO2Concentrations on Human Decision-Making Performance. Environ. Health Perspect. 2012, 120, 1671–1677.
- Pereira, M.; Tribess, A.; Buonanno, G.; Stabile, L.; Scungio, M.; Baffo, I. Particle and Carbon Dioxide Concentration Levels in a Surgical Room Conditioned with a Window/Wall Air-Conditioning System. Int. J. Environ. Res. Public Health 2020, 17, 1180.
- Torpy, F.; Irga, P.; Burchett, M. Profiling indoor plants for the amelioration of high CO2 concentrations. Urban For. Urban Green. 2014, 13, 227–233.
- Australia, E. BTEX Personal Exposure Monitoring in Four Australian Cities; Technical Report No. 6; Common-Wealth of Australia: Sydney, Australia, 2003; pp. 1–62.
- Vasile, V.; Petran, H.; Dima, A.; Petcu, C. Indoor Air Quality—A Key Element of the Energy Performance of the Buildings. Energy Procedia 2016, 96, 277–284.
- Cheng, L.; Li, B.; Cheng, Q.; Baldwin, A.N.; Shang, Y. Investigations of indoor air quality of large department store buildings in China based on field measurements. Build. Environ. 2017, 118, 128–143.
- Kazemi, A.; Ghorbanpour, M. Introduction to Environmental Challenges in All Over the World. In Medicinal Plants and Environmental Challenges; Springer: Cham, Switzerland, 2017; pp. 25–48.
- Luengas, A.T.; Hort, C.; Platel, V.; Elias, A.; Barona, A.; Moynault, L. Removal of traces of toluene and p-xylene in indoor air using biofiltration and a hybrid system (biofiltration + adsorption). Environ. Sci. Pollut. Res. 2017, 24, 10674–10684.
- Katsoyiannis, A.; Bogdal, C. Interactions between indoor and outdoor air pollution—Trends and scientific challenges. Environ. Pollut. 2012, 169, 150–151.
- Veetil, D.S.P. Air Pollution: Sources and Effects in Urban Areas and How it Affect the Investment and Economy. Envirocities Emagazine 2012, 3, 5.
- Wetzel, T.A.; Doucette, W.J. Plant leaves as indoor air passive samplers for volatile organic compounds (VOCs). Chemosphere 2015, 122, 32–37.
- Śmiełowska, M.; Marć, M.; Zabiegała, B. Indoor air quality in public utility environments—A review. Environ. Sci. Pollut. Res. 2017, 24, 11166–11176.
- Segalin, B.; Kumar, P.; Micadei, K.; Fornaro, A.; Gonçalves, F.L. Size–Segregated particulate matter inside residences of elderly in the Metropolitan Area of São Paulo, Brazil. Atmos. Environ. 2017, 148, 139–151.
- PM, V. Processing and Characterizations: State-of-the-Art and New Challenges. Nanostruct. Polym. Membr. 2016, 1, 1.
- Thatcher, A.; Milner, K. Is a green building really better for building occupants? A longitudinal evaluation. Build. Environ. 2016, 108, 194–206.
- Ugranli, T.; Gungormus, E.; Sofuoglu, A.; Sofuoglu, S. Indoor Air Quality in Chemical Laboratories. In Elsevier Comprehensive Analytical Chemistry; Elsevier: Amsterdam, The Netherlands, 2016; pp. 859–878.
- Arif, M.; Katafygiotou, M.; Mazroei, A.; Kaushik, A.; Elsarrag, E. Impact of indoor environmental quality on occupant well-being and comfort: A review of the literature. Int. J. Sustain. Built Environ. 2016, 5, 1–11.
- Balmes, J.R.; Eisner, M.D. Indoor and outdoor air pollution. In Murray & Nadel’s Textbook of Respiratory Medicine E-Book; Elsevier: Amsterdam, The Netherlands, 2016; p. 2208.
- Chandrappa, R.; Kulshrestha, U.C. Sustainable Air Pollution Management Theory and Practice; Hamburg, U.F., Rulkens, W.H., Salomons, W., Eds.; Springer: Cham, Switzerland, 2016.
- Goyal, R.; Khare, M.; Kumar, P. Indoor air quality: Current status, missing links and future road map for India. J. Civ. Environ. Eng. 2012, 2, 2–4.
- Nazaroff, W.W. Exploring the consequences of climate change for indoor air quality. Environ. Res. Lett. 2013, 8, 015022.
- Leung, D.Y.C. Outdoor-indoor air pollution in urban environment: Challenges and opportunity. Front. Environ. Sci. 2015, 2.
- Kiurski, J.S.; Marić, B.B.; Aksentijević, S.M.; Oros, I.B.; Kecic, V.S.; Kovačević, I.M. Indoor air quality investigation from screen printing industry. Renew. Sustain. Energy Rev.. 2013, 28, 224–231.
- Jovanović, M.; Vučićević, B.; Turanjanin, V.; Živković, M.; Spasojević, V. Investigation of indoor and outdoor air quality of the classrooms at a school in Serbia. Energy Environ. Sci. 2014, 77, 42–48.
- Dėdelė, A.; Miškinytė, A. Seasonal variation of indoor and outdoor air quality of nitrogen dioxide in homes with gas and electric stoves. Environ. Sci. Pollut. Res. 2016, 23, 17784–17792.
- Cibella, F.; Cuttitta, G.; Della Maggiore, R.; Ruggieri, S.; Panunzi, S.; De Gaetano, A.; Bucchieri, S.; Drago, G.; Melis, M.R.; La Grutta, S.; et al. Effect of indoor nitrogen dioxide on lung function in urban environment. Environ. Res. 2015, 138, 8–16.
- Shen, H.; Tsai, C.M.; Yuan, C.S.; Jen, Y.H.; Ie, I.R. How incense and joss paper burning during the worship activities influences ambient mercury concentrations in indoor and outdoor environments of an Asian temple. Chemosphere 2017, 167, 530–540.
- Loupa, G.; Polyzou, C.; Zarogianni, A.M.; Ouzounis, K.; Rapsomanikis, S. Indoor and outdoor elemental mercury: A comparison of three different cases. Environ. Monit. Assess. 2017, 189.
- Darling, E.; Morrison, G.C.; Corsi, R.L. Passive removal materials for indoor ozone control. Build. Environ. 2016, 106, 33–44.
- Fadeyi, M.O. Ozone in indoor environments: Research progress in the past 15 years. Sustain. Cities Soc. 2015, 18, 78–94.
- Heal, M.R.; Kumar, P.; Harrison, R.M. Particles, air quality, policy and health. Chem. Soc. Rev. 2012, 41, 6606–6630.
- Irga, P.; Paull, N.; Abdo, P.; Torpy, F. An assessment of the atmospheric particle removal efficiency of an in-room botanical biofilter system. Build. Environ. 2017, 115, 281–290.
- Buczyńska, A.J.; Krata, A.; Van Grieken, R.; Brown, A.; Polezer, G.; De Wael, K.; Potgieter-Vermaak, S. Composition of PM2.5 and PM1 on high and low pollution event days and its relation to indoor air quality in a home for the elderly. Sci. Total Environ. 2014, 490, 134–143.
- Defra The Air Quality Strategy for England, Scotland, Wales and Northern Ireland; Department for Environment, Food and Rural Affairs, The Stationery Office: London, UK, 2007.
- Abd El Aziz, N.G.; Mahgoub, M.H.; Azza, M.M.M.; Farahat, M.M.; Abouziena, H.F. Potentiality of Ornamental Plants and Woody Trees as Phytoremidators of Pollutants in the Air: A Review. Int. J. Chemtech Res. 2015, 8, 468–482.
- Othman, M.; Latif, M.T.; Mohamed, A.F. The PM10 compositions, sources and health risks assessment in mechanically ventilated office buildings in an urban environment. Air Qual. Atmos. Health 2015, 9, 597–612.
- Bozlaker, A.; Peccia, J.; Chellam, S. Indoor/Outdoor Relationships and Anthropogenic Elemental Signatures in Airborne PM2.5 at a High School: Impacts of Petroleum Refining Emissions on Lanthanoid Enrichment. Environ. Sci. Technol. 2017, 51, 4851–4859.
- Mohammadyan, M.; Ghoochani, M.; Kloog, I.; Abdul-Wahab, S.A.; Yetilmezsoy, K.; Heibati, B.; Pollitt, K.J.G. Assessment of indoor and outdoor particulate air pollution at an urban background site in Iran. Environ. Monit. Assess. 2017, 189, 29.
- Kaur, A.; Misra, A. Impact of Indoor Surface Materials and Environment on Perceived Air Quality. J. Environ. Hum. 2014, 2014, 25–35.
- Mentese, S.; Mirici, N.A.; Otkun, M.T.; Bakar, C.; Palaz, E.; Tasdibi, D.; Cevizci, S.; Cotuker, O. Association between respiratory health and indoor air pollution exposure in Canakkale, Turkey. Build. Environ. 2015, 93, 72–83.
- De Gennaro, G.; Dambruoso, P.R.; Loiotile, A.D.; Di Gilio, A.; Giungato, P.; Tutino, M.; Marzocca, A.; Mazzone, A.; Palmisani, J.; Porcelli, F. Indoor air quality in schools. Environ. Chem. Lett. 2014, 12, 467–482.
- Sriprapat, W.; Suksabye, P.; Areephak, S.; Klantup, P.; Waraha, A.; Sawattan, A.; Thiravetyan, P. Uptake of toluene and ethylbenzene by plants: Removal of volatile indoor air contaminants. Ecotoxicol. Environ. Saf. 2014, 102, 147–151.
- Nielsen, G.D.; Larsen, S.T.; Wolkoff, P. Recent trend in risk assessment of formaldehyde exposures from indoor air. Arch. Toxicol. 2012, 87, 73–98.
- Nielsen, G.D.; Larsen, S.T.; Wolkoff, P. Re-evaluation of the WHO (2010) formaldehyde indoor air quality guideline for cancer risk assessment. Arch. Toxicol. 2016, 91, 35–61.
- Destaillats, H.; Maddalena, R.L.; Singer, B.C.; Hodgson, A.T.; McKone, T.E. Indoor pollutants emitted by office equipment: A review of reported data and information needs. Environ. Energy Technol. Div. 2007, 42, 1371–1388.
- ATSDR. Naphthalene, 1-Methylnapthalene, 2-Methylnapthalene; ATSDR: Atlanta, GA, USA, 2011.
- ATSDR. Trichloroethylene (TCE); ATSDR: Atlanta, GA, USA, 2011.
- Bahr, D.E.; Aldrich, T.E.; Seidu, D.; Brion, G.M.; Tollerud, D.J.; Muldoon, S.; Reinhart, N.; Youseefagha, A.; McKinney, P.; Hughes, T.; et al. Occupational exposure to trichloroethylene and cancer risk for workers at the Paducah Gaseous Diffusion Plant. Int. J. Occup. Med. Environ. Health 2011, 24, 67–77.
- Environmental Health and Medicine Education. Tetrachloroethylene Toxicity, What Are the Physiological Effects of Tetrachloroethylene Exposure? In Agency for Toxic Substances and Disease Registry; ATSDR: Atlanta, GA, USA, 2008.
- Ayoko, G.A.; Wang, H. Volatile Organic Compounds. In Indoor Environments; Pluschke, P., Schleibinger, H., Eds.; Springer: Berlin/Heidelberg, Germany, 2014; pp. 69–107.
- World Health Organization. Indoor Air Quality: Organic Pollutants. Report on a WHO Meeting, Berlin, Germany, 23–27 August 1987; EURO Reports and Studies 111; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 1989.
- WHO. Air Quality Guidelines for Europe, 2nd ed.; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2000.
- EPA. United States Environmental Protection Agency; EPA: Washington, DC, USA, 1971.
- Besis, A.; Samara, C. Polybrominated diphenyl ethers (PBDEs) in the indoor and outdoor environments—A review on occurrence and human exposure. Environ. Pollut. 2012, 169, 217–229.
- Darnerud, P.O.; Eriksen, G.S.; Jóhannesson, T.; Larsen, P.B.; Viluksela, M. Polybrominated diphenyl ethers: Occurrence, dietary exposure, and toxicology. Environ. Health Perspect. 2001, 109, 49–68.
- Hooper, K.; McDonald, T.A. The PBDEs: An emerging environmental challenge and another reason for breast-milk monitoring programs. Environ. Health Perspect. 2000, 108, 387–392.
- Gaspar, F.W.; Chevrier, J.; Bornman, R.; Crause, M.; Obida, M.; Barr, D.B.; Bradman, A.; Bouwman, H.; Eskenazi, B. Corrigendum to Undisturbed dust as a metric of long-term indoor insecticide exposure: Residential DDT contamination from indoor residual spraying and its association with serum levels in the VHEMBE cohort. Environ. Int. 2016, 94, 778–783.
- Sánchez, A.M.; Nuevo, M.J. Actions for remediation in cases with large concentration of radon indoor. J. Radioanal. Nucl. Chem. 2016, 311, 1219–1225.
- Al-Zoughool, M.; Krewski, D. Health effects of radon: A review of the literature. Int. J. Radiat. Biol. 2009, 85, 57–69.
- Jenkins, P.L.; Phillips, T.J.; Mulberg, E.J.; Hui, S.P. Activity patterns of Californians: Use of and proximity to indoor pollutant sources. Atmos. Environ. Part A Gen. Top. 1992, 26, 2141–2148.
- Bruce, N.; Perez-Padilla, R.; Albalak, R. Indoor air pollution in developing countries: A major environmental and public health challenge. Bull. World Health Organ. 2000, 78, 1078–1092.
- Ezzati, M. Indoor Air Pollution/Developing Countries; Elsevier Inc.: Amsterdam, The Netherlands, 2008; pp. 547–553.
- Smith, K.R.; Mehta, S.; Maeusezahl-Feuz, M. Indoor air pollution from household solid fuel use. In Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors; Ezzati, M., Ed.; World Health Organization: Geneva, Switzerland, 2004; pp. 1435–1493.
- Smith, K.R. Biofuels, Air Pollution, and Health: A Global Review; Plenum Press: New York, NY, USA, 1987.
This entry is offline, you can click here to edit this entry!
