Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Lipids are hydrophobic or amphiphilic small molecules, including fatty acids and their derivatives, in particular esters, sterols, steroids and phospholipids.
- insulin resistance
- type 2 diabetes
- natural product
1. Introduction
Insulin resistance (IR) is clinically defined as the inability of a known quantity of exogenous or endogenous insulin to increase glucose uptake and its utilization in an individual as much as it does in a normal population [1]. IR is associated with conditions beyond prediabetes and type 2 diabetes (T2D), including cardiovascular and metabolic pathologies, collectively referred to as a metabolic syndrome, nonalcoholic fatty liver disease, as well as atherosclerosis, hypertension, polycystic ovarian syndrome and infectious diseases with sepsis sequelae [2][3][4][5][6][7][8]. The cause of IR is poorly understood, but the major contributors are thought to comprise systemic chronic inflammation [9] associated with abnormal lipid levels, oxidative and endoplasmic reticulum stress, insulin receptor mutations and mitochondrial dysfunctions [10].
2. Lipids
Lipids are hydrophobic or amphiphilic small molecules, including fatty acids and their derivatives, in particular esters, sterols, steroids and phospholipids.
Azelaic acid (AZA) [11] and the best characterized azelate, diethyl azelate DEA [12], (Figure 1A) are both MAIMs. Yet, as can be expected from the large differences in respective water–octanol partitioning coefficients, the respective interactions of AZA and DEA with plasma membrane are quite different [13]. DEA is a membrane fluidizer that interacts with the plasma membrane and membrane proteins, while AZA, due to its lower lipophilicity, has limited membrane interactions [13][14].
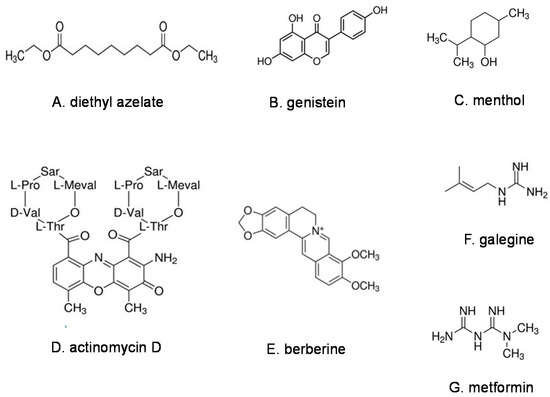
Figure 1. Representative natural products in the families of lipids (A), phenols (B), terpenes (C), antibiotics (D) and alkaloids (E–G).
AZA and azelates occur naturally in plants, animals and humans. Archaeological records provide evidence that even ancient humans consumed AZA and its esters in the form of grains, olives, soybeans, fermented foods and alcoholic beverages [13][14][15]. Endogenous AZA produced from longer chain carboxylic acids, mainly oleic acid, is present at micromolar levels in human cerebrospinal fluid, saliva and also in breast milk [13]. The levels of AZA and azelates in the body appear to increase in response to environmental insults [16] and fasting [17].
AZA and its esters act as immunomodulators in multicellular organisms. AZA primes plant systemic immunity after infection [18]. AZA modulates the innate immune responses in human skin and induces the expression of peroxisome proliferator-activated receptor gamma (PPARγ), a key regulator of inflammation, activated by fatty acids and products of lipid peroxidation [19]. DEA and related azelates exert immunomodulatory actions in vitro and in vivo [14]. DEA is a metabolic precursor of AZA, and is rapidly converted into AZA under physiological conditions [13].
Although DEA and AZA are pharmacologically distinct entities, they share some common effects in the mitigation of IR, albeit at quite different doses. Oral AZA administered to diabetic mice at 80 mg/kg over 11–15 weeks improved glucose tolerance and decreased plasma triglycerides, glucose and cholesterol plaque formation in the arteries [20]. In a human study in overweight adult males, daily oral DEA at 1 mg/kg over 3 weeks significantly reduced fasting glucose and insulin in subjects with IR and/or hemoglobin A1c (A1c) ≥ 5.6%, and improved diagnostic lipid ratios in all cases. The impact of DEA on biomarkers of disease correlated with the degree of IR [21]. These findings are in line with the physicochemical differences between AZA and DEA. Notably, sebacic acid [22], a C10 dicarboxylic acid, purportedly has some hypoglycemic effects [23], albeit at doses nearly 100 times higher than those achieved with DEA in humans [21].
Some effects of DEA and AZA on IR may be mediated by mitochondria. Mitochondrial dysfunction has been found to be associated with obesity-induced IR and T2D [24], while the enrichment of mitochondria in skeletal muscle was reported to lower the risk of T2D [25].
AZA was reported to bind to a murine olfactory receptor Olfr544 [26]. Olfactory receptors are G-protein-coupled plasma membrane receptors that constitute over 5% of the mammalian genome. Olfr544 is widely expressed in nonolfactory murine tissues, such as the small intestine, colon, adipose tissue, liver and skeletal muscle [17]. The activation of Olfr544 with AZA stimulated mitochondrial biogenesis in mouse skeletal muscle [27][28]. In vivo treatment with AZA increased insulin sensitivity and ketone body levels [17] and upregulated genes involved in insulin signal transduction [29]. It was proposed that AZA is a fasting signaling molecule that can activate Olfr544 in various tissues [17]. In the pancreas, AZA upregulated glucagon secretion through pancreatic islets [26]. In the gut, AZA’s activation of Olfr544 increased the secretion of an insulinotropic hormone glucagon-like peptide-1 (GLP-1) [30]. Since IR and T2D are associated with the impaired postprandial secretion of GLP-1 [31][32], the endogenous activity of AZA might be beneficial in these conditions. The putative human analogue of murine Olfr544 is encoded by the OR52K1 gene, but its function, like that of many other ectopically expressed olfactory receptors, is presently unknown.
Phospholipids are the main components of cell plasma membranes, and are also canonical MAIMs. Human studies have demonstrated the association between IR and the levels of the two most abundant phospholipids, phosphatidylcholine (PC) [33] and phosphatidylethanolamine (PE) [34][35]. Interestingly, the PC/PE ratio in skeletal muscle has been found to be elevated in T2D [36]. Abnormally high or low PC/PE ratios (and even small alterations thereof) influence the mitochondrial energy metabolism and have been linked to IR and metabolic syndrome [37][38]. A U-shaped dose response of phospholipids in the control of IR was reminiscent of the dose responsiveness of some MAIMs [15].
Other lipid MAIMs, such as n-3 and n-6 polyunsaturated fatty acids (PUFAs), represented by α-linoleic acid [39] and linoleic acid [40], respectively, affect membrane fluidity upon incorporation into phospholipids [41] or as free fatty acids. The dietary n-3 PUFA counteracted IR by modulating mitochondrial bioenergetics and decreasing endoplasmic reticulum stress [42]. Higher adipose tissue levels of α-linoleic acid have been inversely associated with IR in healthy adults [43]. Rats fed a high-fat diet enriched in n-3 and n-6 PUFAs developed hyperglycemia and hyperinsulinemia, consistent with IR. The expression of insulin receptors was significantly reduced in the liver, but not in the muscle, and the n-3 PUFA diet maintained normal GLUT-4 levels in the muscle [44]. Isomers of linoleic acids activated nuclear factor kappa-B (NFκB), elevated interleukin-6 (IL-6) and induced IR in human adipocytes [45].
Cholesterol [46] is the most common steroid in human physiology and a classical lipid MAIM. Cholesterol organizes and rigidifies plasma membranes [47] where cholesterol-enriched lipid rafts regulate protein diffusion and distribution [48]. An association between IR, increased cholesterol synthesis and decreased cholesterol absorption was reported in normoglycemic men [49] and subjects with metabolic syndrome [50]. Insulin sensitivity affected the cholesterol metabolism to a greater extent than obesity [51].
Cholesterol is a precursor of primary bile salts produced by the liver. The regulation of bile acid levels is linked to the lipid and glucose metabolism. Increased plasma levels of α-hydroxylated bile acids were found to be associated with IR [52], while bile acid sequestrants reduced glucose and cholesterol levels in T2D [53][54].
This entry is adapted from the peer-reviewed paper 10.3390/ph16070913
References
- Lebovitz, H.E. Insulin resistance: Definition and consequences. Exp. Clin. Endocrinol. Diabetes 2001, 109 (Suppl. S2), S135–S148.
- Kouzi, S.A.; Yang, S.; Nuzum, D.S.; Dirks-Naylor, A.J. Natural supplements for improving insulin sensitivity and glucose uptake in skeletal muscle. Front. Biosci. 2015, 7, 94–106.
- Bugianesi, E.; Moscatiello, S.; Ciaravella, M.F.; Marchesini, G. Insulin resistance in nonalcoholic fatty liver disease. Curr. Pharm. Des. 2010, 16, 1941–1951.
- Affinati, A.H.; Wallia, A.; Gianchandani, R.Y. Severe hyperglycemia and insulin resistance in patients with SARS-CoV-2 infection: A report of two cases. Clin. Diabetes Endocrinol. 2021, 7, 8.
- Acquah, S.; Boampong, J.N.; Eghan Jnr, B.A.; Eriksson, M. Evidence of insulin resistance in adult uncomplicated malaria: Result of a two-year prospective study. Malar. Res. Treat. 2014, 2014, 136148.
- Van Cromphaut, S.J.; Vanhorebeek, I.; Van den Berghe, G. Glucose metabolism and insulin resistance in sepsis. Curr. Pharm. Des. 2008, 14, 1887–1899.
- Niang, F.; Sarfo, F.S.; Frimpong, M.; Guenin-Mace, L.; Wansbrough-Jones, M.; Stinear, T.; Phillips, R.O.; Demangel, C. Metabolomic profiles delineate mycolactone signature in Buruli ulcer disease. Sci. Rep. 2015, 5, 17693.
- Phillips, R.O.; Sarfo, F.S.; Landier, J.; Oldenburg, R.; Frimpong, M.; Wansbrough-Jones, M.; Abass, K.; Thompson, W.; Forson, M.; Fontanet, A.; et al. Combined inflammatory and metabolic defects reflected by reduced serum protein levels in patients with Buruli ulcer disease. PLoS Negl. Trop. Dis. 2014, 8, e2786.
- Hansson, E.; Skioldebrand, E. Coupled cell networks are target cells of inflammation, which can spread between different body organs and develop into systemic chronic inflammation. J. Inflamm. 2015, 12, 44.
- Yaribeygi, H.; Farrokhi, F.R.; Butler, A.E.; Sahebkar, A. Insulin resistance: Review of the underlying molecular mechanisms. J. Cell Physiol. 2019, 234, 8152–8161.
- Azelaic acid. Available online: https://pubchem.ncbi.nlm.nih.gov/#query=azelaic%20acid (accessed on 5 June 2023).
- Diethyl azelate. Available online: https://pubchem.ncbi.nlm.nih.gov/#query=diethyl%20azelate (accessed on 5 June 2023).
- Izbicka, E.; Streeper, R. Azelaic Acid Esters as Pluripotent Immunomodulatory Molecules: Nutritional Supplements or Drugs? Nutraceuticals 2021, 1, 42–53.
- Izbicka, E.; Streeper, R.T.; Louden, C. Adaptive Membrane Fluidity Modulation: A Feedback Regulated Homeostatic System and Target for Pharmacological Intervention. In Vivo 2021, 35, 3073–3095.
- Izbicka, E.; Streeper, R.T. Adaptive Membrane Fluidity Modulation: A Feedback Regulated Homeostatic System Hiding in Plain Sight. In Vivo 2021, 35, 2991–3000.
- Matsubara, T.; Tanaka, N.; Krausz, K.W.; Manna, S.K.; Kang, D.W.; Anderson, E.R.; Luecke, H.; Patterson, A.D.; Shah, Y.M.; Gonzalez, F.J. Metabolomics identifies an inflammatory cascade involved in dioxin- and diet-induced steatohepatitis. Cell Metab. 2012, 16, 634–644.
- Wu, C.; Hwang, S.H.; Jia, Y.; Choi, J.; Kim, Y.J.; Choi, D.; Pathiraja, D.; Choi, I.G.; Koo, S.H.; Lee, S.J. Olfactory receptor 544 reduces adiposity by steering fuel preference toward fats. J. Clin. Investig. 2017, 127, 4118–4123.
- Jung, H.W.; Tschaplinski, T.J.; Wang, L.; Glazebrook, J.; Greenberg, J.T. Priming in systemic plant immunity. Science 2009, 324, 89–91.
- Mastrofrancesco, A.; Ottaviani, M.; Aspite, N.; Cardinali, G.; Izzo, E.; Graupe, K.; Zouboulis, C.C.; Camera, E.; Picardo, M. Azelaic acid modulates the inflammatory response in normal human keratinocytes through PPARgamma activation. Exp. Dermatol. 2010, 19, 813–820.
- Muthulakshmi, S.; Saravanan, R. Protective effects of azelaic acid against high-fat diet-induced oxidative stress in liver, kidney and heart of C57BL/6J mice. Mol. Cell Biochem. 2013, 377, 23–33.
- Streeper, R.T.; Louden, C.; Izbicka, E. Oral Azelaic Acid Ester Decreases Markers of Insulin Resistance in Overweight Human Male Subjects. In Vivo 2020, 34, 1173–1186.
- Sebacic acid. Available online: https://pubchem.ncbi.nlm.nih.gov/#query=sebacic%20acid (accessed on 5 June 2023).
- Iaconelli, A.; Gastaldelli, A.; Chiellini, C.; Gniuli, D.; Favuzzi, A.; Binnert, C.; Mace, K.; Mingrone, G. Effect of oral sebacic Acid on postprandial glycemia, insulinemia, and glucose rate of appearance in type 2 diabetes. Diabetes Care 2010, 33, 2327–2332.
- Montgomery, M.K.; Turner, N. Mitochondrial dysfunction and insulin resistance: An update. Endocr. Connect. 2015, 4, R1–R15.
- Russell, A.P.; Foletta, V.C.; Snow, R.J.; Wadley, G.D. Skeletal muscle mitochondria: A major player in exercise, health and disease. Biochim. Biophys. Acta 2014, 1840, 1276–1284.
- Kang, N.; Bahk, Y.Y.; Lee, N.; Jae, Y.; Cho, Y.H.; Ku, C.R.; Byun, Y.; Lee, E.J.; Kim, M.S.; Koo, J. Olfactory receptor Olfr544 responding to azelaic acid regulates glucagon secretion in alpha-cells of mouse pancreatic islets. Biochem. Biophys. Res. Commun. 2015, 460, 616–621.
- Thach, T.T.; Wu, C.; Hwang, K.Y.; Lee, S.J. Azelaic Acid Induces Mitochondrial Biogenesis in Skeletal Muscle by Activation of Olfactory Receptor 544. Front. Physiol. 2020, 11, 329.
- Thach, T.T.; Hong, Y.J.; Lee, S.; Lee, S.J. Molecular determinants of the olfactory receptor Olfr544 activation by azelaic acid. Biochem. Biophys. Res. Commun. 2017, 485, 241–248.
- Muthulakshmi, S.; Chakrabarti, A.K.; Mukherjee, S. Gene expression profile of high-fat diet-fed C57BL/6J mice: In search of potential role of azelaic acid. J. Physiol. Biochem. 2015, 71, 29–42.
- Wu, C.; Jeong, M.Y.; Kim, J.Y.; Lee, G.; Kim, J.S.; Cheong, Y.E.; Kang, H.; Cho, C.H.; Kim, J.; Park, M.K.; et al. Activation of ectopic olfactory receptor 544 induces GLP-1 secretion and regulates gut inflammation. Gut Microbes 2021, 13, 1987782.
- Nachawi, N.; Rao, P.P.; Makin, V. The role of GLP-1 receptor agonists in managing type 2 diabetes. Cleve. Clin. J. Med. 2022, 89, 457–464.
- Lim, G.E.; Huang, G.J.; Flora, N.; LeRoith, D.; Rhodes, C.J.; Brubaker, P.L. Insulin regulates glucagon-like peptide-1 secretion from the enteroendocrine L cell. Endocrinology 2009, 150, 580–591.
- Phosphatidylcholine. Available online: https://pubchem.ncbi.nlm.nih.gov/#query=phosphatidylcholine&sort=cid&page=1 (accessed on 5 June 2023).
- Phosphatidylethanolamine. Available online: https://pubchem.ncbi.nlm.nih.gov/#query=%22Phosphatidylethanolamine%20%5BWHO-DD%5D%22 (accessed on 5 June 2023).
- Zhao, J.; Zhu, Y.; Hyun, N.; Zeng, D.; Uppal, K.; Tran, V.T.; Yu, T.; Jones, D.; He, J.; Lee, E.T.; et al. Novel metabolic markers for the risk of diabetes development in American Indians. Diabetes Care 2015, 38, 220–227.
- Newsom, S.A.; Brozinick, J.T.; Kiseljak-Vassiliades, K.; Strauss, A.N.; Bacon, S.D.; Kerege, A.A.; Bui, H.H.; Sanders, P.; Siddall, P.; Wei, T.; et al. Skeletal muscle phosphatidylcholine and phosphatidylethanolamine are related to insulin sensitivity and respond to acute exercise in humans. J. Appl. Physiol. 2016, 120, 1355–1363.
- Van der Veen, J.N.; Kennelly, J.P.; Wan, S.; Vance, J.E.; Vance, D.E.; Jacobs, R.L. The critical role of phosphatidylcholine and phosphatidylethanolamine metabolism in health and disease. Biochim. Biophys. Acta Biomembr. 2017, 1859, 1558–1572.
- Chang, W.; Hatch, G.; Wang, Y.; Yu, F.; Wang, M. The relationship between phospholipids and insulin resistance: From clinical to experimental evidence. J. Cell. Mol. Med. 2019, 23, 702–710.
- Alpha linolenic acid. Available online: https://pubchem.ncbi.nlm.nih.gov/#query=%22alpha%20Linolenic%20Acid%22 (accessed on 5 June 2023).
- Linoleic acid. Available online: https://pubchem.ncbi.nlm.nih.gov/#query=linoleic%20acid (accessed on 5 June 2023).
- Calder, P.C. Polyunsaturated fatty acids and inflammatory processes: New twists in an old tale. Biochimie 2009, 91, 791–795.
- Lepretti, M.; Martucciello, S.; Burgos Aceves, M.A.; Putti, R.; Lionetti, L. Omega-3 Fatty Acids and Insulin Resistance: Focus on the Regulation of Mitochondria and Endoplasmic Reticulum Stress. Nutrients 2018, 10, 350.
- Heskey, C.E.; Jaceldo-Siegl, K.; Sabate, J.; Fraser, G.; Rajaram, S. Adipose tissue alpha-linolenic acid is inversely associated with insulin resistance in adults. Am. J. Clin. Nutr. 2016, 103, 1105–1110.
- Taouis, M.; Dagou, C.; Ster, C.; Durand, G.; Pinault, M.; Delarue, J. N-3 polyunsaturated fatty acids prevent the defect of insulin receptor signaling in muscle. Am. J. Physiol. Endocrinol. Metab. 2002, 282, E664–E671.
- Chung, S.; Brown, J.M.; Provo, J.N.; Hopkins, R.; McIntosh, M.K. Conjugated linoleic acid promotes human adipocyte insulin resistance through NFkappaB-dependent cytokine production. J. Biol. Chem. 2005, 280, 38445–38456.
- Cholesterol. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/5997 (accessed on 5 June 2023).
- Yeagle, P.L. Cholesterol and the cell membrane. Biochim. Biophys. Acta 1985, 822, 267–287.
- Owen, D.M.; Williamson, D.J.; Magenau, A.; Gaus, K. Sub-resolution lipid domains exist in the plasma membrane and regulate protein diffusion and distribution. Nat. Commun. 2012, 3, 1256.
- Pihlajamaki, J.; Gylling, H.; Miettinen, T.A.; Laakso, M. Insulin resistance is associated with increased cholesterol synthesis and decreased cholesterol absorption in normoglycemic men. J. Lipid Res. 2004, 45, 507–512.
- Hoenig, M.R.; Sellke, F.W. Insulin resistance is associated with increased cholesterol synthesis, decreased cholesterol absorption and enhanced lipid response to statin therapy. Atherosclerosis 2010, 211, 260–265.
- Gylling, H.; Hallikainen, M.; Pihlajamaki, J.; Simonen, P.; Kuusisto, J.; Laakso, M.; Miettinen, T.A. Insulin sensitivity regulates cholesterol metabolism to a greater extent than obesity: Lessons from the METSIM Study. J. Lipid Res. 2010, 51, 2422–2427.
- Haeusler, R.A.; Astiarraga, B.; Camastra, S.; Accili, D.; Ferrannini, E. Human insulin resistance is associated with increased plasma levels of 12alpha-hydroxylated bile acids. Diabetes 2013, 62, 4184–4191.
- Staels, B.; Kuipers, F. Bile acid sequestrants and the treatment of type 2 diabetes mellitus. Drugs 2007, 67, 1383–1392.
- Tomkin, G.H.; Owens, D. Obesity diabetes and the role of bile acids in metabolism. J. Transl. Int. Med. 2016, 4, 73–80.
This entry is offline, you can click here to edit this entry!
